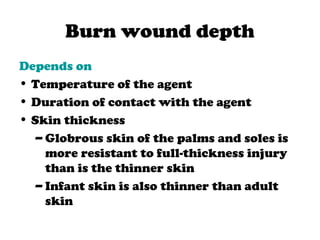
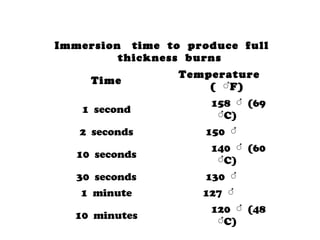
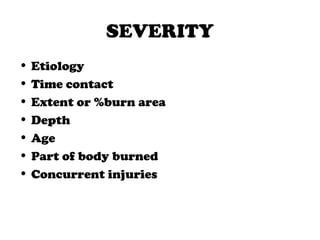
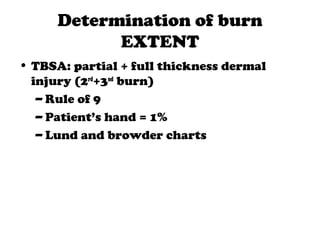
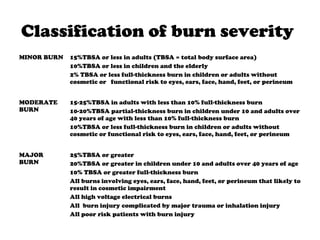
1) Burns are caused by excessive heat or caustic chemicals damaging the skin. Burn severity depends on factors like temperature, duration of contact, extent of burn area, and depth of burn.
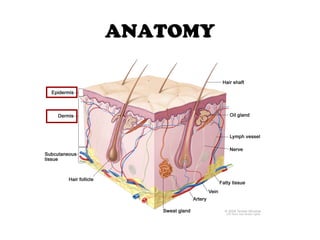
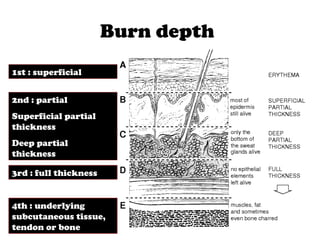
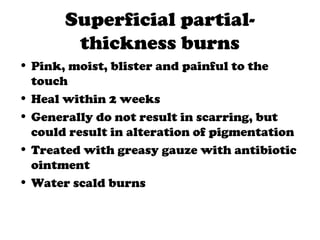
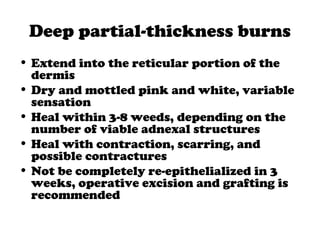
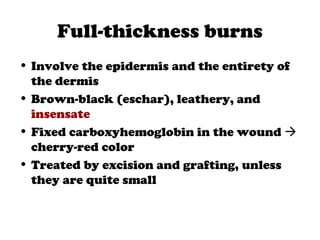
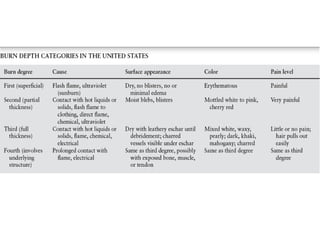
2) Burns are classified by depth - superficial burns involve only the epidermis, partial thickness burns also involve the dermis, and full thickness burns extend through the entire dermis.
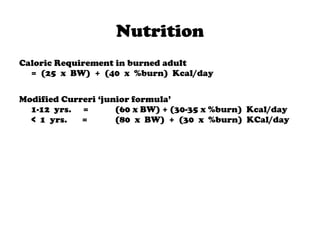
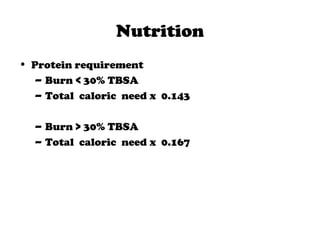
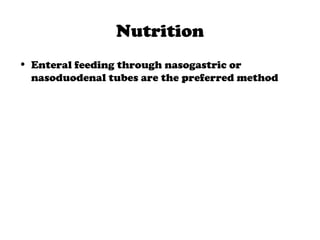
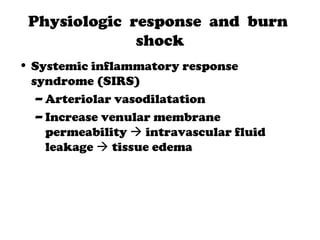
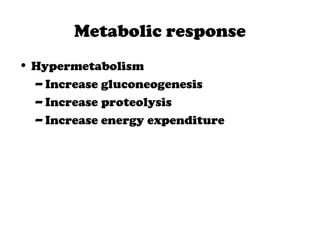
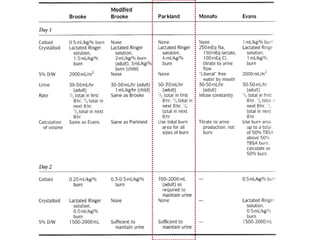
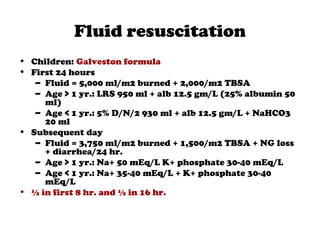
3) Treatment of burns involves initial evaluation, fluid resuscitation to prevent shock, wound care like dressings and possible excision/grafting, adequate nutrition to prevent complications from increased metabolic needs, and managing complications.
![Modification of the Harris-
Benedict Equation
Men
BMR = [66.47 + (13.75 x W) + (5.0 x H) - (6.76 x A) ] x (Activity
factor) x (injury factor)
Women
BMR = [665.1 + (9.56 x W) + (1.85 x H) - (4.68 x A) ] x (Activity
factor) x (injury factor)
BMR = basal metabolic rate W = weight in kg, M = height in cm, A =
age in years
Activity factor
Confined to bed = 1.2
Out of bed = 1.3
Injury factor
Minor operation = 1.2
Skeletal trauma = 1.35
Major sepsis = 1.6
Severe thermal burn = 1.5](https://image.slidesharecdn.com/burn-130610085634-phpapp02/85/Burn-46-320.jpg)