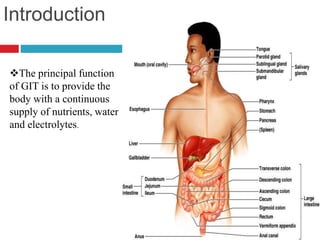
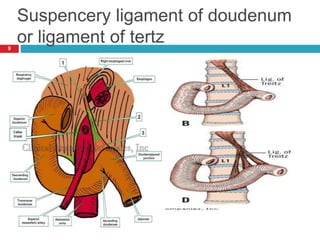
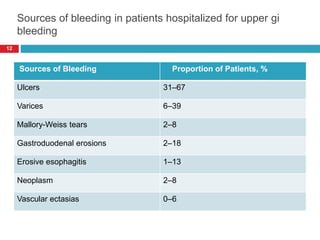
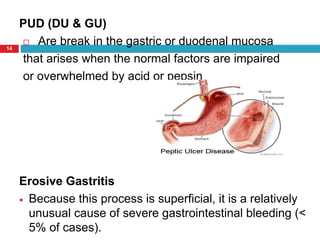
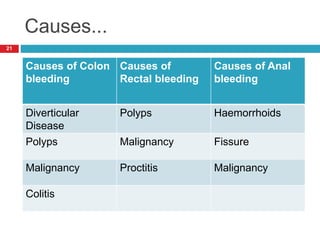
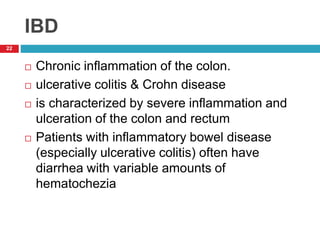
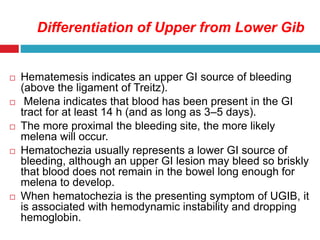
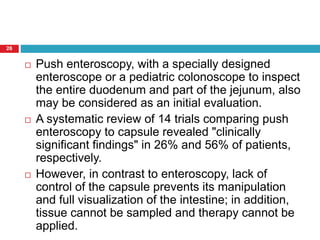
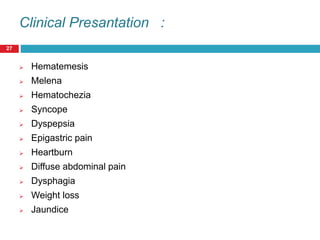
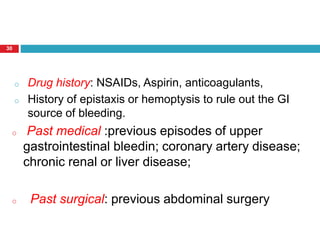
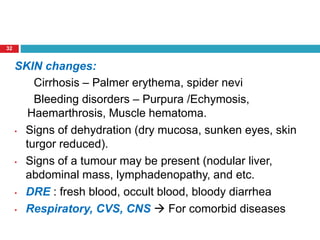
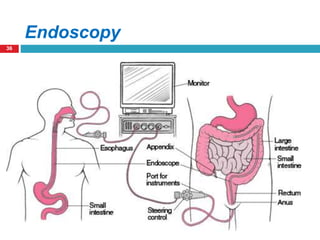
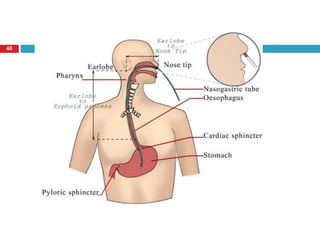
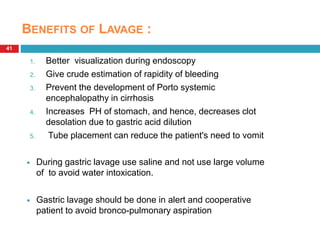
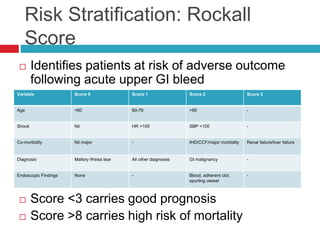
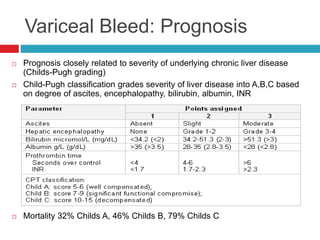
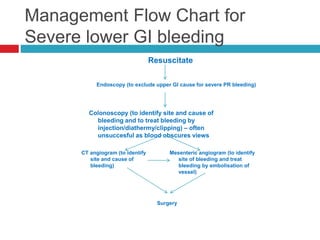
This document discusses the approach to patients presenting with acute gastrointestinal bleeding. It begins with an overview of gastrointestinal anatomy and blood supply. It then discusses the classification, causes, and clinical presentation of upper and lower GI bleeding. The summary concludes with the key aspects of evaluating a patient with GI bleeding, including history, physical exam, labs, endoscopy, imaging, and risk stratification using the Rockall score.