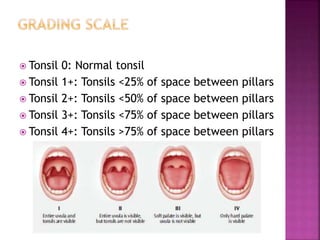
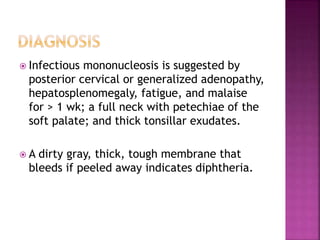
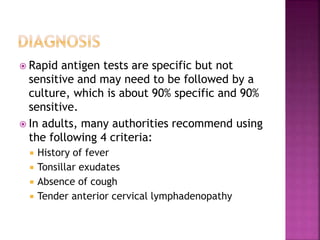
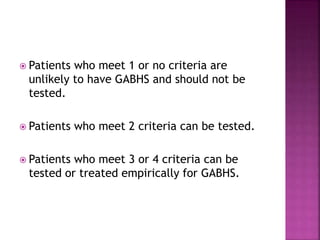
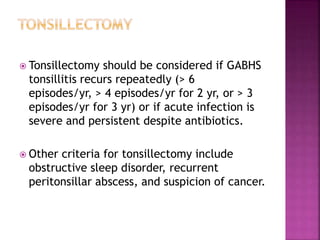
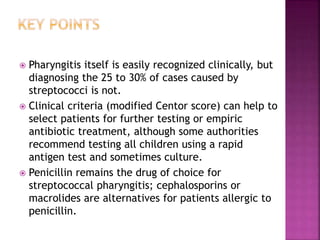
This document discusses tonsillopharyngitis (acute infection of the pharynx and tonsils). It notes that the condition is usually viral but is occasionally bacterial, most commonly caused by Group A beta-hemolytic streptococcus (GABHS). Symptoms include pain with swallowing, fever, and swollen tonsils. Diagnosis involves a clinical exam plus rapid antigen test or culture. Treatment depends on the cause but may include analgesics, hydration, and antibiotics for bacterial infections like GABHS. Tonsillectomy is considered for recurrent GABHS infections.