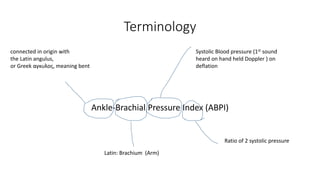
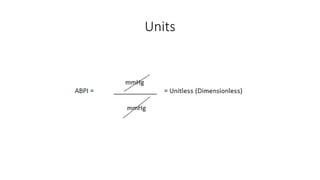
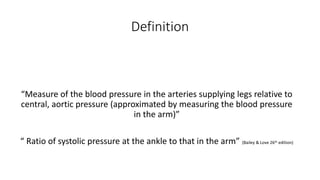
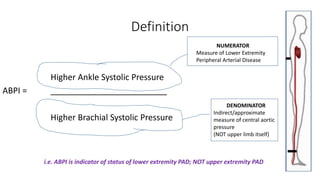
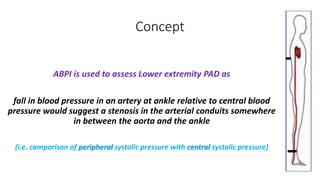
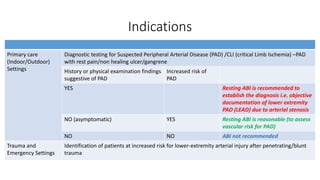
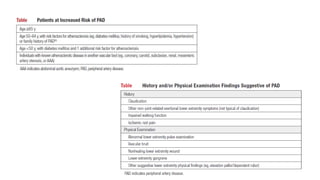
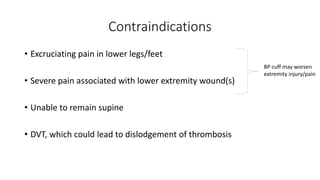
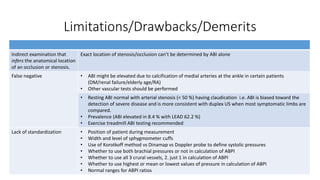
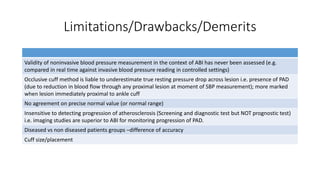
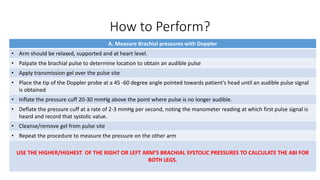
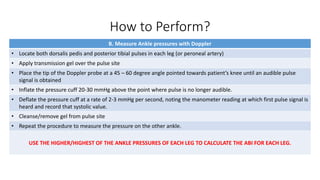
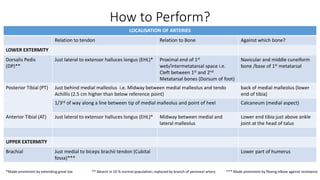
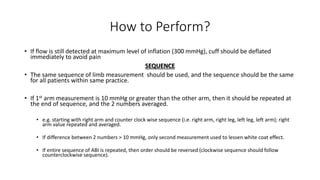
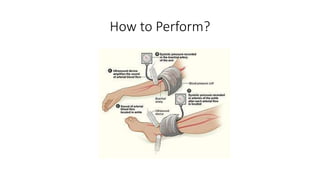
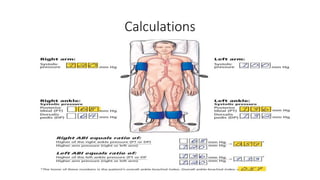
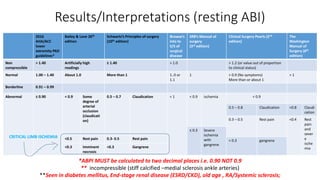
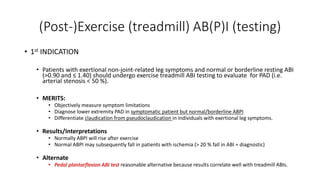
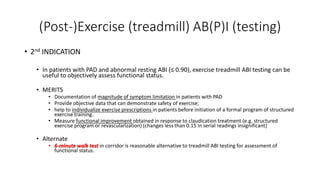
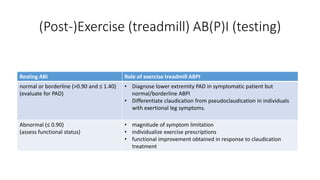
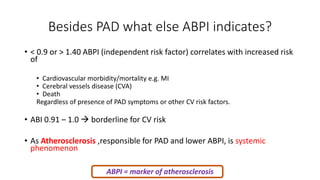
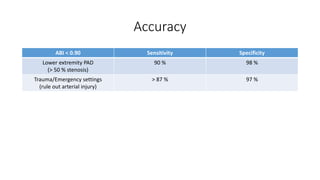
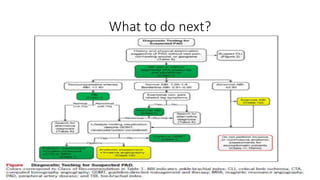
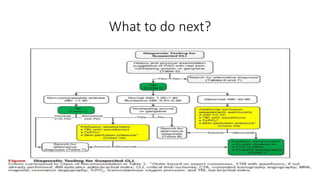
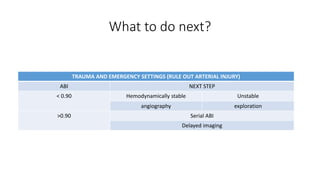
This document provides an overview of ankle-brachial pressure index (ABPI) testing, including definitions, indications, methodology, interpretations, and limitations. ABPI is a non-invasive test that involves measuring the blood pressure in the ankles and arms to calculate a ratio, with ratios below 0.9 indicating peripheral artery disease. The document outlines the equipment, patient positioning, measurement techniques, and calculations required to perform ABPI testing and interpret the results. Limitations include variability in measurements, inability to determine stenosis location, and overestimation in patients with calcified ankle arteries.