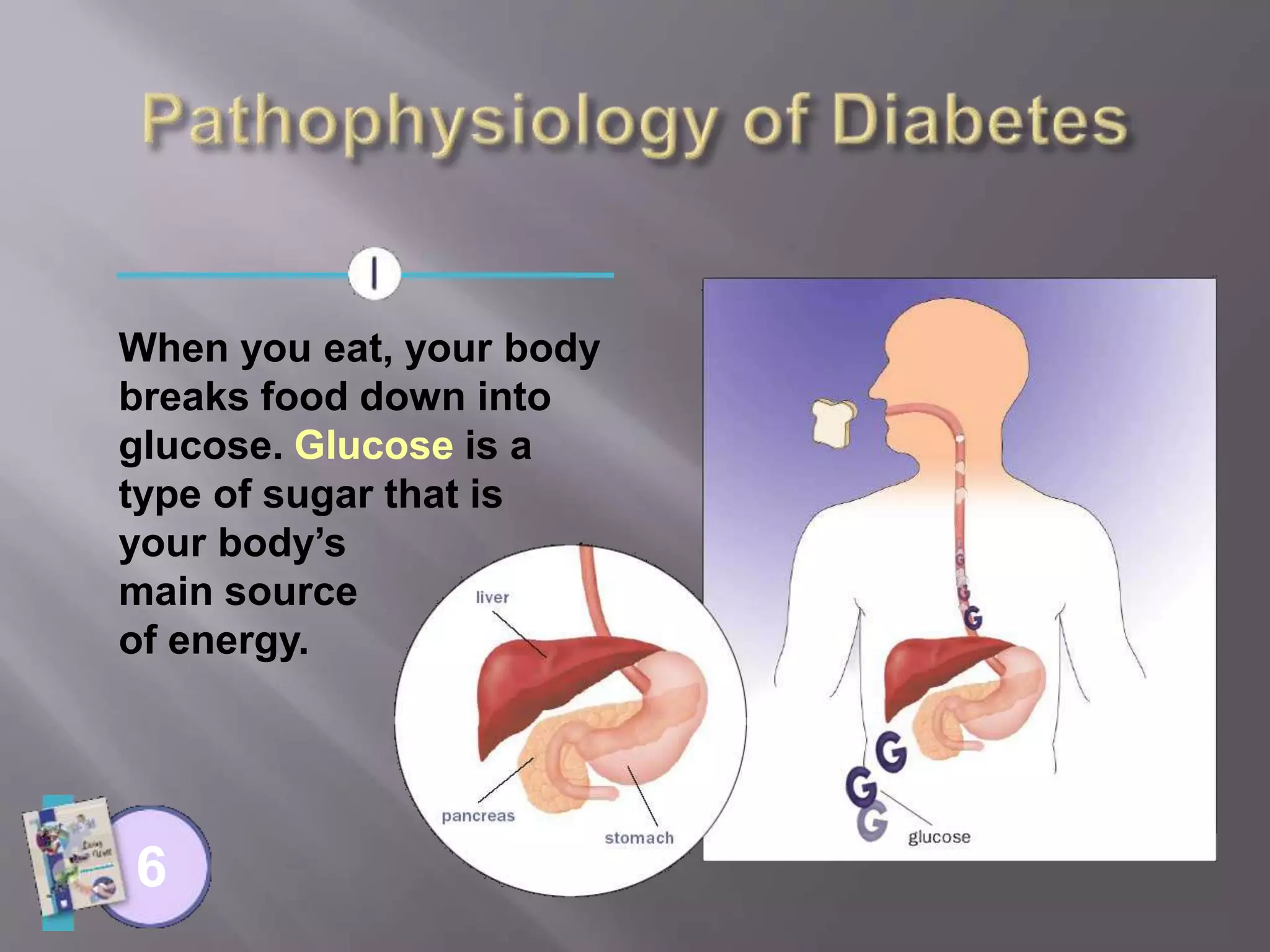
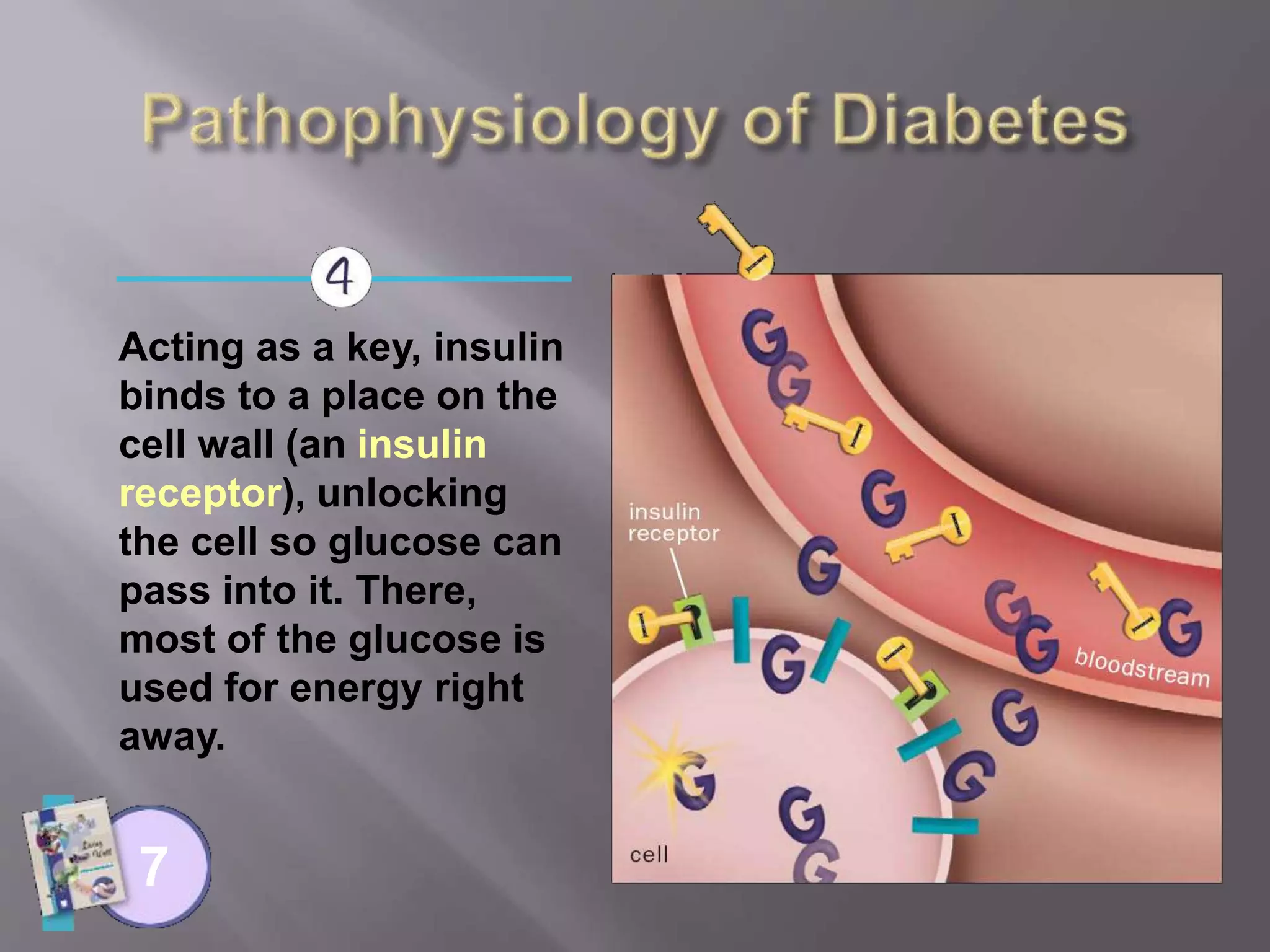
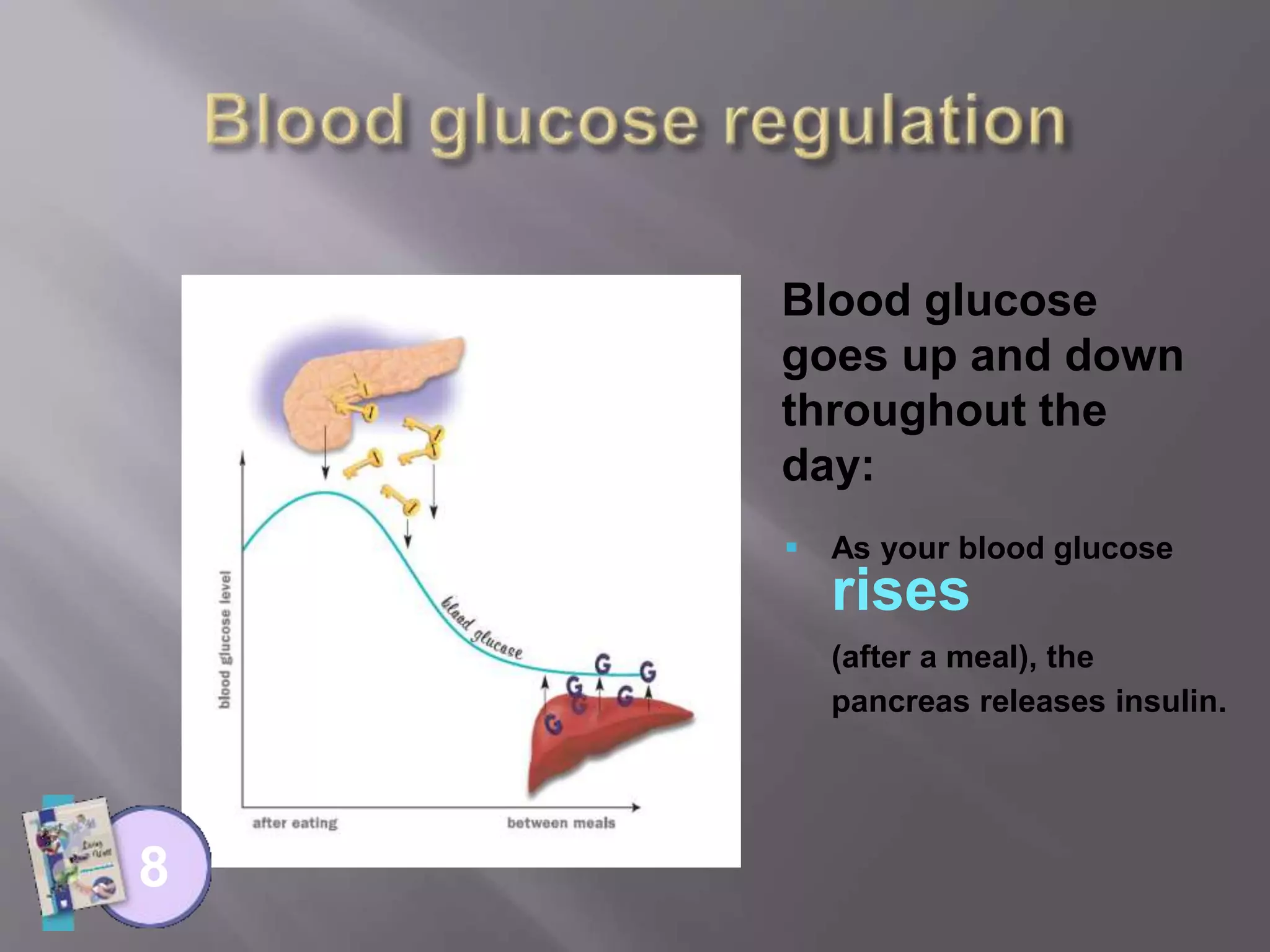
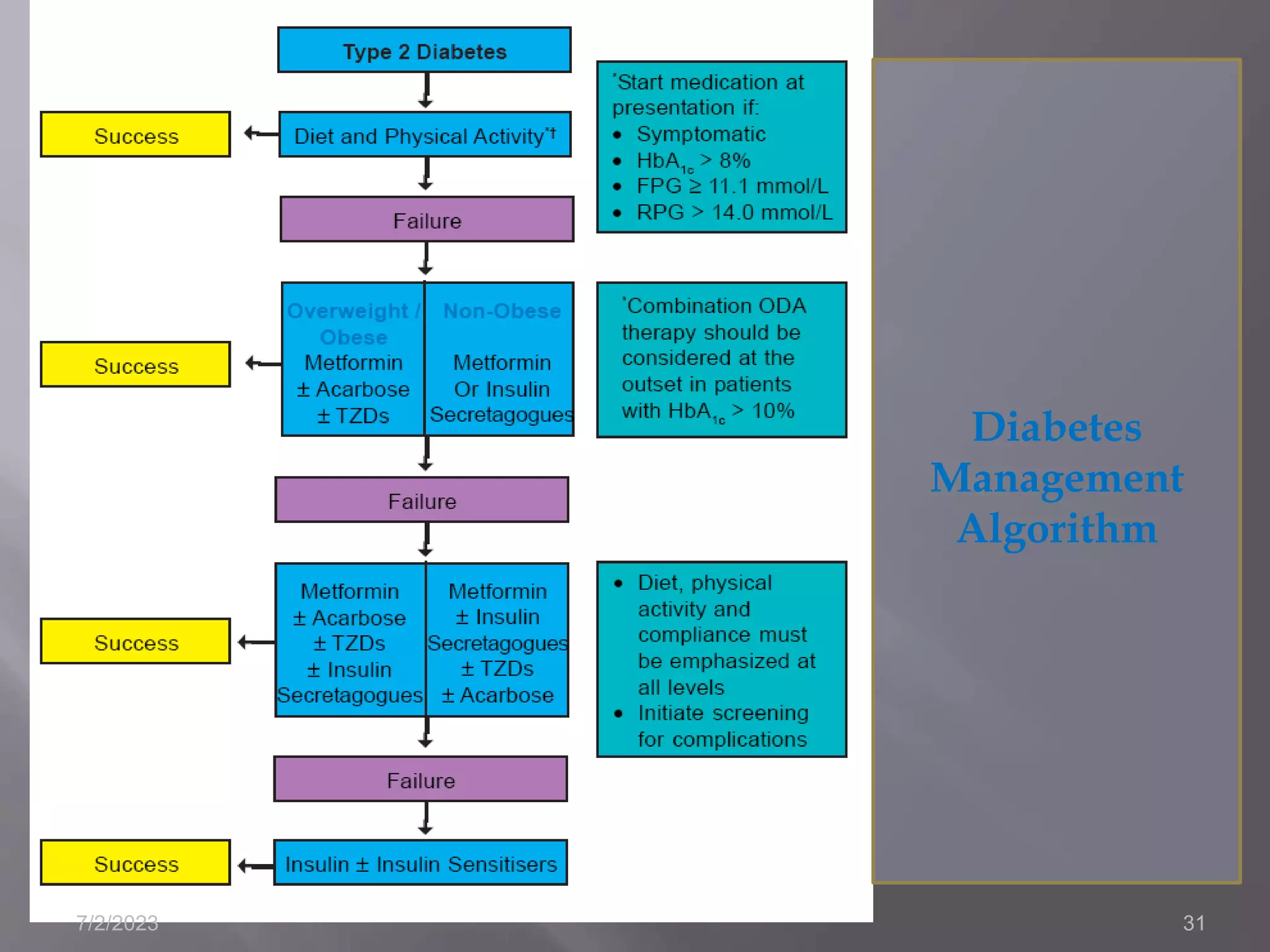
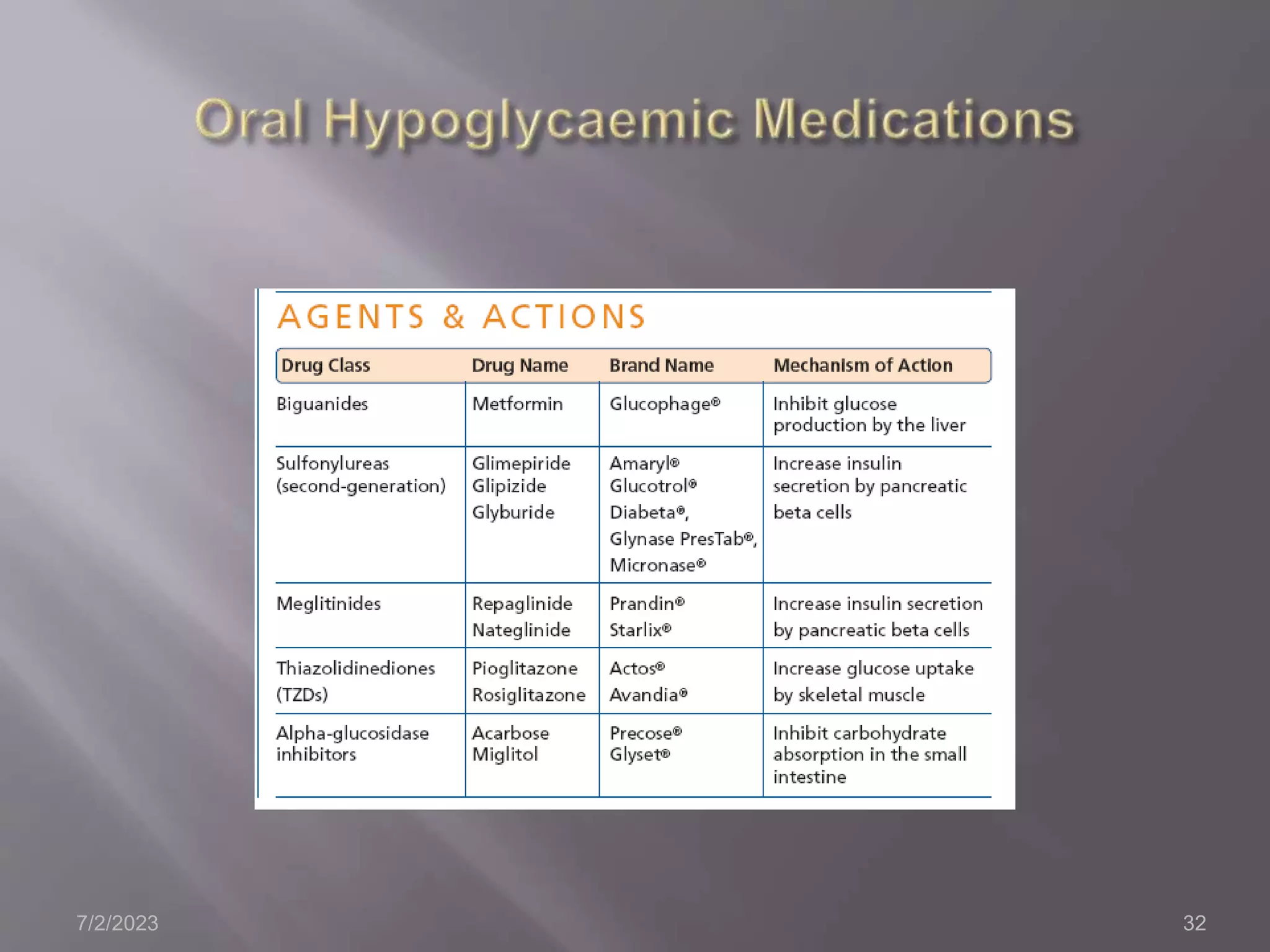
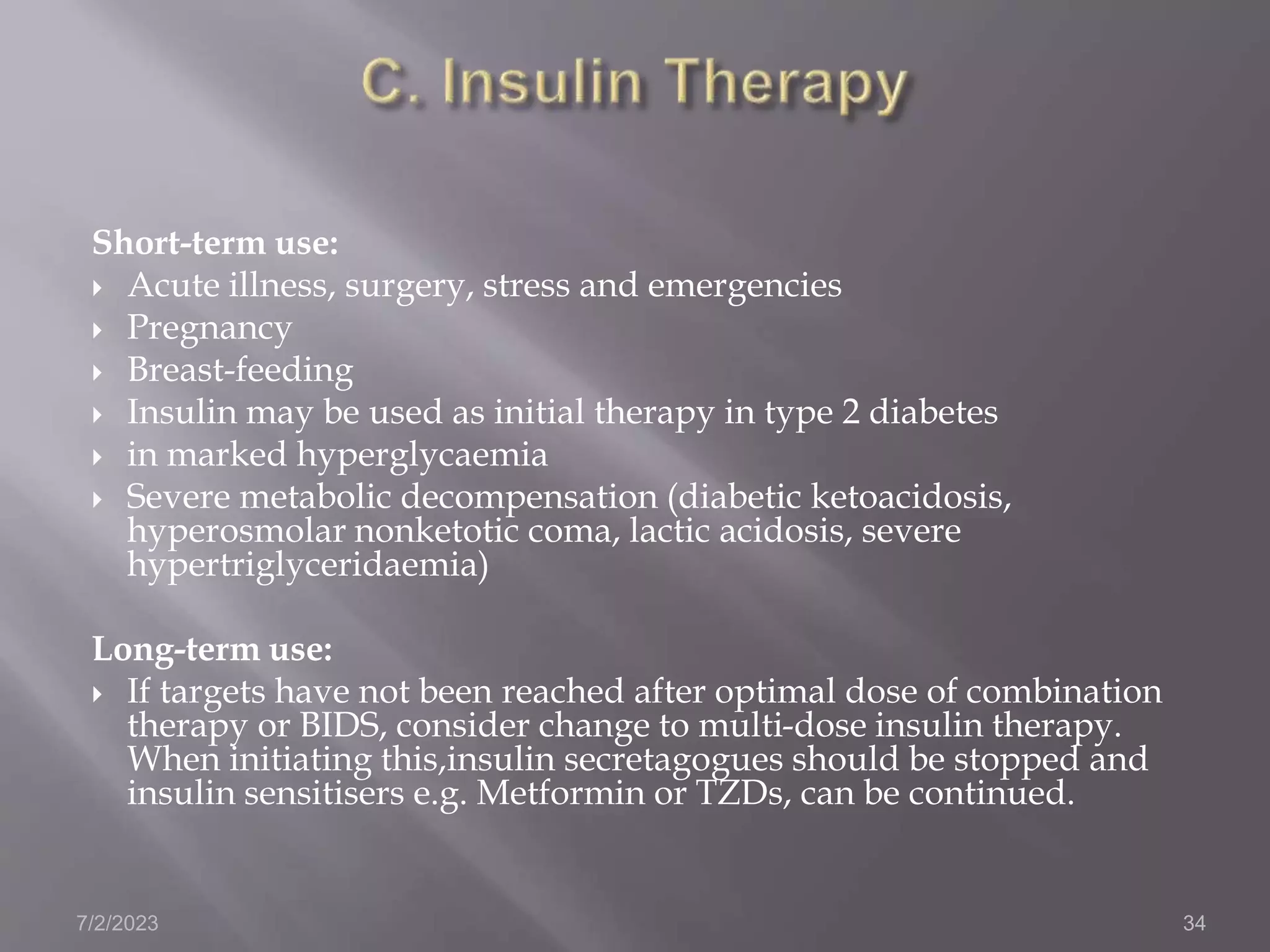
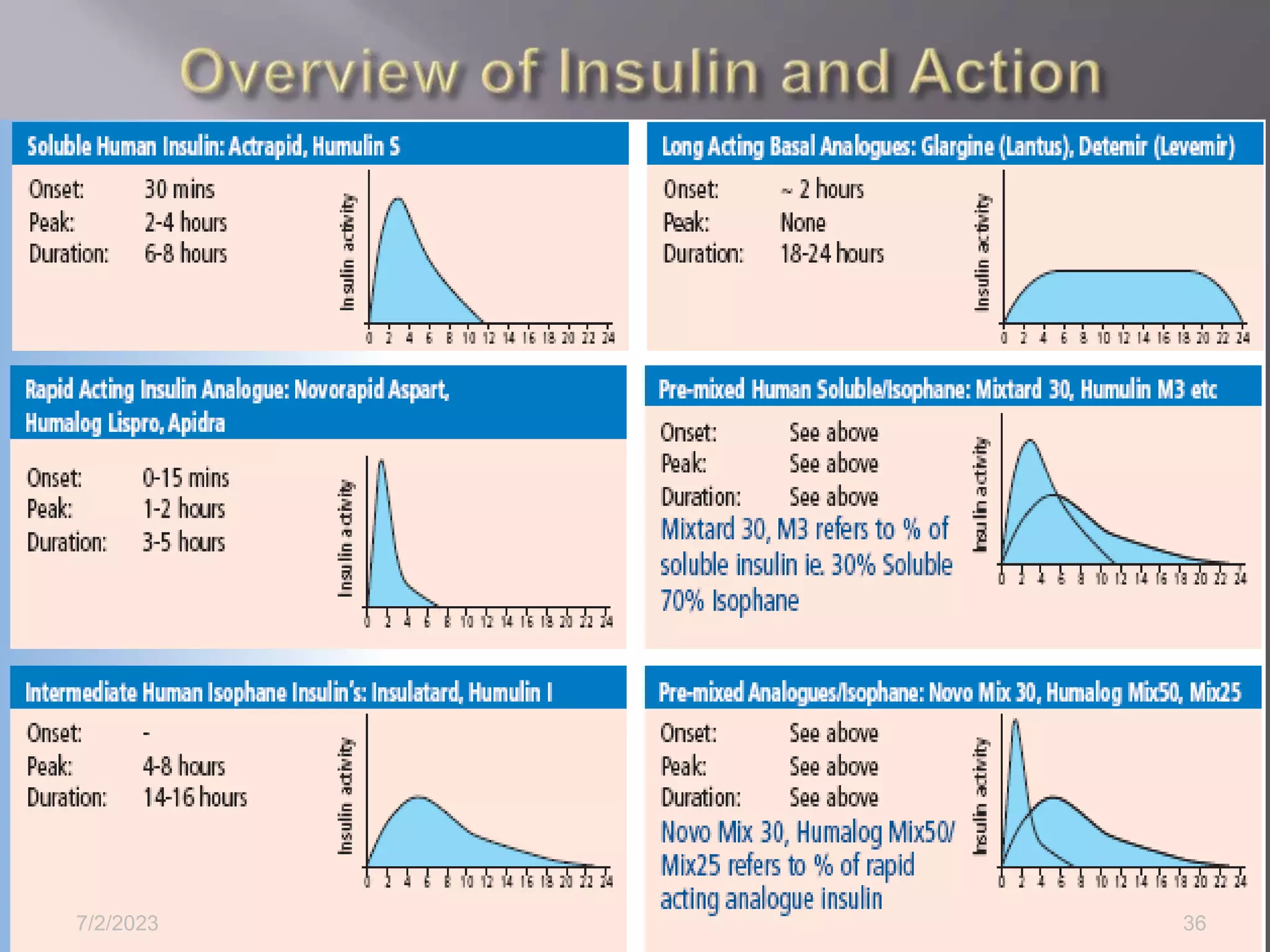
This document provides information on diabetes mellitus (DM), including describing its classification, symptoms, complications, management, and prevention. It defines DM as a group of metabolic diseases characterized by high blood glucose levels. DM is classified into type 1, type 2, and gestational diabetes. The document outlines that management of DM involves lifestyle modifications like diet and exercise, as well as oral hypoglycemic medications or insulin therapy. It also discusses preventing the progression of prediabetes to DM through lifestyle changes and medications.