The document provides an overview of gastrointestinal physiology, focusing on the functional structure, regulation, and processes of the gastrointestinal tract (GIT), including digestion, absorption, and excretion. Key roles of the GIT include maintaining homeostasis, fluid balance, and microbial defense, supported by an intricate nervous system that regulates motility and secretion. Additionally, it discusses the anatomy of the GIT and the electrical activities of smooth muscle that facilitate digestive movement.
![9/1/2023
General characteristics of the GIT
• When studying GI-physiology, it is important to
emphasize on the following facts.
1. Functional structure of the gut
2. Neural & hormonal innervations & regulation
3. Motility & propulsion of food along the tract
4. Blood flow regulation
5. Digestion, Secretion, absorption & excretory processes
6. Common diseases of the GIT
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-2-320.jpg)
![9/1/2023
Gastrointestinal System (GIS) Introduction
• Introduction to the GIS
I. The role of the GIS in Homeostasis
II. The role of the GIS in Fluid Balance
III. The role of the GIS in Microbial Defense
IV. The overall function of the GIS
3
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-3-320.jpg)
![9/1/2023
Role of GI-system in homeostasis
• Body cells require nutrients to obtain energy and
function optimally.
• The food has to be crushed into smaller units &
be available for utilization by cells.
• It is, therefore, the main role of the GIS to digest,
propel, absorb, and eliminate unwanted residues
out of the body.
• Thus, the GIT serves as one of the homeostatic
organs in maintaining the day-to-day balance of
food intake and excretion, thereby sustaining life.
4
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-4-320.jpg)
![9/1/2023
GIS and Fluid balance
A. Secretion:
~ 7 Liters of fluid is secreted
(added) from different
organs into the tract
~ 2 Liters of fluid is drunk
daily
~ 9 Liters of fluid added into
the Gut daily.
B. Absorption:
~ 8.5 Lit is absorbed by the SI
~ 400 ml is absorbed by the
LI
C. Excretion: only ~ 100
ml of fluid is excreted
5
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-5-320.jpg)
![9/1/2023
GIT & microbial defense
• The openness of GIT favors the entrance and thus
harboring of microorganisms (bacteria) in its luminal
surfaces.
• However, the GI-system can protect itself from such
hazards by some defense mechanisms found in:
a. Mouth: Saliva contains lysozymes etc
b. Stomach: HCl acid, Pepsin etc both have
bactericidal effects
c. Small intestine (e.g., Payer's patches):
Immuno- competent
lymph tissues
d. Macrophages: Located in SI walls attacks
bacteria (e.g., by
phagocytosis) 6
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-6-320.jpg)
![9/1/2023
(Cont…) GIT & it’s role in defense
7
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-7-320.jpg)
![9/1/2023
Overall function of the GIS
8
• The overall function of
the GIS includes:
1. Breaking of food
2. Transport (motility)
3. Secretion of
hormones
4. Absorption of
digested
substances
5. Excretion of waste
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-8-320.jpg)
![The basic principles of function in the entire alimentary tract
• The alimentary tract provides the body with a continual supply of water,
electrolytes, vitamins, and nutrients.
To achieve this requires:-
1) Movement of food through the alimentary tract
2) Secretion of digestive juices and digestion of the food;
3) Absorption of water, various electrolytes, vitamins, and digestive products;
4) Circulation of blood through the gastrointestinal organs to carry away the
absorbed substances; and
5) Control of all these functions by local, nervous, and hormonal systems.
• Each part is adapted to its specific functions: some to simple passage of
food, such as the esophagus others to temporary storage of food, such
as the stomach; and others to digestion and absorption, such as the
small intestine.
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-9-320.jpg)
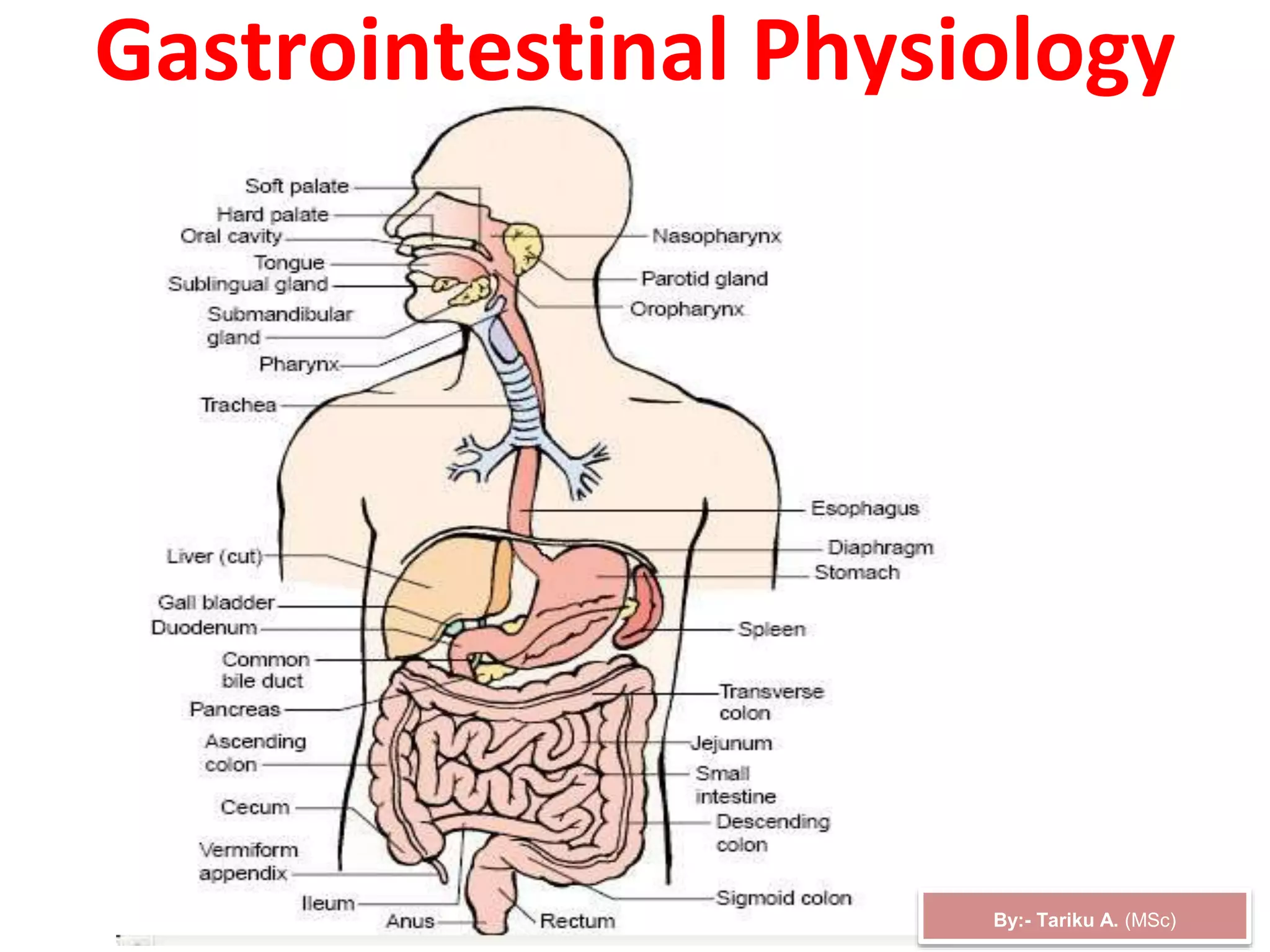
![9/1/2023
Structures of Digestive System
Organs involved in the process of digestion are:
Principal structures that make up the alimentary canal: – mouth,
pharynx, esophagus, stomach, small intestine, and large intestine
Accessory structures – teeth, tongue, gallbladder, salivary glands,
liver, and pancreas
Teeth aids mechanical breakdown of food
Tongue assists chewing and swallowing
Other accessory organs produce and send secretions to the GIT that
facilitate chemical breakdown of food
10
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-10-320.jpg)
![9/1/2023
I. Functional structures, Different Organs &
Accessories of the GI-System
11
1. Mouth
2. Pharynx
3. Esophagus
4. Stomach
5. Small intestine
6. Large intestine
7. Rectum
(Anus)
1. Salivary glands
2. Pancreas
3. Liver
4. Gallbladder
GI-Organs
Accessories
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-11-320.jpg)
![Physiologic Anatomy of the Gastrointestinal Wall
• A typical cross section of
the intestinal wall,
including the following
layers from outer surface
to inward:-
1) Serosa,
2) Longitudinal smooth
muscle layer,
3) Circular smooth muscle
layer
4) Submucosa, and
5) Mucosa.
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-12-320.jpg)
![9/1/2023
Histology of the GIT
epithelium – stratified squamous or simple
columnar
lamina propria – loose CT
muscuaris mucosa – smooth muscle
Mucosa
Submucosa
CT with BV’s,
nerves &
lymphatics
Muscularis externa
Skeletal muscle at beginning & end
of GIT, smooth muscle (inner
circular; outer longitudinal layer)
from lower esophagus to rectum
Serosa (a.k.a.
viseral
peritoneum)
4 -layers of tissue surround
the lumen of the GIT
13
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-13-320.jpg)
![9/1/2023
Organization of the wall of the intestine into functional layers
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-14-320.jpg)
![9/1/2023
Functions of the Mucosa and Sub-mucosa
1.The mucosa is divided into 3-sub-layers
a. Epithelium:
covers the mucosa and is columnar or stratified squamous cells.
b. Lamina propria: is under the epithelium and contains capillaries and
some lymph nodules necessary for immunological defenses
(e.g., Payers patches that produce B-lymphocytes).
C. Muscularies mucosa:
Located underneath the lamina. It is a thin layer of smooth
muscle and its contraction and relaxation changes the degree of
folding of the luminal diameter.
2. Sub-mucosa
- Is located beneath the mucosa
- Contains rich supply of blood vessels, nerves, lymph nodes, and
glands
- The submucosa also contains nerve plexuses of the Enteric nervous
system called Submucosa plexus or Meissiner’splexus .
15
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-15-320.jpg)
![9/1/2023
Function of Muscularis externa
3. Muscularies Externa (has 2-sublayers)
a. The circular layer (inner luminal side)
- Their contractions decrease the diameter of the lumen.
- At some regions, the circular SM thicken and forms a sphincter
that prevents backflow of food contents.
b. The outer longitudinal layer
- when it contracts, it decreases the length of the tract and cause
shortening and lengthening of the tract.
-The effect of both contractions help mix and propel the chyme in
aboral direction (i.e., towards the anus).
- Between the layers of the muscularis is a second plexus of
neurons—the myenteric plexus.
16
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-16-320.jpg)
![9/1/2023
(Cont… GIT) Function of the Serosa
4. Serosa
– Is an outermost layer consisting of connective tissues.
– It protects the underlying tissues and supplies blood
vessels, lymph and nerves to the gut wall.
– Its squamous epithelial cells secrete serous fluid that helps in
moistening & lubricating the tubes outer surface. This helps
the abdominal cavity to slide freely against one another, there by
decreasing friction.
17
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-17-320.jpg)
![9/1/2023 18
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-18-320.jpg)
![The GI Smooth Muscle Functions as a Syncytium
• The individual smooth muscle fibers are 200 to 500 micrometers in
length and 2 to 10 micrometers in diameter
• In the longitudinal muscle layer
- The bundles extend longitudinally down the intestinal tract
• In the circular muscle layer
- They extend around the gut.
• The muscle fibers are electrically connected with one another through
gap junctions
- Allow low-resistance movement of ions from one muscle cell to
the next.
• Each bundle of smooth muscle fibers is partly separated from the
next by loose connective tissue.
• Each muscle layer functions as a syncytium
- When an action potential is elicited anywhere within the muscle
mass,
it generally travels in all directions in the muscle.
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-19-320.jpg)

![• The cause of slow waves is poorly understood, but they
may
result from slow undulation of the activity of the sodium-
potassium pump or rhythmical changes in sodium
permeability.
• The slow waves usually do not by themselves cause
muscle contraction in most parts of the GIT, except perhaps
in the stomach. Instead, they mainly excite the appearance
of intermittent/ irregular spike potentials.
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-21-320.jpg)





![Neural Control of GI Function
1. Enteric Nervous System
• The GIT has its own nervous system called the enteric nervous
system.
• It lies entirely in the wall of the gut from esophagus & up to the anus.
• The number of neurons in enteric system is about 100 million,
almost exactly equal to the number in the entire spinal cord.
• Can function independently of the CNS
• The ENS is important in controlling motility and secretion of GI.
• The enteric nervous system is composed mainly of two plexuses
1) An outer plexus the myenteric plexus or Auerbach's plexus
2) An inner plexus the submucosal plexus or Meissner's
plexus
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-27-320.jpg)
![Cont…
The Myenteric Plexus consists mostly of a linear chain of many
interconnecting neurons that extends the entire length of the GIT.
• it lies between the longitudinal & circular muscle layers
• controls mainly the gastrointestinal movements
The Submucosal Plexus controls mainly gastrointestinal
secretion & local blood flow
• lies in the submucosa layers
• Although the ENS can function independently to that of the
extrinsic nervous system,
• stimulation by the parasympathetic and sympathetic systems
can greatly enhance or inhibit gastrointestinal functions.
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-28-320.jpg)
![Cont…
• Sensory nerve endings that originate in the gastrointestinal
epithelium or gut wall and send afferent fibers;
1. to both plexuses of the enteric system,
2. to the prevertebral ganglia of the sympathetic nervous
system,
3. to the spinal cord, &
4. in the vagus nerves all the way to the brain stem. (Figure next
slide)
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-29-320.jpg)
![1) Increased tonic contraction
2) Increased intensity of
rhythmical contractions
3) increased rate of contraction,
4) Increased velocity of
conduction of excitatory
waves along the gut wall
• But, some of its neurons are
inhibitory & release inhibitory
transmitter vasoactive
intestinal polypeptide (VIP)
• Useful for inhibiting some of
the intestinal sphincter muscles
9/1/2023 Tariku A. [GIT Physiology]
The Myenteric Plexus concerned mainly with controlling
muscle activity along the length of the gut
When stimulated, its principal effect are:-](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-30-320.jpg)
![Cont….
The Submucosal Plexus, help control
• Local intestinal secretion, local absorption,
& local contraction of
submucosal muscle.
Types of Neurotransmitters Secreted by
Enteric Neurons
• Ach, NE, serotonin, dopamine,
cholecystokinin, substance P, vasoactive
intestinal polypeptide, somatostatin,
adenosine triphosphate, leu-
enkephalin, met-enkephalin, and
bombesin.
• Acetylcholine most often excites
gastrointestinal activity.
• Norepinephrine and epinephrine almost
always inhibits gastrointestinal activity.
• The other aforementioned transmitter
substances are a mixture of excitatory and
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-31-320.jpg)
![Cont…
• The plexuses of the ENS consist of motor neurons, interneurons,
and sensory neurons
• Because the motor neurons of the myenteric plexus supply the
longitudinal and circular smooth muscle layers of the muscularis,
• This plexus mostly controls GI tract motility (movement),
particularly the frequency and strength of contraction of the
muscularis.
• The motor neurons of the submucosal plexus supply the secretory
cells of the mucosal epithelium, controlling the secretions of the
organs of the GI tract.
• The interneurons of the ENS interconnect the neurons of the
myenteric and submucosal plexuses.
• The sensory neurons of the ENS supply the mucosal epithelium.
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-32-320.jpg)
![• Some of these sensory neurons function as chemoreceptors
• Receptors that are activated by the presence of certain chemicals
in food located in the lumen of a GI organ.
• Other sensory neurons function as stretch receptors, receptors that
are activated when food distends (stretches) the wall of a GI organ.
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-33-320.jpg)
![34
2. Extrinsic neural control of GI function
Parasympathetic innervations to the gut
• Parasympathetic innervations to the gut is divided into cranial and
sacral division.
• The cranial parasympathetic are transmitted almost entirely in the
vagus nerves, providing extensive innervations to the esophagus,
stomach, pancreas, and first half of the large intestine (but rather
little innervations to the small intestine).
• The sacral parasympathetic originate in the 2nd, 3rd and 4th sacral
segments of spinal cord and pass through the pelvic nerves to the
distal half of the large intestine.
• The sigmoidal, rectal and anal regions are better supplied with
parasympathetic fibers. These fibers function in the defecation
reflexes.
• The postganglionic neurons of the PNS are located in the
myenteric and submucosal plexuses, and stimulation of PNS
causes a general increase in activity of the entire enteric NS,
enhancing GI function.
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-34-320.jpg)

![9/1/2023
Extrinsic neural control of (cont’d)
a. Parasympathetic : is
cholinergic (Ach)
- Excitatory and causes
constrictions of the gut.
- However, at the sphincters,
PNS is dilatatory in action
b. Sympathetic fibers
- are adrenergic and
inhibitory in action.
It causes dilatation of the
alimentary tract.
- at sphincters, it causes
constriction
36
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-36-320.jpg)
![Gastrointestinal Reflexes
Three types of reflexes are essential for GI control
1. Reflexes that occur entirely within the ENS.
This reflexes controls
– GI-secretion,
– Peristalsis & mixing contractions,
– Local inhibitory effects.
2. Reflexes that arise from the gut to the prevertebral sympathetic ganglia
and then back to the GIT.
– These reflexes transmit signals long distances to other areas of the GIT.
• Examples:
a) The gastro-colic reflex: signals send from the stomach
to cause evacuation of the colon.
b) The entero-gastric reflexes: signals from the colon & small intestine
to inhibit stomach motility and secretion.
c) The colono-ileal reflex: reflexes from the colon to inhibit
emptying of ileal contents into the colon.
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-37-320.jpg)
![3. Reflexes from the gut to the spinal cord or brain stem & then back
to GIT:
• These reflexes include especially:-
a) reflexes from the stomach & duodenum to the brain stem and
back to the stomach —by way of the vagus nerves— to control
gastric motor and secretory activity;
b) pain reflexes that cause general inhibition of the entire GIT; and
c) defecation reflexes that travel from the colon & rectum to the
spinal cord and back again to produce the powerful colonic, rectal,
and abdominal contractions required for defecation.
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-38-320.jpg)
![9/1/2023
Reflexes of the GIT cont..
Different GIT reflexes
1. Short localized reflexes (intrinsic)
- occurs within the Enteric NS and at
Ganglionic regions (Pre-vertbral
ganglion)
- cause tonic contractions, secretions etc
e.g., gastro-colic, entero-gastric, gastroileal,
etc
2. Long reflexes (both extrinsic and intrinsic )
- effected mainly by CNS and
parasympathetic (vagus) nerves
e.g., Defecation reflex
39
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-39-320.jpg)
![40
Neural Control of Gastrointestinal Function
Figure 23.4
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-40-320.jpg)
![9/1/2023
GASTROINTESTINAL HORMONES
• Hormones play a prominent role in the control of GI function, and in most cases
these hormones are secreted by the GI mucosa itself.
• GI hormones are peptides, most of which are also found as NTs in the ENS and
CNS, giving rise to the term gut-brain peptides.
• The release of hormones is influenced by the chemical environment in the lumen
of the GIT; enteroendocrine cells have microvilli-bearing receptors that “taste”
the gut lumen, allowing the cells to secrete hormone at the appropriate time.
• The timing of hormone secretion is also guided by “crosstalk” with the ENS.
• GI hormones are first secreted into the capillary blood in the GIT & must pass
through the portal venous system & liver before entering the systemic
circulation, a process known as first-pass metabolism.
• Several dozen substances are currently being investigated as possible GI
hormones, but only four have met all the criteria for true hormone
Gastrin
Cholecystokinin
Secretin
Gastric inhibitory polypeptide (GIP)
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-41-320.jpg)
![Gastrin
9/1/2023
• is secreted by the G-cells of the antrum, duodenum, and jejunum.
• In response to stimuli associated with ingestion of a meal such as:-
distention of the stomach, the products of proteins, the rate of discharge
of the vagus nerves (gastrin releasing peptide), and blood borne factors.
• Atropine does not inhibit the gastrin response to a test meal in humans,
b/se the transmitter secreted by the postganglionic vagal fibers that
innervate the G cells is gastrin-releasing polypeptide (GRP) rather than
acetylcholine.
• Which is released by the nerves of the gastric mucosa
• During vagal stimulation.
• The primary actions of gastrin are
1) stimulation of gastric acid & pepsin secretion and
2) stimulation of the growth of the mucosa of the stomach and
small & large intestines (trophic action).
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-42-320.jpg)
![Stimuli that affect gastrin secretion
Stimulatory factors
1. Luminal factors
• Amino acids in stomach
– Peptides & amino acids
(Phenylalanine & tryptophan)
are particularly effective.
• Distention of the stomach
2. Neural factors
• Vagus nerve (acetylcholine)
– Increased vagal discharge via GRP
3. Blood-borne factors
• Calcium,
Inhibitory factors
1. Luminal factors
• Acid (via a negative feedback
mechanism) [N.B. in pernicious anemia,
gastrin secretion is elevated].
• Somatostatin
2. Blood-borne factors
• Secretin, GIP,VIP, glucagon,
calcitonin
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-43-320.jpg)
![44
G
gastrin
circulation
HCl
vagus
nerve
FOOD
Distension
Peptides
2. Gastric Phase of
Gastric Secretion
(approx 60% of total)
(initiated by gastric events)
G
gastrin
circulation
HCl
vagus
nerve
1. Cephalic Phase of
Gastric Secretion (approx.
30% of total)
(initiated by brain)
Functional Phases of Gastric Secretion
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-44-320.jpg)
![9/1/2023 45
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-45-320.jpg)
![46
Cholecystokinin /CCK /
is secreted by “I” cells of the duodenum, jejunum, and ileum
The stimuli for secretion of CCK are the presence of partially-digested fats,
proteins, and acids in the lumen of the duodenum.
Stimulates the release of digestive enzymes from the pancreas, the
contraction of the gallbladder, and relaxation of the sphincter of Oddi,
which allows both bile and pancreatic juice to flow into the intestinal
lumen.
slows the emptying of food from the stomach to give adequate time for
digestion of the fats in the upper intestinal tract.
CCK augments the action of secretin in producing secretion of an alkaline
pancreatic juice.
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-46-320.jpg)
![9/1/2023
Motilin
Is secreted by the stomach and upper duodenum during fasting
is secreted by enterochromaffin cells & ‘M’ cells in the stomach, small
intestine, and colon.
The only known function of this hormone is to increase GI motility.
Motilin is released cyclically and stimulates waves of gastrointestinal
motility called interdigestive myoelectric complexes that move through the
stomach and small intestine every 90 minutes in a fasted person.
Motilin secretion is inhibited after ingestion by mechanisms that are not
fully understood
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-47-320.jpg)
![48
Cont…
Fig 15
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-48-320.jpg)
![9/1/2023
Secretin
• Was the first gastrointestinal hormone discovered
• Is secreted by the "S" cells in the mucosa of the duodenum in response to
the products of protein digestion & to acidic gastric juice emptying into the
duodenum
• It increases NaHCO3 secretion by the duct cells of the pancreas and biliary
tract; & other pancreatic secretions. It neutralizes the acid.
• Its action on pancreatic duct cells is mediated via cAMP.
• It also augments the action of CCK in producing pancreatic secretion of
digestive
enzymes.
• It decreases gastric acid secretion & may cause contraction of the pyloric
sphincter. Inhibits the motility of most of GIT.
GIP: Gastric inhibitory peptide
• Secreted by the ‘K’ cells in the mucosa of the upper small intestine in
response to fat and carbohydrate meal in the intestine.
• B/se in large doses it inhibits gastric secretion & motility, it was named gastric
inhibitory peptide.
• GIP stimulates insulin secretion and for this reason, it is also known as
glucose-dependent insulinotropic peptide.
49
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-49-320.jpg)
![9/1/2023
Somatostatin
the growth-hormone-inhibiting hormone originally isolated
from the hypothalamus,
is secreted as a paracrine by D-cells in the pancreatic
islets and by similar D-cells in the GI mucosa.
It exists in tissues in two forms, somatostatin 14 &
somatostatin 28, and both are secreted.
• Somatostatin inhibits the secretion of gastrin, VIP, GIP,
secretin, and motilin.
• Its secretion is stimulated by acid in the lumen, and it
probably acts in a paracrine fashion to mediate the inhibition
of gastrin secretion produced by acid.
• It also inhibits pancreatic exocrine secretion; gastric acid
secretion and motility; gallbladder contraction; and the
absorption of glucose, amino acids, and triglycerides.
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-50-320.jpg)
![51
Response to Acidity
Regulation by Secretin
HCl + NaHCO3 NaCl + CO2 + H2O
+
+
-
+
gall
bladder
liver
HCl
HCl
motility
NaCl
+ H2O
HCO3
HCl
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-51-320.jpg)
![9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-52-320.jpg)
![9/1/2023
Ghrelin is secreted primarily by the stomach and appears to play an
important role in the central control of food intake. It also stimulates
growth hormone secretion by acting directly on receptors in the pituitary.
The predominant source of circulating ghrelin is the GIT.
Primarily from the stomach but also in smaller amounts from the intestine.
At least two major biologic activates have been described to ghrelin:
Stimulation of growth hormone secretion
Regulation of energy balance
Ghrelin's activity in modulating feeding behavior and energy balance are
best explained by the presence of ghrelin receptors in areas of the
hypothalamus long known to be involved in appetite regulation.
Other effects of ghrelin include stimulating gastric emptying
Other GIT- hormones:-
• Glucagon (29aas) - substance-p
• Glucagon like peptides (GLP) - VIP (28 aas)
• Gastrin (17aa residues) - Opiates
• Somatostatin
• Metilin, met enkephalin
53
Ghrelin
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-53-320.jpg)

![9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-55-320.jpg)
![9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-56-320.jpg)
![Paracrine control
• Paracrine control is exerted when a hormone diffuses locally to affect target cells.
• Three major examples of paracrine mediators in GI physiology are serotonin,
somatostatin, and histamine.
1. Serotonin is produced by enterochromaffin (EC) cells in the intestinal mucosa in
response to distension of the gut wall. It exerts most of its effects indirectly
through interactions with the ENS. The effects of serotonin are generally
excitatory & result in increased intestinal motility & secretion.
2. Somatostatin is a peptide produced by D cells and is a potent inhibitor substance
in the GI system. It may be released both into the blood to act in an endocrine
fashion and also as a paracrine mediator. Somatostatin inhibits pancreatic and
gastric secretion, relaxes the stomach and gallbladder, and decreases nutrient
absorption in the small intestine. These actions result partly from inhibition of
several other stimulatory gut hormones, including gastrin, secretin, gastric
inhibitory peptide (GIP), and motilin.
3. Local release of histamine in the stomach has a potent stimulatory effect on acid
secretion. Enterochromaffin-like (ECL) cells are the source of histamine released
as a paracrine mediator in the stomach.
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-57-320.jpg)
![Functional Movements in the GIT
• Two types of movements occur in the GIT:
1) Propulsive movements 2) Mixing movements
Propulsive Movements-Peristalsis
• The basic propulsive movement of the GIT is peristalsis.
• Distention of the intestinal tract causes a contractile ring to appear
around the gut, which moves anal ward a few centimeters before
ending.
• At the same time, the gut sometimes relaxes several centimeters
down toward the anus, which is called receptive relaxation, allowing
the food to be propelled more easily toward the anus.
• This complex pattern does not occur in the absence of the myenteric
plexus; therefore the complex is called the myenteric reflex, or
peristaltic reflex.
• The peristaltic reflex plus the direction of movement toward the anus
is called the law of the gut.
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-58-320.jpg)
![Cont…
• Directional movement of
peristaltic waves toward the anus
• The “law of the gut” movement
always occurs from mouth- to-
anus unless pathological
• A peristaltic motion consists of a
progressive wave of strong
contraction preceded by
relaxation.
• This phenomena of relaxation
where the muscular walls ahead
of the ring relaxes is called
receptive relaxation.
• Peristalsis produces audible
sounds (bowel sounds).
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-59-320.jpg)
![9/1/2023 Tariku A. [GIT Physiology]
• Figure shows Peristalsis
1. A wave of circular smooth muscle relaxation moves ahead of the bolus of food
or chyme allowing the digestive tract to expand.
2. A wave of contraction of the circular smooth muscles behind the bolus of food
or chyme propels it through the digestive tract.](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-60-320.jpg)
![Cont…
Mixing:
• occurs due to local
contractions taking
place in small
segments.
• It chops, shakes, and
thereby mixes food
with digestive juices.
• Provides increase in
surface area for
mixing of digestive
juices with the chyme
(stomach, small and
large intestine).
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-61-320.jpg)
![62
Blood Supply to Digestive System
• The blood vessels of the GI-system are part of a more extensive
system called the splanchnic circulation.
• Includes blood flow through the GIT plus through the spleen,
pancreas and the liver.
• All of the blood that flows through the gut, spleen & pancreas then
passes into the liver by way of the portal vein.
• The non-fat, water-soluble nutrients absorbed from the gut (such as
carbohydrates and proteins) are transported in the portal venous
blood to the same liver sinusoids
• Leaves the liver by way of the hepatic veins that empty into the
inferior vena cava of the general circulation.
• The advantage is the reticuloendothelial cells in the liver remove bacteria
and other particles entering the blood from the GIT & preventing pathogens
• Almost all of the fats absorbed from the intestinal tract are not carried in the
portal blood
• Instead absorbed into the intestinal lymphatics and then conducted to the
systemic circulating blood by way of the. thoracic duct, bypassing the
liver
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-62-320.jpg)
![Blood Supply to GIT (cont’d)
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-63-320.jpg)

![Factors that control blood flow to the GIT
1. Local metabolic factors (vasoactive substances)
2. Neural factors
• Local metabolic factors
– GI-BF usually is proportional to the level of local activity.
– For instance, during active absorption of nutrients, BF in the villi and adjacent
regions of the submucosa is greatly increased. Likewise, BF in the muscle
layers of the intestinal wall is greater with increased motor activity in the gut.
– Although the precise cause or causes of increased BF during increased GI
activity are still unclear, some facts are known.
a) Vasodilator substances are released from the mucosa during the digestive
process.
– Most of them are peptide hormones, including cholecystokinin, gastrin, and
secretin. Some of the GI glands also release two kinins, kallidin & bradykinin,
into the gut wall. These kinins are powerful vasodilators.
– An increase in local metabolic activity also, enhances O2-utilisation by
tissues.
9/1/2023 Tariku A. [GIT Physiology]
(Cont…) blood flow of the GIT](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-65-320.jpg)
![• vasoactive substance
– The release of vasodilator GI hormones during
digestive processes.
– These include CCk, VIP, gastrin, secretin, bradykinin,
nitric oxide.
Local factors affecting blood flow to the gut
• O2 concentration.
• metabolic products
• Metabolic demand
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-66-320.jpg)
![Propulsion and Mixing of Food in the Alimentary Tract
• The amount of food that a person ingests is determined
principally by intrinsic desire for food called hunger.
Mastication (Chewing)
• The teeth are admirably designed for chewing
• Most of the muscles of chewing are innervated by the motor
branch of the fifth cranial nerve
• The chewing process is controlled by nuclei in the brain stem.
• Chewing is important for digestion of all foods especially for
most fruits and raw vegetables.
• Aids the digestion of food by increasing surface area for
enzymatic reaction
• Grinding the food prevents excoriation of the GIT.
• Increases the ease with which food is emptied from the
stomach into the small intestine
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-67-320.jpg)
![9/1/2023
(Cont…) The Mouth
• The mouth (oral cavity) is
responsible for mechanical
digestion of solid food by
mastication. Mastication
helps mix food with saliva.
Parts of the oral cavity:
- The cheeks, the lips
- The tongue
- The hard and soft palate
- The teeth
- Saliva is released into the
oral cavity
68
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-68-320.jpg)
![9/1/2023
(Cont…) The Mouth in digestion
• The mouth (oral cavity) is responsible for mechanical
digestion of solid food by mastication.
• In the oral cavity begins mastication of food that involves
breaking & mixing of food with saliva.
The different organs of the mouth include:
a. The Cheeks:
• Cheeks are lateral walls that include skin, elastic skeletal
muscles, and subcutaneous fats.
• The cheeks can hold relatively greater volume of food because
of its elasticity.
b. Lips:
• skeletal muscles and sensory receptors that are useful in
judging the temperature, texture or shape of the food.
• Is usually red in color (due to many blood vessels near their
surfaces).
69
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-69-320.jpg)
![9/1/2023
(Cont.) Mouth (oral cavity)
c. Teeth:
• Grinds into smaller peaces;
• Increases surface area for digestive enzymes react more
effectively.
• Incisors (cutting), Canines (tearing), Premolars & Molars
(crushing and grinding, respectively).
• There are two sets of teeth:
1. Primary/deciduous
2. Permanent
• Primary – 20 deciduous teeth that erupt at intervals between
6 and 24 months
• Permanent – enlarge and develop causing the root of
deciduous teeth to be resorbed and fall out between the ages
of 6 and 12 years
• All, but the third molars have erupted by the end of
adolescence
• Usually there are 32 permanent teeth 70
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-70-320.jpg)
![9/1/2023 71
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-71-320.jpg)
![72
Dental Formula: Permanent Teeth
• A shorthand way of indicating the number and relative
position of teeth
• Written as ratio of upper to lower teeth
• Deciduous: 2I (incisors), 1C (canine), 2M (molars) = 20
• Permanent: 2I, 1C, 2PM (premolars), 3M =32
2I 1C 2PM 3M X 2 =(32 teeth)
2I 1C 2PM 3M
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-72-320.jpg)
![9/1/2023
(Cont.) Mouth or oral cavity
d. Tongue: connected to the flour of the mouth.
• Is a thick mass of voluntary skeletal muscle that shows a high
degree of movement in every angle.
• Mucous membranes are important for lubrication.
• The papillae are projections of the tongue and contain test
buds.
• The tongue mixes food with saliva & pushes food towards the
pharynx.
e. Palate: (the hard & soft palate):
• During swallowing, it moves upwards & closes the nasal
cavity to prevent food from entering.
73
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-73-320.jpg)
![9/1/2023
(Cont…) Saliva, functions
a. Digestion:
- CHO-digestion begins in saliva .
- The enzyme ptyalin breaks starch- to-maltose.
- Lingual lipase begins fat digestion in the mouth.
b. Protection:
- Has anti-microbial actions (contains Lysozyme &
thiocyanate that kills microbes).
c. Speech:
- Clear & fluent articulation is possible in the presence of
saliva.
d. Secretes HCO3
- :
- Good to maintains the pH to neutral range (6-to-7), the
neutral pH is good for ptyalin action.
e. Lubrication:
- Muncin found in saliva facilitates moistening and
swallowing of food.
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-74-320.jpg)
![9/1/2023
(Cont …) Types of Salivary glands and their secretions
a. Parotid 25%:
- Secrete mainly serous
watery fluid rich in ptyalin.
b. Submandibular 70%:
- Produce both serous and
mucous fluid.
c. Sublingual ~5%:
- Secrete mainly thick
mucous with little serous
fluid
75
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-75-320.jpg)
![9/1/2023
(Cont…), Constituents of saliva
Constituents of saliva
A. H2O (99.5%):
B. Electrolytes ( 0.5%): Na+,
Cl-, K+, HCO3- Mg, Iodine,
etc.
C. Other organic substances
include:
Enzymes (amylase), lingual
lipases, Lysozymes,
thiocyanate, Glycoproteins,
(albumin, globulin), IgA,
mucus, etc.)
(Total secretion = about
1-1.5 L/day)
76
• Saliva contains 2-types
protein secretions
1. Serous secretion:
– Secretion that
contains mainly the
enzyme alpha-amylase
(begins digestion of
starch to
disaccharides)
2. Mucous secretion:
– Secretion that
contains a protein
mucin that helps for
lubrication & surface
protection.
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-76-320.jpg)
![9/1/2023
(Cont…) Mechanisms of salivary secretion
A. Clusters of cells called
acini that produce the
primary secretion
containing electrolytes,
enzymes, proteins etc.
that is essentially identical
in its composition to
plasma. (i.e. isotonic).
B. The primary secretion
are modified by active
absorption of (Na+) and
passive absorption of (Cl-
) ions. K+ and HCO3-
are secreted into the
lumen as they pass
through the ducts
causing secondary
hypotonic secretions
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-77-320.jpg)
![9/1/2023
(Cont…) Salivary secretions
Reasons for hyptonicity
of the saliva, includes:
1. Na+ and Cl-
reabsorption from the
lumen to the plasma is
greater than K+ and
HCO3- secretion into
the lumen
2. The ducts are relatively
impermeable to water
(i.e. H2O does not
follow the osmotic
gradient of NaCl)
78
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-78-320.jpg)
![9/1/2023
(Cont.) Salivary secretion
Reflex control of salivation: (Nervous control)
Sight, smell, and taste or thinking of food Receptors in oral
cavity or smell Sensory fibers from the tongue to the nuclei
in brain stem (MO), so called Salivatory nuclei
Parasympathetic fibers act on salivary glands to increase
copious salivary secretion.
* Salivation can also be controlled by higher centers like
hypothalamus which has nerve connections with salivatory
nuclei in the Medulla oblongata (MO)
* Higher centers like appetite area in the hypothalamus are also
involved in reflex control.
79
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-79-320.jpg)
![9/1/2023
(Cont…) Reflex secretion of saliva
Salivary innervations are:
mainly autonomic
A. Parasympathetic fibers:
causes copious secretion
of saliva (Cholinergic).
B. Sympathetics: Causes
small and insignificant
secretion which is viscous
(Adrenergic).
Interrupting sympathetic
fibers do not greatly affect
salivary secretions, but
parasympathetic
denervation causes
atrophy of the gland.
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-80-320.jpg)


![9/1/2023
(Cont…) Phases of Salivary secretions
3-phases of salivary secretions include
1. Cephalic (brain) phase: triggered by
thought, smell, or sight of food
2. Oral phase: triggered by food that
stimulate touch & taste receptors in the
mouth
3. Gastric phase: triggered by substances
which stimulate the gastric mucosa (acids
or sour tastes) in the stomach.
83
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-83-320.jpg)


![9/1/2023
(Cont.) Swallowing reflex
3. Esophageal phase (involuntary):
- The esophagus functions primarily to conduct food rapidly from
the pharynx to the stomach
- The esophagus normally exhibits two types of peristaltic
movements:
primary peristalsis and secondary peristalsis.
- Primary peristalsis begins in the pharynx and spreads into the
esophagus during the pharyngeal stage of swallowing.
- This wave passes all the way from the pharynx to the stomach
in about 8 to 10 seconds
- If the primary peristaltic contraction is not adequate to push the
bolus, then distention of the esophageal walls cause the so
called “secondary peristalsis” that is modified by enteric
nerves and strong enough to push the bolus to the stomach.
Secretion of the esophagus
Mucous glands that surround the esophagus secrete mucus that
provide lubrication and protection from gastric digestion (HCl)
that may arise from reflux of stomach contents.
86
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-86-320.jpg)
![9/1/2023
(Cont…) Swallowing reflex, Esophagus
1. Voluntary phase:–
- The bolus is pushed by tongue
towards the pharynx
2. Pharyngeal phase:
- Cause of primary peristalsis.
- The musculature of the
pharyngeal wall and upper 1/3 of the
esophagus is striated muscle.
- Therefore, the peristaltic waves in
these regions are controlled by
skeletal nerve impulses from the
glossopharyngeal and vagus nerves
3. Esophageal phase (involuntary)
- Distention of the esophageal walls
causes the so called “secondary
peristalsis” (10 sec)
- In the lower 2/3 of the esophagus,
the musculature is smooth muscle
- Controlled by the vagus nerves
acting through connections with
myenteric nervous system.
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-87-320.jpg)
![The lower esophageal sphincter (LES)
• The LES opens at the start of deglutition due to a vagovagal reflex
(receptive relaxation) mediated by VIP- & NO-releasing neurons.
– Otherwise, the LES remains closed to prevent the reflux of aggressive gastric
juices containing pepsin & HCl.
• Esophageal motility is usually checked by measuring pressure in
the lumen, e.g., during a peristaltic wave.
– The resting pressure within the LES is normally 20–25 mmHg.
– During receptive relaxation, esophageal pressure drops to match the
low pressure in the proximal stomach, indicating opening of the sphincter.
In achalasia, receptive relaxation fails to occur & food collects in
the esophagus.
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-88-320.jpg)
![• If the pressure in the LES is decreased, it causes a reflux from the
stomach to the esophagus.
– E.g. by VIP, CCK, NO, GIP, secretin & progesterone.
• Pressure in the LES is increased by,
– Ach, gastrin & motilin.
– Increased abdominal pressure (external pressure) also increases sphincter
pressure b/se part of the lower esophageal sphincter is located in the
abdominal cavity.
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-89-320.jpg)

![91
Functional structure of the stomach
The stomach has the following regions:
Cardia region: surrounds the cardiac orifice
Fundus: dome-shaped region beneath the diaphragm
Body: midportion of the stomach
Pyloric region: made up of the antrum and canal
which terminates at the pylorus
• The pylorus is continuous with the duodenum through the
pyloric sphincter
• Anatomically, the stomach is usually divided into
two major parts:
1) the body and 2) the antrum.
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-91-320.jpg)
![9/1/2023 92
Function
1. Storage (1-1.5 Liter)
2. Mixing (soupy chyme)
3. Secretion of intrinsic
factor and other
enzymes
4. Protein digestion
5. Has antiseptic actions
(HCl) etc
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-92-320.jpg)


![9/1/2023
(Cont…) Production of gastric juices in stomach
Cells Secretions
1. Parietal cells HCl + IF (intrinsic factor)
2. Chief cells Pepsinogen (stimulated by HCl)
3. Mucous cells: Mucous
4. G-cells: Gastrin (at pyloric antrum)
5. D-cells Somatostatin
6. H-cells Histamine
7. Water 99% liquefies the food
Enterochromaffin-like cells (ECL cells)-
Histamine
95
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-95-320.jpg)
![9/1/2023
(Cont…) Phases of gastric juice secretion
• 3-phases of gastric juice secretion include:
A. Cephalic B. Gastric & C. Intestinal
phases
The cephalic (~15%) (neural):
• Afferent impulses from taste, smell, sight, or thought of
food are carried to MO that causes reflex stimulation of the
stomach to secrete gastric juices.
• 2-ways of increasing gastric secretion:
a. The transmitter (Ach) released from Vagal nerve acts
on parietal and chief cells to secrete (HCl + intrinsic
factor) & pepsinogen, respectively.
b. Mechanical stimulation + protein foods directly
stimulates G-cells to release the hormone gastrin
and indirectly HCl
96
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-96-320.jpg)

![9/1/2023
(Cont…) Regulation of gastric secretion
2. The gastric phase (~70%)
• When food distends the stomach, mechanoreceptors &
chemoreceptor are activated by products of food.
• Sensory information from the receptors pass to the brain stem
(MO).
• Reflex Vagal stimulation on the stomach causes increased gastric
secretions through Ach .
Different mechanisms of gastric release include:
a. Local reflex: stretch causes the enteric nerves to increase gastric
acid secretion
b. Mechanical distention: directly stimulates G-cells in the antrum to
increase HCl release
c. Presence of amino acids, dipeptides, alcohol, coffee: stimulate
histamine
(H-cells), parietal and G-cells that release HCl and other gastric
juices in
the stomach. 98
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-98-320.jpg)
![9/1/2023 Tariku A. [GIT Physiology]
• 70% of acid
response
• Distension
• Peptides
• Calcium
• Alcohol
• Caffeine
Gastric phase……](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-99-320.jpg)
![9/1/2023 Tariku A. [GIT Physiology]
Acetylcholine
Gastrin Cell
Somatostatin
Cell
-
Regulation of gastrin release……](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-100-320.jpg)

![9/1/2023
(Cont…) Gastric secretion, intestinal phase
3. The intestinal phase (~5%)
- This stage begins when chyme reaches the duodenum.
- This phase is mostly inhibitory to gastric juice secretion.
- When fatty chyme, amino acids etc. reach the duodenum, they
cause secretion of hormones like Secretin, CCK, GIP that
reflexly inhibit gastric secretion in the stomach.
- In small cases, however, this phase causes secretion of
gastric juice b/se of the presence of G-cells in the duodenum.
- G- cells release gastrin that stimulates gastric secretion
reflexly.
102
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-102-320.jpg)

![9/1/2023 104
Phases of gastric juice secretion in the stomach
Cephalic, gastric, and intestinal phases.
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-104-320.jpg)

![9/1/2023
(cont…) Stomach secretions
The following are general factors that decrease gastric
secretion:
1. Low pH: Decreases gastric motility
2. Enterogastric reflex: Deceases Vagal output of the
stomach and thus decreases motility of the stomach
3. CCK: stimulated by fat diet in the duodenum
decreases stomach motility reflexly.
106
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-106-320.jpg)
![9/1/2023
(Cont…), HCl secretion by Parietal cells
1. H+ ions that result from the dissociation of H20 in the
cytoplasm of the parietal cells are continuously pumped
(actively) through the membrane of the gland (canaliculi)
into the gland lumen (pit).
2. Within the cell cytoplasm (intracellular), CO2 and OH-
combine to produce bicarbonate ions HCO3-.
3. Cl- ions are transported from the blood into the parietal cell
and finally into the lumen (pit) of the gland by facilitated
diffusion.
4. HCO3
- in exchange to Cl- is transported in reverse direction
(from the cytoplasm into the blood, charge balance).
5. Finally, H+ and Cl- ions combine in the lumen of the gland
(pit) and produce HCl that is collected and stored in the pit
until used for different physiological functions.
107
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-107-320.jpg)
![9/1/2023 108
Tariku A. [GIT Physiology]
Secretion of HCl by parietal cells](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-108-320.jpg)



![9/1/2023
Cont…
• These slow waves are conducted through gap junctions along the
stomach’s longitudinal muscle layer and also induce similar slow
waves in the over lying circular muscle layer.
• In the absence of neural or hormonal input, however, these
depolarization are too small to cause significant contractions.
• Action potentials may be generated at the peak of the slow wave cycle
if threshold is reached .
• The number of spikes fired with each wave determines the strength of
the muscle contraction.
• whereas the frequency of contraction is determined by the intrinsic
basic electrical rhythm and remains essentially constant.
• The initiation of these reflexes depends upon the contents of both the
stomach and small intestine.
112
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-112-320.jpg)
![9/1/2023
(Cont…) Gastric motility, Orad (fundus and body) and
caudad (antrum) regions
113
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-113-320.jpg)

![(Cont…) Emptying of the stomach (Neural)
- Stomach emptying is promoted by intense peristaltic contractions in
the stomach antrum.
- At the same time, emptying is opposed by varying degrees of
resistance to passage of chyme at the pylorus.
- Increased food volume in the stomach promotes increased
emptying from the stomach
- The rate at which the stomach empties depends on the fluidity of
the chyme and its contents.
- Thus, liquids empty faster than solids (fast CHO> protein> Slow
fat).
Factors that affect emptying include neural & hormonal:
1. Neural factors that affect emptying:
- The rate at which the stomach empties is regulated by signals from both the
stomach and the duodenum.
a. Parasympathetic: Causes increase rate of emptying by opening the
pyloric sphincter (dilatation)
b. Sympathetic: Increases constriction of the pyloric sphincter through
its Adrenergic receptors, thus it has the effect of delaying emptying
(constriction)
c. Enterogastric reflex: When fat or protein chyme reaches the
duodenum, receptors detect and send impulses to enteric nerves of the
stomach that in turn cause the inhibition of stomacheal motility and
secretion. This reflex, therefore, delays emptying.
115
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-115-320.jpg)
![Powerful Duodenal Factors That Inhibit Stomach Emptying
• When food enters the duodenum, multiple nervous reflexes are
initiated from the duodenal wall.
• They pass back to the stomach to slow or even stop stomach
emptying if the volume of chyme in the duodenum becomes too
much.
• These reflexes are mediated by three routes:
• 1) directly from the duodenum to the stomach through the ENS
in the gut wall, (Local reflex)
• 2) through extrinsic nerves that go to the prevertebral
sympathetic ganglia and then back through inhibitory
sympathetic nerve fibers to the stomach (Enterogastric reflex)
• 3) probably to a slight extent through the vagus nerves all the
way to the brain stem
• All these parallel reflexes have two effects on stomach
emptying:
1. they strongly inhibit the "pyloric pump" propulsive
contractions,
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-116-320.jpg)
![Cont…
• The types of factors that continually monitored in the
duodenum and initiate enterogastric inhibitory reflexes
include the following:
- The degree of distention of the duodenum
- The presence of any degree of irritation of the
duodenal mucosa
- The degree of acidity of the duodenal chyme
- The degree of osmolality of the chyme
- The presence of certain breakdown products in the
chyme, especially breakdown products of proteins
and, perhaps to a lesser extent, of fats
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-117-320.jpg)
![(Cont…) Stomach emptying, hormonal
2. Hormonal factors
- Gastrin is stimulatory to gastric emptying on the stomach wall Hormone
from the Duodenum Inhibits Gastric Emptying
CCK (cholecystokinin)
- Potent, stimulated by fat chyme
- Released from the mucosa of the jejunum
- Acts as an inhibitor to block increased stomach motility caused by gastrin
Secretin
- Is released mainly from the duodenal mucosa
- stimulated by high acid (HCl)
GIP (gastric inhibitory polypeptide)
- GIP is released from the upper small intestine
- Stimulated by fat & lesser extent to carbohydrates
- Inhibits gastric motility under some conditions
- Main effect stimulate secretion of insulin by the pancreas.
- Also called glucose-dependent insulinotropic peptide
118
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-118-320.jpg)
![Cont…
General Mechanism of hormonal control
a. The hormones after being secreted pass through the blood
and reach the stomach, where they inhibit stomach motility
and secretion.
b. They also cause constriction of the pyloric sphincters
thereby delaying emptying.
Summary of Gastric emptying
- Emptying of the stomach is controlled only to a moderate degree by
stomach factors such as the degree of filling in the stomach and the
excitatory effect of gastrin on stomach peristalsis.
a. Rate of emptying is fastest when stomach contents are isotonic, others
slow emptying (hypotonic or hypertonic fluids) especially hypertonic elicit
the inhibitory reflexes
b. Fat food slow emptying, the hormone CCK is the mediator
c. Low pH or increased H+ (acidity) in the duodenum delay or inhibit
emptying. The hormone Secretin can be the mediator because its
secretion is stimulated by increased H+ level in duodenum.
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-119-320.jpg)
![120
Hormonal and neural factors that regulate
stomach emptying
Stimulatory stomach factors
Distension of the stomach
Partially digested protein
Distension
Alcohol,Caffeine
↑Gastrin
Sensory
Secretion impulse via vagus
-Constrict LES
-↑Stomach motility
-Relax pyloric sphincter
Stimulate gastric emptying
Inhibitory duodenal factors
Distension of the duodenum
Fatty acids and glucose
Partially digested protein
↑Secretion of
CCK Entero-gastric reflex
GIP
Secretin
↓Stomuch motility
↑Pyloric sphincter tone
Inhibit gastric emptying
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-120-320.jpg)
![9/1/2023
(Cont…) Gastric emptying
Physiological advantage of delaying stomacheal
contents
1. It gives ample time for nutrients (e.g., like fat) to remain
longer in the stomach and be digested by gastric juices.
2. The delay prevents acids (HCl) not to be damped into
the duodenum at higher rates to cause duodenal ulcers.
3. The delay also gives time for pancreatic secretions
to reach duodenum and neutralize the acid.
• Rough estimates of transit times in healthy humans following
ingestion of a standard meal.
• Variability among individuals can exist.
Time
• A. 50% of stomach contents emptied 2.5 to 3 hr
• B. Total emptying of the stomach 4 to 5 hr
• C. 50% emptying of the SI 2.5 to 3 hr
• D. Transit through the colon 30 to 40 hr
121
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-121-320.jpg)
![9/1/2023
(Cont…) Absorption from the stomach
• The stomach is a poor absorptive area of the GIT.
• Because it lacks the typical villus type of absorptive
membrane
• Also because the junctions between the epithelial cells
are tight junctions.
• Only a few highly lipid-soluble substances, such as
alcohol and some drugs like aspirin, can be absorbed
in small quantities
• Organic nutrients (glucose, amino acids, and FFA etc.
are not usually absorbed from the stomach.
122
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-122-320.jpg)


![9/1/2023
(Cont…) Pancreas, Function
• Pancreatic juice is secreted most abundantly in response to the
presence of chyme in the upper portions of the small intestine.
The bulk of the pancreas by volume consists of exocrine cells that secrete
an alkaline solution of digestive enzymes. This secretion moves through a
duct system that eventually leads to the pancreatic duct.
Only about 5% of the volume of the pancreas consists of endocrine cells.
These cells secrete peptide hormones that playa role in controlling
carbohydrate metabolism. The endocrine cells are closely associated with
large numbers of blood capillaries into which they secrete the peptide
hormones.
Major function of the pancreas
1. Involved in digestion processes by producing:
a. Digestive enzymes: necessary to digest CHO, fat, and
protein
b. Bicarbonates: to neutralize the gastric juice
c. Water and electrolytes (Na+, K+ etc):
Location of secretion
1. Digestive enzymes & electrolytes are secreted by acinar
cells of the pancreases
2. HCO3- and water are secreted in cells lining the pancreatic
125
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-125-320.jpg)
![9/1/2023 126
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-126-320.jpg)
![(Cont…) pancreatic secretions
• Pancreatic secretion first synthesized in the pancreatic cells are
in the inactive forms.
• The inactive proenzymes secreted by cells of the pancreases
that break protein, fat, and CHO include:
• a. Trypsinogen (protein digestion)
• b. Chymo-trypsinogen (protein digestion) inactive
forms
• c. Pro-Carboxy-peptidase (protein)
• d. Pancreatic lipase (fat digestion)
• e. Alpha amylase (CHO digestion)
127
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-127-320.jpg)
![9/1/2023
(Cont…) Mechanism of action of pancreatic secretions
• All the inactive enzymes flow through the pancreatic and
common bile duct into the duodenum.
• At the beginning, an enzyme called enterokinase that is located
on the wall of the duodenum changes trypsinogen to trypsin.
• Trypsin then activates the others as follows (look steps b and c):
a. Trypsinogen ----enterokinase- Trypsin
b. Chymotrypsinogen---trypsin - Chymotrypsin
c. Pro-carboxypeptidase ---trypsin- Carboxypolypeptidase
1. Protein ------- Trypsin and/or chymotrypsin- to peptides
2. Peptides ------ Carboxypolypeptidase--- to amino acids
128
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-128-320.jpg)
![Cont….
• Trypsin & chymotrypsin split whole and partially digested proteins into
peptides of various sizes. They do not cause release of individual amino
acids (AA) Carboxypolypeptidase splits some peptides into individual AA.
• The pancreatic enzyme for digesting carbohydrates is pancreatic
amylase , which hydrolyzes starches, glycogen, and most other
carbohydrates (except cellulose) to disaccharides .
• The main enzymes for fat digestion are
• (1) pancreatic lipase, which is capable of hydrolyzing neutral fat into fatty
acids and monoglycerides;
• (2) cholesterol esterase, which causes hydrolysis of cholesterol esters;
and
• (3) phospholipase, which splits fatty acids from phospholipids.
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-129-320.jpg)


![9/1/2023 132
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-132-320.jpg)
![Formation of bicarbonate by the pancreas
• Carbon dioxide diffuses into the interior of the cell from the blood
• Then the bicarbonate ions are actively transported in association with
sodium ions (Na+) through the luminal border of the cell into the lumen of
the duct.
• The H+ formed by dissociation H2CO3 inside the cell are exchanged for
Na+through the blood border of the cell by a secondary active transport
process.
• This supplies the Na+ that are transported through the luminal border into the
pancreatic duct lumen to provide electrical neutrality for the secreted
bicarbonate ions.
• The overall movement of Na+ & HCO3
- ions from the blood into the duct lumen
creates an osmotic pressure gradient.
• That causes osmosis of water also into the pancreatic duct, thus forming an
almost completely isosmotic bicarbonate solution.
9/1/2023 Tariku A. [GIT Physiology]
CO2 + H2O H2CO3 HCO3
- + H+
CA
CA](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-133-320.jpg)
![9/1/2023
(cont…) formation bicarbonate by the pancreas
134
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-134-320.jpg)
![Regulation of Pancreatic Secretion
• Three basic stimuli are important in causing pancreatic
secretion:
• Acetylcholine, which is released from the parasympathetic
vagus nerve endings and from other cholinergic nerves in the
ENS. Mainly stimulates secretion of digestive enzymes.
• Cholecystokinin, which is secreted by the duodenal & upper
jejunal mucosa when food enters the small intestine. Mainly
stimulates secretion of digestive enzymes.
• Secretin, which is also secreted by the duodenal and jejunal
mucosa when highly acidic food enters the small intestine.
mainly stimulates secretion of sodium bicarbonate.
135
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-135-320.jpg)

![9/1/2023 Tariku A. [GIT Physiology]
Regulation of pancreatic secretion
Cephalic and gastric phase
Acetylcholine
CCK
enzymes
Secretin
water
bicarbonate](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-137-320.jpg)
![9/1/2023 Tariku A. [GIT Physiology]
Fat
Intestinal phase
Acetylcholine
CCK
enzymes
Secretin
water
bicarbonate
Regulation of pancreatic secretion](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-138-320.jpg)
![9/1/2023 139
Regulation of pancreatic secretion
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-139-320.jpg)

![9/1/2023
(Cont…) Hormonal regulation of pancreatic secretion
- Fats and amino acids stimulate the Duodenum to
releases CCK and Secretin. These hormones flow
through the blood and reach the pancreas.
In the Pancreas two processes take place
a . CCK stimulates b. Secretin stimulates
acinar cells to duct epithelium to
release digestive release H2O &
HCO3 enzymes
Both flow through common bile duct to
duodenum to do their specific job.
141
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-141-320.jpg)

![9/1/2023
• Pancreatic juice secretion is controlled in the acini by cholinergic (vagal) mechanisms and
by the hormone cholecystokinin (CCK, vagal stimulation seems to be enhanced by CCKA
receptors).
Both cause an elevation of cytosolic [Ca2+], which stimulates Cl- and pro-enzyme
secretion.
• Trypsin in the small intestinal lumen deactivates CCK release via a feedback loop.
• Secretin increases HCO3
- and H2O secretion by the ducts.
• CCK & vagal ACh potentiate this effect by raising cytosolic [Ca2+].
• The hormones also have a growth-promoting effect](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-143-320.jpg)
![9/1/2023
(Cont…) Digestive disorder, Pancreatitis
a. Absence of the enzyme enterokinase:
– In the absence of enterokinase, trypsin is not formed
to activate other proenzyme from the pancreases.
– Dietary proteins, thus, remain undigested. This
causes protein deficiency in the body.
b. Acute pancreatitis:
– Duct blockage produces logging of the secretions in
pancreatic tissues.
– This in turn causes activation of proenzyme causing
digestion of the pancreatic tissues within a few hours
leading to lethal conditions.
144
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-144-320.jpg)
![145
LIVER AND GALLBLADDER
• The liver is the heaviest gland in the body and the second
largest organ in the body after the skin.
• The liver is divisible into left and right lobes, separated by
the falciform ligament. Associated with the right lobe are
the caudate and quadrate lobes.
• The gallbladder is a sac located in a depression on the
posterior surface of the liver.
• The gall bladder is a sac that is lined with a simple
columnar epithelium and has a tunica muscularis
containing smooth muscle that is innervated by both the
parasympathetic and sympathetic branches of the ANS.
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-145-320.jpg)

![147
Functions of the liver
1. On Carbohydrate Metabolism:
• It is the site of glycogenesis, gluconeogenesis and glycogenolysis
• Turns proteins into glucose
• Turns triglycerides into glucose
• Turns excess glucose into glycogen & stores
• Turns glycogen back into glucose as needed
2. On Lipid Metabolism
• It is the site of β-oxidation, formation of phospholipids, lipoproteins,
synthesis of cholesterol, and conversion of CHO into fat
3. Protein Metabolism
• Deamination of amino acids = removes NH2 (amine group) from amino
acids so can use what is left as energy source
• Converts resulting toxic ammonia (NH3) into urea for excretion by the
kidney
• Synthesizes plasma proteins utilized in the clotting mechanism and
immune system
• Converts one amino acid to another
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-147-320.jpg)
![148
Other Functions of the liver
4. Inactivation of drugs & hormones (Sulfonamide,
penicillin, thyroid, steroids)
5. Removes the waste product; bilirubin
6. Releases bile salts
7. Stores fat soluble vitamins: A, B12, D, E, K
8. Stores iron and copper
9. Filtration of blood: phagocytizes worn out blood
cells & bacteria. Removes blood clots and toxins
from portal circulation
10.Activates vitamin D
11.Storage of blood: a major blood reservoir
12.Synthesis of blood clotting factors (F-I, II, VII, IX, X)
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-148-320.jpg)
![149
Secretion of bile
Bile is secreted by hepatocytes in the liver for two purposes
1. It facilitates fat digestion and absorption of fat
2. Serves as a means of excretion of waste products
(bilirubin and cholesterol)
Bile secretion has two stages:
1. Primary secretion: contains bile salt, cholesterol, lecithin,
electrolytes (Na, Ca, K ions)
2. Secondary secretions: contains primary secretions plus
water, NaHCO3, Cl.
• Average biliary out put: 600 -1200 ml/day
• Yellow-green in color b/c of bilirubin & pH = 7.6 - 8.6
• The gallbladder can hold 30 to 60 milliliters only
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-149-320.jpg)
![9/1/2023
(Cont…) Bile Production in the liver
- Bile is an alkaline fluid (pH 8)
- secreted in the liver
- functions in emulsification of
fat in the duodenum.
- Emulsification means
changing greater fat globules
into smaller fat-droplets
called micelles
150
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-150-320.jpg)
![9/1/2023
(Cont…) Composition of bile
151
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-151-320.jpg)
![9/1/2023 152
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-152-320.jpg)
![9/1/2023
(Cont…) Constituents of bile
• Bile contains the following constituents:
1. Bile salts (bile acids), ~11%
2. Bile pigment (bilirubin), ~1%
3. Others organic constituents like: (~3%)
Cholesterol, Lecithin, protein etc.
4. Electrolytes (Na+, K+, Ca2+, Cl-, and greater
HC03- than plasma) ~1%.
5. H2O (~ 84%) also takes the higher share of
bile
153
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-153-320.jpg)

![9/1/2023
(Cont…) Bile, Enterohepatic circulation
155
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-155-320.jpg)
![156
Regulation of Bile Secretion
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-156-320.jpg)

![• The sympathetic nervous system inhibits
gallbladder contractions via α2 adrenoreceptors located on
cholinergic fiber terminals.
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-158-320.jpg)

![9/1/2023
(Cont…) Bilirubin in the Small intestine
- In the intestine, bacterial actions change bilirubin into
stercobilin and urobilinogen.
- They are further oxidized and excreted in feces or urine as
stercobilin and urobilin.
• Excess level of bilirubin in the blood (>18 mg/L) causes
jaundice (icterus), that is, yellow coloration of the sclera's, skin
etc occurs.
• 3- types of jaundice:
• A. Prehepatic jaundice : Increased Hemolysis of RBC
• B. Intrahepatic jaundice: Liver disease
• C. Posthepatic jaundice: Blockage or obstruction of the bile
ducts.
160
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-160-320.jpg)
![Gall Bladder (GB)
• The gall bladder receives bile from the liver. Bile is composed of
bile salts that emulsify fats forming water-soluble complexes
with lipids (micelles)to facilitate the absorption of fat. Bile salts in
the small intestine also activate lipases in the intestine.
Functions of the GB
1. storage of bile
2. concentration of bile
3. acidification of bile
4. send bile to the duodenum in response to CCK which is
secreted by enteroendocrine cells of the small intestine;
horse does not have a gall bladder & bile is continuously
received from the liver.
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-161-320.jpg)
![9/1/2023
(Cont…) Gall bladder and gall stone formation
• GB is a storage sac for bile.
• GB is stimulated by CCK which
constricts the GB & release bile.
• Bile emulsifies fat in the
duodenum.
• Cholesterol & other substances
precipitate in the GB, and this
effect favors gall-stone formation.
162
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-162-320.jpg)
![9/1/2023
(Cont…) Digestive disorder, Gallstone
- The GB stores bile between meals, concentrates bile (by
reabsorbing water & electrolytes), and
- Releases bile through cystic & common bile duct into the
duodenum.
- During the reabsorption process bile salts, bile pigments, and
cholesterol become increasingly concentrated.
- These substances precipitate & form solid crystals.
- When they become larger they form gallstones.
- Gallstones may then block the flow of bile causing obstructive
jaundice.
- Gallstone accumulation may obstruct bile flow to the
duodenum resulting in jaundice (bilirubin a yellowish-green
by-product of heme metabolism increases in plasma giving
yellowish pigment).
163
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-163-320.jpg)
![9/1/2023 164
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-164-320.jpg)

![9/1/2023
(Cont…) The Small intestine (SI)
SI is specialized for completion of
digestion and absorption of
nutrients.
A. Duodenum: ~ 25 cm, mainly
secretory, mucous, hormones,
enzymes)
B. Jejunum : ~1.5 m mainly absorptive
C. Ileum : ~1.7 m mainly absorptive
166
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-166-320.jpg)
![9/1/2023
(Cont.) Small intestine, structure
-Structure of the wall is similar to others and consists of
4-layers (Mucosa, Submucosa, Muscularis externa &
Serosa).
-Enteric and Autonomic (Vagal) nerves profusely
innervate the Small intestine.
-The inner lining is greatly folded to increase the
surface area for absorption, thus
-(The microvillus + Villi + greater folding called
valvulae conniventus- increase the absorptive
surface of Small intestine by ~ 600-fold). Area of a
“Tennis-ball”
167
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-167-320.jpg)
![9/1/2023
Small intestine, the brush border (microvillus)
Brush border or microvilli: increase the surface
area to a great extent in the small intestine
168
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-168-320.jpg)
![9/1/2023
(Cont…) the Small intestinal Villi
• Milking of the villi:
- The muscularis mucosa
that fold to a great extent
in the small intestine
increase the surface area
necessary for absorption
- Also contraction of the Villi
milk the villi and help the
lymph to flow.
169
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-169-320.jpg)
![9/1/2023
(Cont…) Small intestine, Villi
• Mucus: protect and
lubricate
The Mucus is secreted
by:
a. Brunner's glands
located in the
duodenum
b. Goblet cells in other
parts of the intestine
c. Paneth cells lymph
nodules in the villi
170
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-170-320.jpg)
![9/1/2023
(Cont…) Small intestine, The Villi
- Villi: Are numerous finger like projections that emerge
from the mucous membrane.
- Each Villi consist of a layer of absorptive epithelial
cells that contain minute microvilli (brush border) at
their surfaces.
- The epithelial cells contain digestive enzymes like
sucrase, maltase, lactase, and peptidases in the
membranes of the microvillus.
Small intestinal Villi
• Glands at the base of Villi (entrocytes): Secrete large
watery fluid (pH ~ 7-7.5, neutral).
• Epithelial cells of the villus: Also secrete digestive
enzymes that break nutrients before absorption takes
place.
171
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-171-320.jpg)
![9/1/2023
(Cont…) Small intestine, Villi
The enzymes breaks disaccharide into
monosaccharide before absorption and
peptides into amino acids
Cells in the Lieberkühn crypts divide fast
(mitosis) and are replaced by new ones (every
2-5days)
Villi contain centrally located, blood capillaries
lymphatic (lacteals), nerve fibers and
connective tissues.
172
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-172-320.jpg)
![9/1/2023
(Cont…) Small intestine, motility
• Motility in the small intestine are of 2-types
1. Segmentation & 2. Peristalsis
1. Segmentation: involves ring like (rhythmical) contraction
and relaxation of the intestine in short distances.
- Segmentation provides a sustained small divisions and
mixes the chyme by bringing it into contact with the intestinal
wall.
• This small ring like contractions help chop, cut and
mix the chyme to a greater degree with intestinal juice.
- Also such motility allows the contents to stay longer and
promote increased absorption of the chyme.
173
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-173-320.jpg)
![9/1/2023
(Cont…) Motility, Segmentation in small intestine
174
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-174-320.jpg)
![9/1/2023
(Cont…) Small intestine, peristalsis
• 2. Peristalsis (propulsive) motility
• Peristaltic waves move the chyme to the anal direction
(velocity 2 cm/sec)
• Generally, it takes 3-5 hours to pass the chyme from
the pylorus to Ileo-cecal valve.
• Nervous reflexes that increases peristalsis includes
gastro-enteric reflex that starts when stomach
distends & sends signals to small intestine
• Hormonal signals that stimulate peristalsis include
CCK, gastrin, serotonin, insulin, motilin.
• Secretin & glucagon inhibits SI motility.
175
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-175-320.jpg)
![9/1/2023
(Cont…) Small intestinal motility, peristalsis
Peristalsis in SI:
Generally the usefulness of peristalsis is 2-fold:
A. To cause progression of chyme to LI
B. To spread out the chyme along intestinal mucosa
- When reaching the Ileocecal sphincter, the chyme is
blocked for several hours until the person eats another
meal.
- There after, a gastro-ileal reflex intensifies peristalsis and
this reflex forces the chyme to reach the large intestine.
Peristaltic rush:
• Is a powerful & rapid contraction of the small intestine
caused by irritation of the intestinal walls (e.g, as in
diarrhea).
• It sweeps the contents of the intestine into the colon and
176
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-176-320.jpg)
![9/1/2023
(Cont…) Small intestine, Ileosecal valve
• Function of Ileocecal valve & delay of emptying from
small intestine
- The Ileocecal sphincter prevents backflow of fecal matter from
the colon to small intestine.
- When pressure builds in the cecum, the valve protrudes into
the lumen of the cecum and is forcefully closed.
- Reflex control of the Ileocecal sphincter (cause of delay of
emptying from SI).
Cecum distention--- increased contraction of the sphincter -
-- ileum peristalsis is inhibited- Delay of emptying is
caused
Also irritants in the cecum delay emptying
177
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-177-320.jpg)

![9/1/2023
(Cont…) Small intestine, CHO absorption
179
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-179-320.jpg)
![9/1/2023
Digestion of carbohydrates
180
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-180-320.jpg)
![9/1/2023
(Cont…) Absorption of Na+ ion and H2O by osmosis in
the Small intestine
181
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-181-320.jpg)
![9/1/2023
(Cont…) Small intestine, fat absorption
182
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-182-320.jpg)
![9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-183-320.jpg)
![9/1/2023 184
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-184-320.jpg)
![9/1/2023
(Cont…) Fat soluble vitamins (A, D, E, K)
• Fat soluble vitamins are mixed with micelles formed by
the bile acids and lipid digestion products.
• These bile acids and lipid digestion products in the small
intestine enhances the absorption of Fat-soluble vitamins.
• In the epithelial cells of the small intestine, the fat soluble
vitamins enter the chylomicrons and leave the intestine
with the lymph. However, a small fraction may be
absorbed and leave the intestine with the portal blood
185
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-185-320.jpg)
![9/1/2023
(Cont…) Small intestine, Protein absorption
186
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-186-320.jpg)
![9/1/2023
Digestion of proteins
187
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-187-320.jpg)

![9/1/2023
Large intestine (colon), Function
Function of the large intestine
1. Water absorption
2. Electrolyte absorption; mainly NaCl
3. Mucous & HCO3
- Secretion
4. Storage, transport, and evacuation of feces
5. Absorption of some drugs (suppositories)
6. Bacterial fermentation in the colon stimulates
synthesis of some vitamins
189
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-189-320.jpg)
![9/1/2023
• After the cecum, the colon
consists of the ascending and
transverse colons, which are
mostly involved in absorption
& secretion.
• The descending & sigmoid
colons are mostly the site of
storage of fecal matter.
• The sigmoid joins the
muscular rectum, where
storage and stimulation of
defecation induces bowel
movement.
• The anus that has two
sphincters is involved in
control of involuntary and
voluntary evacuation of the
ingesta (defecation reflex).
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-190-320.jpg)
![9/1/2023
(Cont…) Large intestinal motility
• Like Small intestine motility, LI motility is governed
by:
A. Haustral movement (segmentation)
B. Mass movement
A. Haustral movements
In the colon, segmentation movements occur in
a large circular constrictions that are
powerful enough to close the diameter to a
narrow loop.
Moreover, the 3-longitudinal muscles “teniae
coli” contract and push the segments into a
bag-like portions called haustrations.
191
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-191-320.jpg)
![9/1/2023
Motility of the colon
A. Characteristics of Haustral movements:
Move slowly through the colon.
– This slow movement rolls the fecal matter and help expose the
fecal contents to the mucosal surfaces of the colon.
– Its contact with the mucosal surfaces promotes efficient
absorption of fluid and electrolytes from the colon.
B. Mass (propulsive) movement:
- Produced by slow and continuous Haustral contractions and supported or modified
by peristaltic actions.
- Mass movements occur seldom (~ 1 - 3/d or once after a breakfast), gastro-colic or
duodeno-colic reflex initiate mass movement.
- When mass movement forces feces into the rectum, the desire for defecation
occurs immediately, including reflex contraction of the rectum and relaxation of
the internal anal sphincter.
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-192-320.jpg)

![Mucus secretion
• The mucosa of the large intestine, like that of the small intestine,
has many crypts of Lieberkühn
• However, unlike the small intestine, there are no villi.
• The epithelial cells secrete almost no digestive enzymes they
contain mucous cells that secrete only mucus.
• This mucus contains moderate amounts of bicarbonate ions
secreted by a few non-mucus-secreting epithelial cells.
• Mucus in the large intestine protects the intestinal wall against
excoriation
• It provides an adherent medium for holding fecal matter
together.
• It protects the intestinal wall from the great amount of bacterial
activity that takes place inside the feces
• The mucus plus the alkalinity of the secretion provides a barrier
to keep acids formed in the feces from attacking the intestinal
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-194-320.jpg)
![Colon, defecation reflex
- Mainly, the sacral
spinal cord is involved
in this reflex and the
Cholinergic
parasympathetic fibers
are important for they
greatly innervate the large
intestine.
- The reflex: Stimulation of
receptors in the rectum
by feces > Sensory
impulses to the sacral
spinal cord > Motor reflex
through PSN ( pelvic +
pudendal nerves) back to
the colon > Powerful
peristalsis mainly at
descending, sigmoid,
rectum, & anal regions +
relaxation of internal 195
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-195-320.jpg)

![Composition of the Feces
• The feces normally are about three-fourths water and one-
fourth solid matter
• That is composed of about 30%dead bacteria ,10 to 20%fat,
10 to 20% inorganic matter, 2 to 3% protein, and
30%undigested roughage from the food and dried
constituents of digestive juices, such as bile pigment and
sloughed epithelial cells.
• The brown color of feces is caused by stercobilin and urobilin,
derivatives of bilirubin.
• The odor is caused principally by products of bacterial action
• These products vary from one person to another, depending
on each person's colonic bacterial flora and on the type of
food eaten.
• The actual odoriferous products include indole, skatole,
mercaptans, and hydrogen sulfide
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-197-320.jpg)

![(Cont…) Digestive disorders, Lactose intolerance
Lactose intolerance
- Is mostly hereditary, caused by deficiency of the enzyme lactase located at
the brush border of the small intestine.
- Lactose (milk sugar) is a disaccharide and should be degraded to galactose
and glucose, in order to be absorbed into the blood.
- The undigested lactose reaches the colon (large intestine) and is acted by
bacteria’s.
- This result is increased gas production, borborgymi (noise), flatulence, and
enhanced motility of the colon.
- Lactose intolerant subjects usually dehydrate for they lose water to the colon
(b/s osmolality increases)
- Infants, who are lactose intolerant, dehydrate and show diarrhea for they do
not utilize lactose.
- Thus formula milk with lactose should be avoided.
Peptic ulcers :
- Normally the stomach and intestinal walls are protected by mucosa against the
eroding actions of HCL.
- Excess acid secretion erodes the wall creating wounds (ulcers). If these wounds are
deep enough, they can reach the vascular layer and cause bleeding
- Increased secretion of gastrin and excessive activity of the Vagus nerve as well as
psychological factors stemming from anxiety and stress are believed to be involved
as causatives and also infected with a bacterium known as Helicobacter pylori.
9/1/2023 Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-199-320.jpg)
![9/1/2023
Vomition
- Is forceful expulsion of stomacheal and upper intestinal contents
through the esophagus, pharynx, and mouth.
Mechanism of vomition reflex:
- Vomition reflex is mainly controlled by “a vomition center” located
in the medulla oblongata (MO).
- Moreover, another center that causes vomition is the so called
“chemoreceptor trigger zone, CTZ” located at the root of the 4th
ventricle.
- There is a neural connection between the two centers.
- CTZ causes central vomiting and is stimulated by chemical
substances (e.g., drugs like morphine's etc), pregnancy, alcohol,
movement etc.
Consequences of prolonged vomition:
Excessive vomition > large loses of fluids and salt > severe
dehydration > decreased plasma volume > circulatory imbalances
occur.
200
Tariku A. [GIT Physiology]](https://image.slidesharecdn.com/4ogbrgrorigdyqtuou20-025-git-physiology1-230901191817-836ee5f9/85/025-GIT_Physiology1-ppt-200-320.jpg)