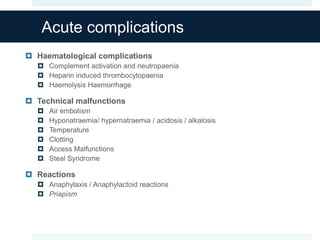
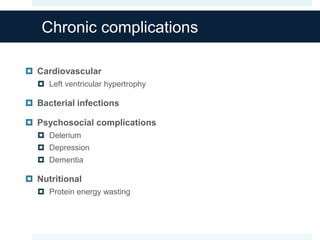
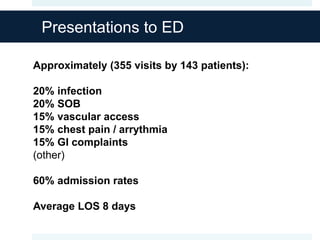
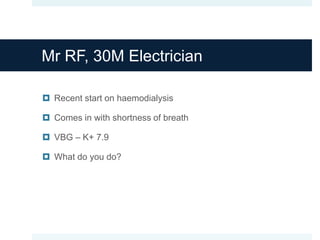
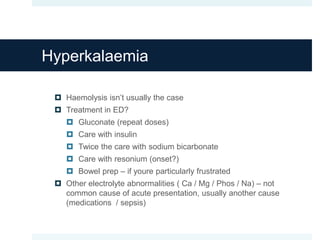
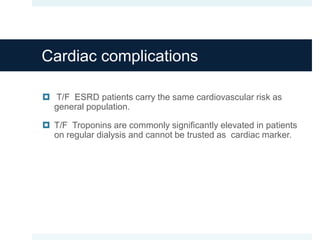
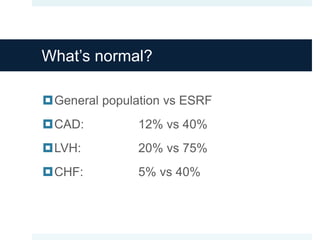
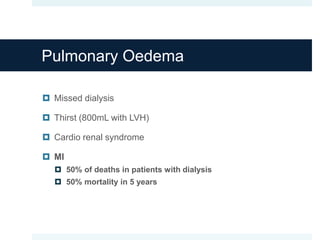
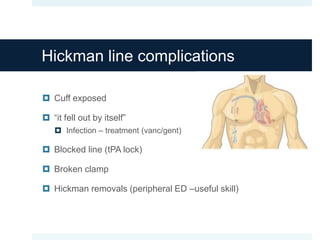
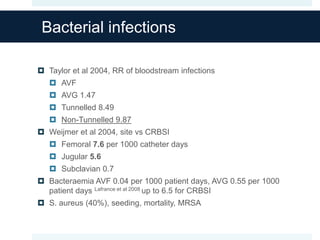
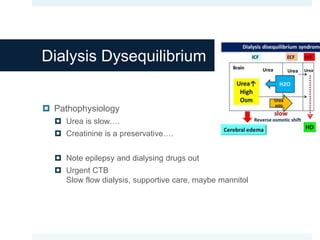
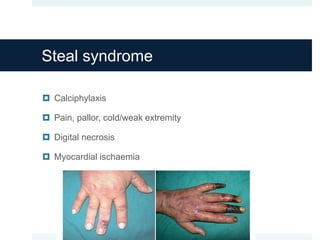
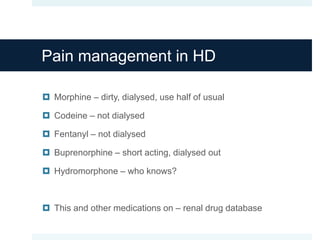
This document discusses renal failure and its complications. It covers acute complications of renal failure including cardiovascular, neuromuscular, hematological, and technical issues during dialysis. Chronic complications include cardiovascular disease and infections. Common presentations to the emergency department for patients with renal failure include infections, shortness of breath, vascular access issues, chest pain, and gastrointestinal complaints. Several case examples are provided to discuss management of specific complications like hyperkalemia, pulmonary edema, cardiac issues, bleeding, and infections.