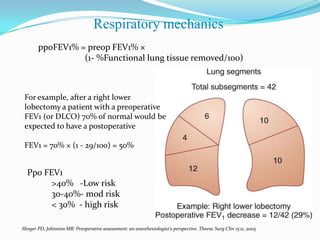
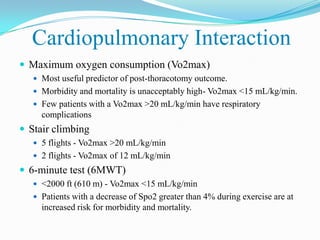
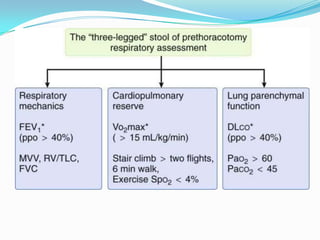
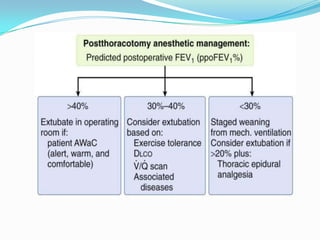
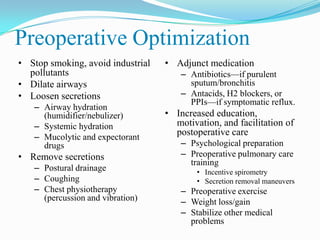
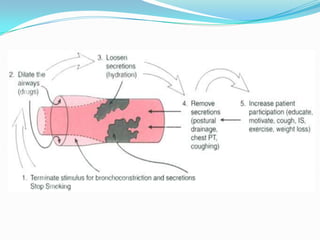
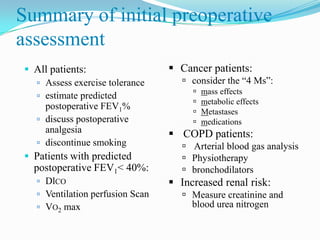
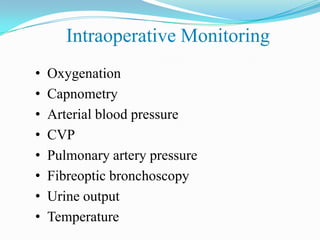
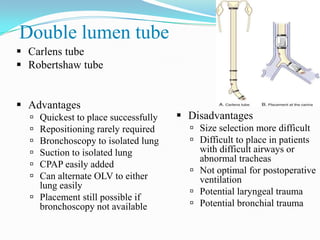
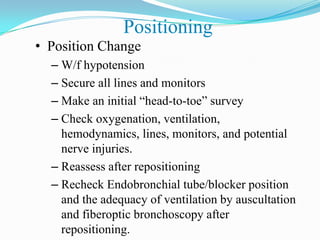
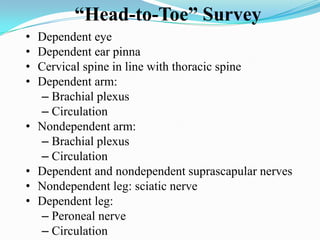
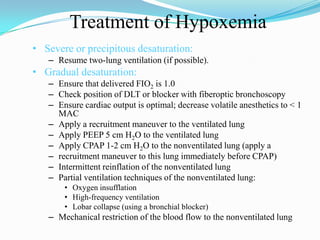
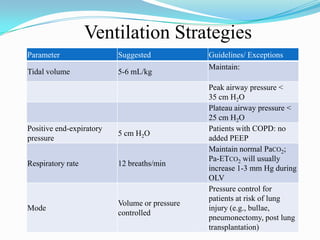
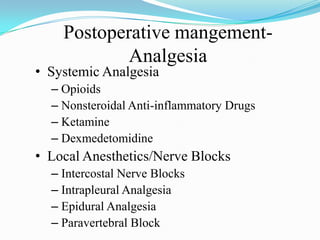
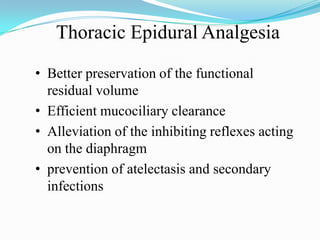
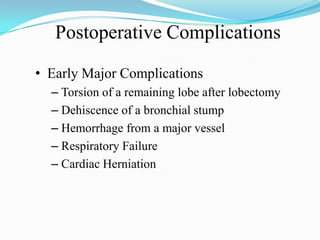
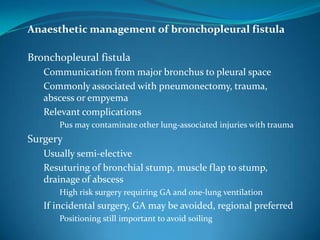
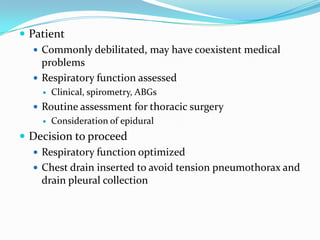
This document discusses anesthesia considerations for patients with chronic lung disease undergoing surgery. It covers preoperative assessment of pulmonary function, intraoperative monitoring and lung isolation techniques, positioning, and one lung ventilation. Postoperative management focuses on analgesia and complications related to chronic lung conditions. Preoperative optimization aims to improve patient risk stratification and respiratory status prior to surgery.