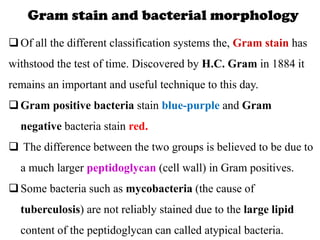
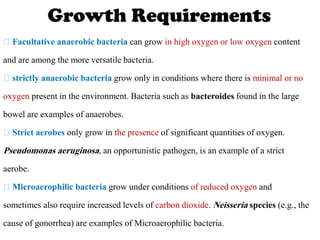
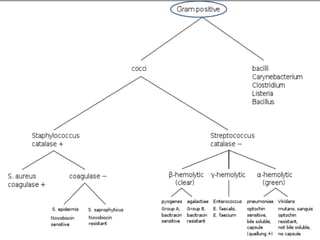
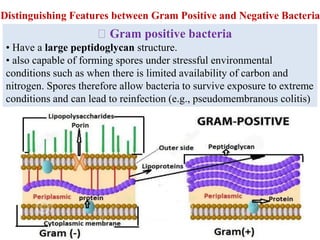
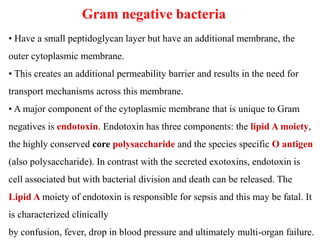
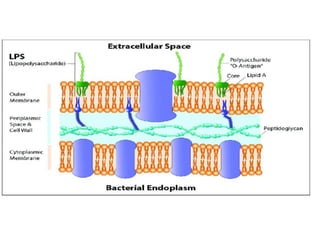
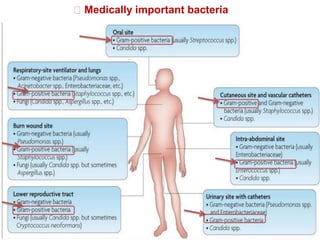
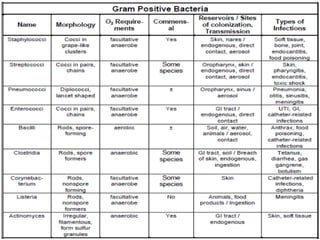
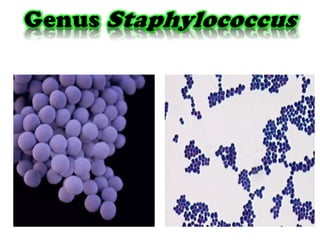
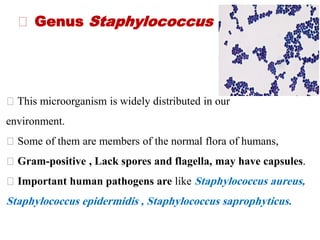
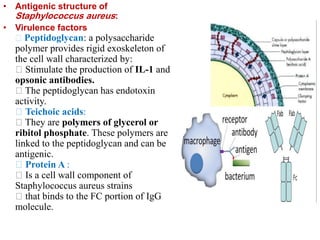
This document discusses the classification and typing of bacteria. It begins by explaining that bacteria can be grouped using phenotypic typing schemes utilized by clinicians, which examine bacterial morphology, staining properties, oxygen requirements, and biochemical tests. It also notes the importance of identifying the environmental reservoir and transmission means for clinicians. The document then provides details on various classification schemes for bacteria, including based on shape, staining, oxygen requirements, temperature tolerance, and structure. It focuses on the Gram stain technique and discusses characteristics of Gram-positive and Gram-negative bacteria.