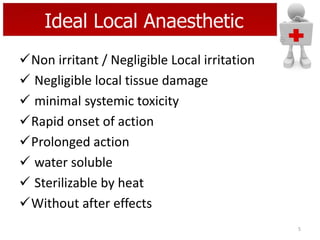
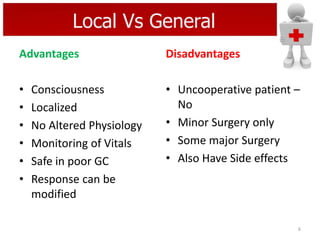
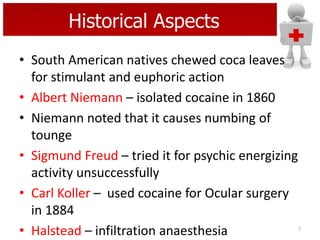
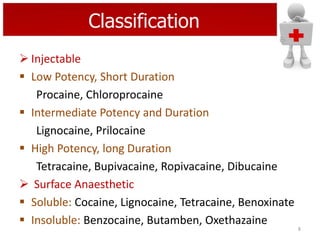
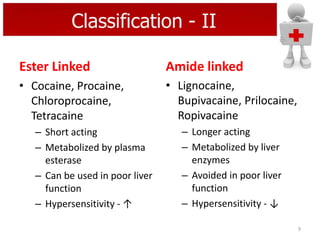
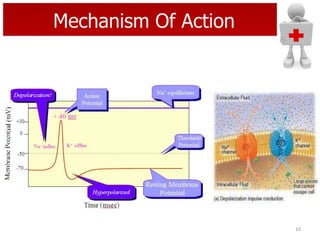
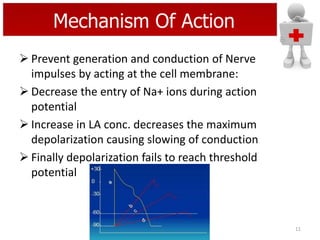
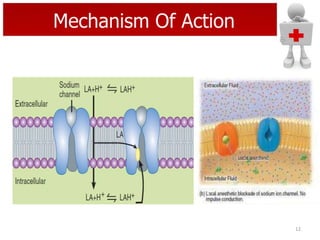
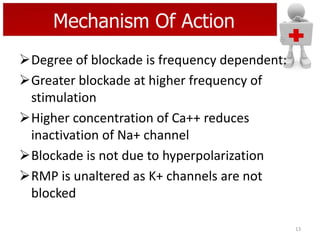
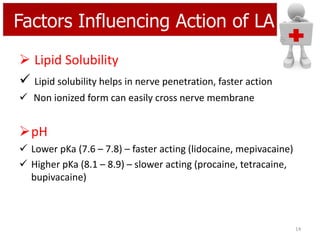
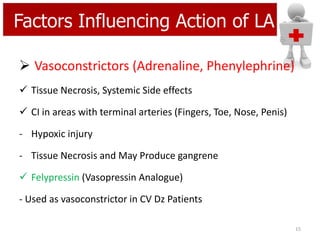
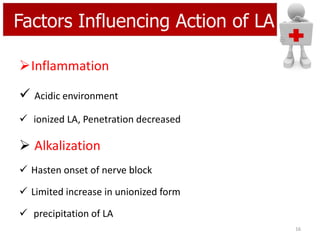
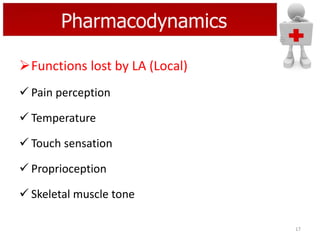
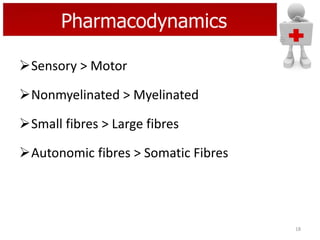
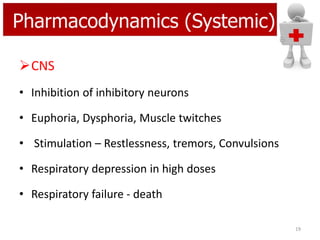
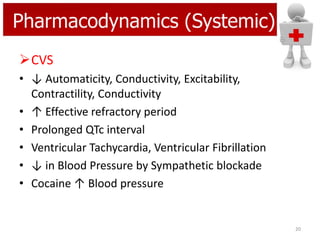
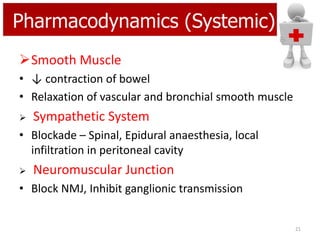
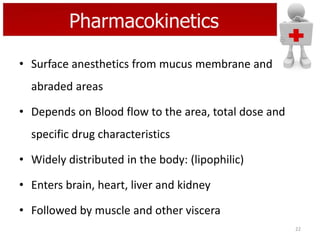
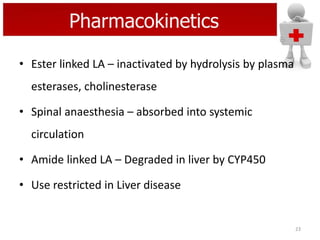
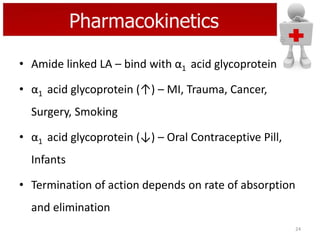
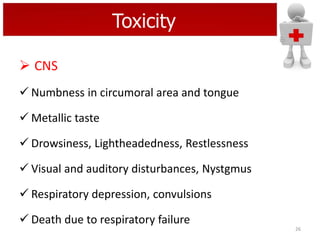
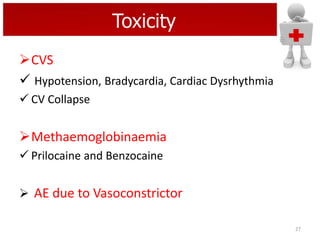
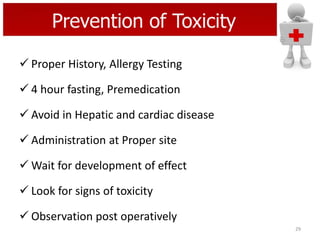
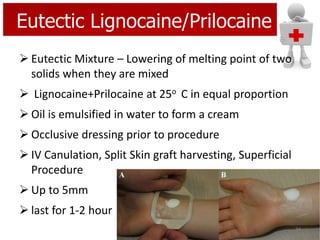
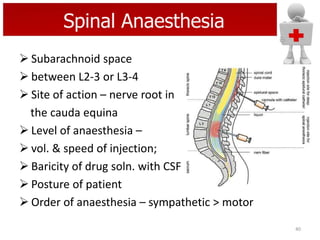
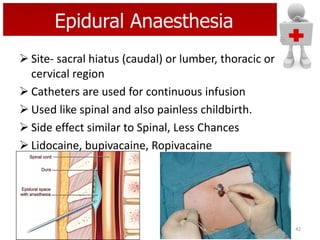
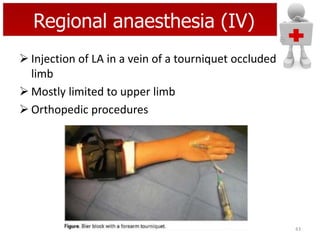
The document discusses local anaesthetics, covering their mechanisms of action, pharmacodynamics, pharmacokinetics, individual agents, and various techniques and uses. It highlights the ideal characteristics of local anaesthetics, classification into ester and amide types, and associated risks, including toxicity and hypersensitivity. Historical aspects and the evolution of local anaesthetic agents are also elaborated, along with their specific applications in medical procedures.