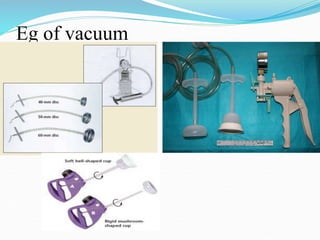
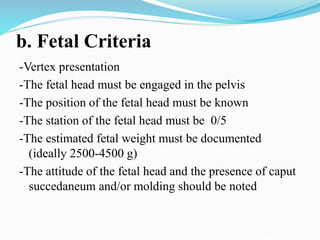
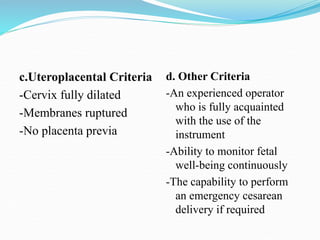
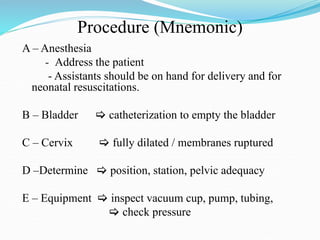
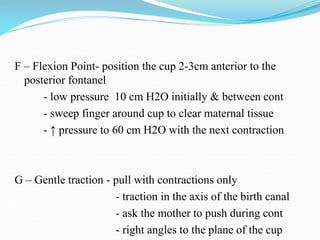
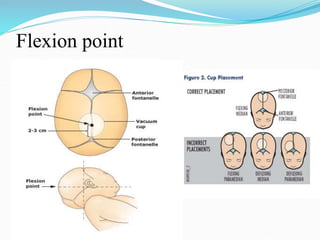
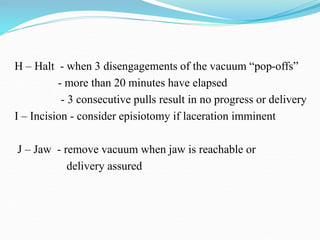
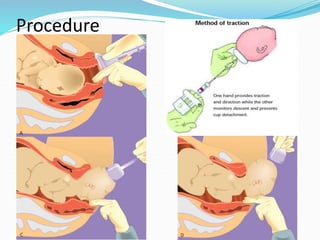
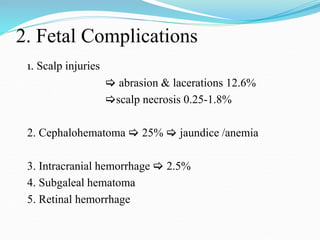
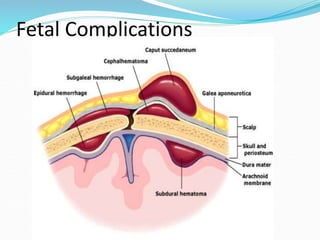
This document outlines vacuum-assisted vaginal delivery (VVD). It defines VVD as using a suction cup on the fetal head attached to a vacuum pump to provide traction during contractions. It classifies VVD by fetal station and lists indications such as prolonged second stage or fetal distress. Contraindications include non-vertex presentation or cephalopelvic disproportion. The document details prerequisites, provides a mnemonic for the procedure, discusses complications, and notes advantages like less force on the fetal head and disadvantages like requiring maternal effort.