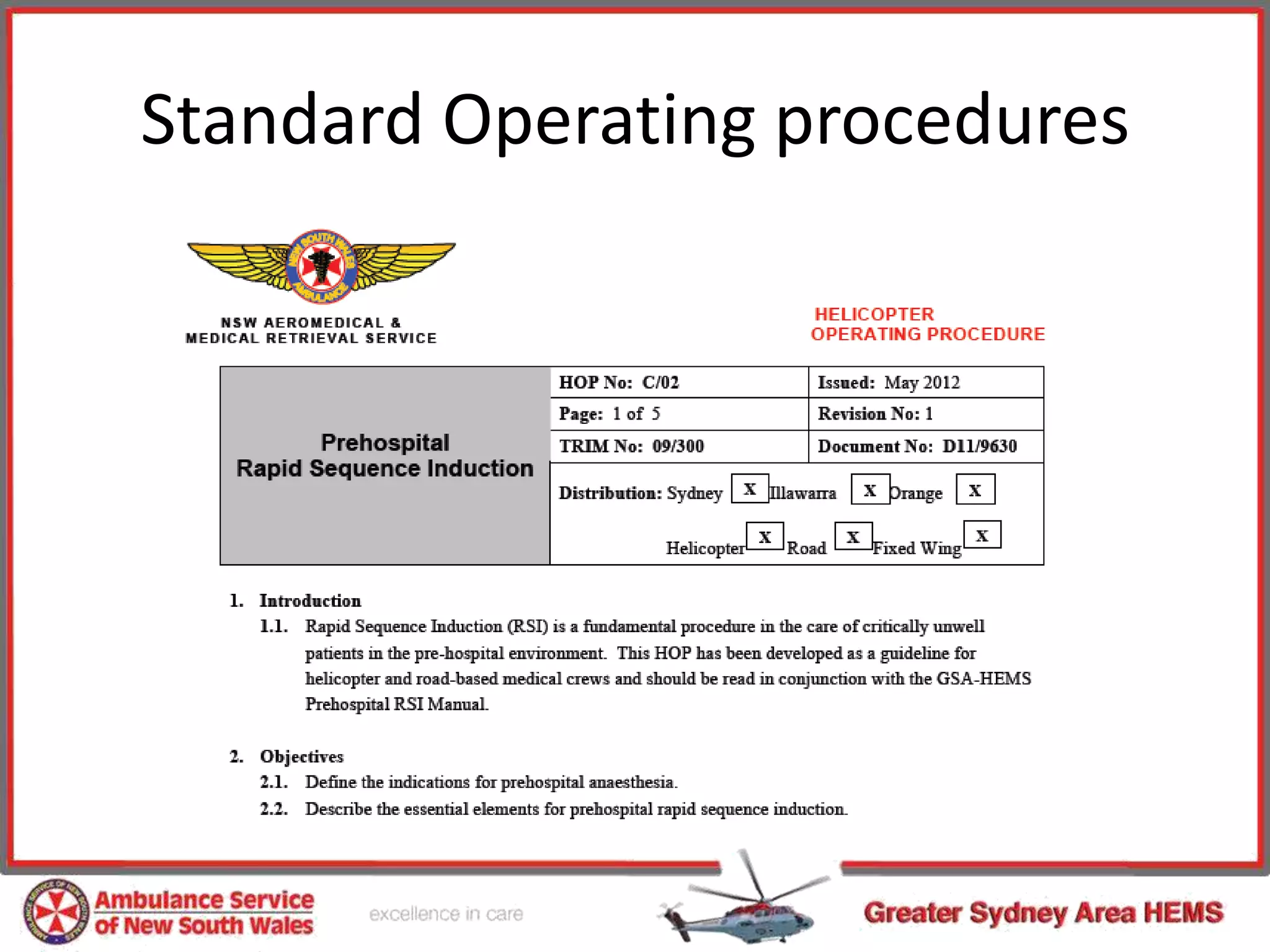
Rapid sequence intubation (RSI) in the pre-hospital setting can provide a higher level of care for trauma patients with airway compromise or risk of aspiration. While controversial, RSI performed by a trained physician-paramedic team can achieve high first-pass intubation success rates of over 97%. However, pre-hospital RSI also carries risks and has shown mixed results in studies. To mitigate risks, pre-hospital RSI should follow standardized procedures, utilize proper monitoring, and involve rigorous training through simulation to minimize human error and maximize patient safety.