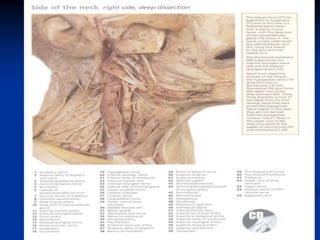
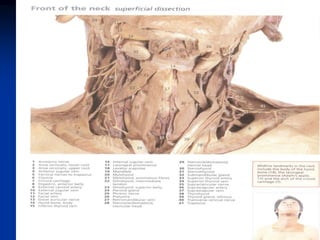
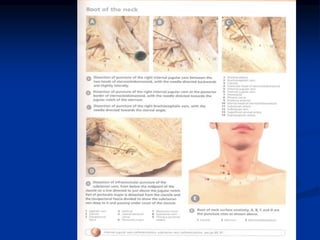
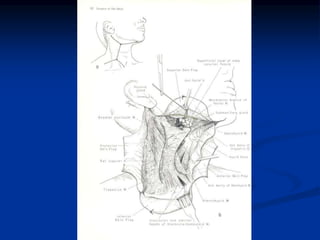
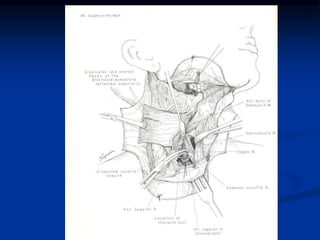
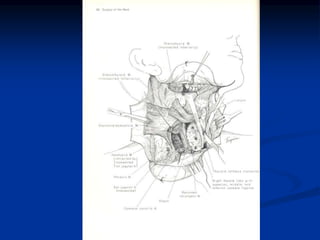
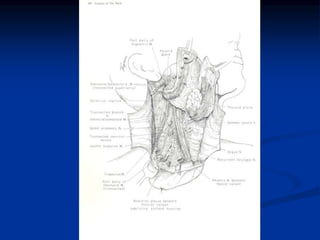
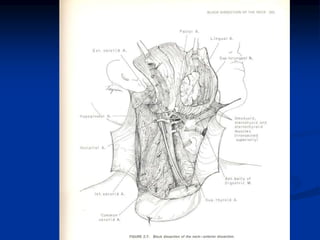
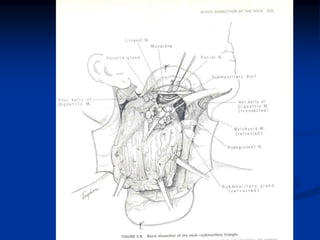
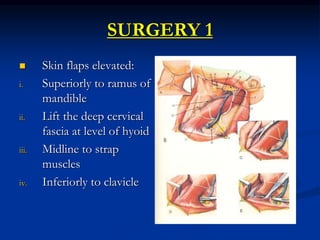
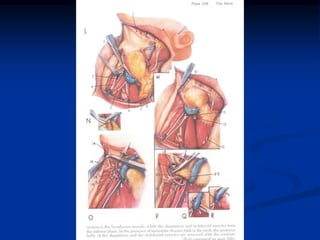
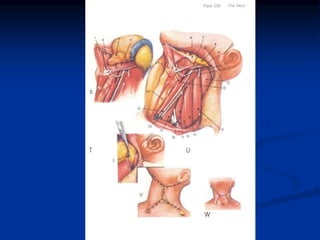
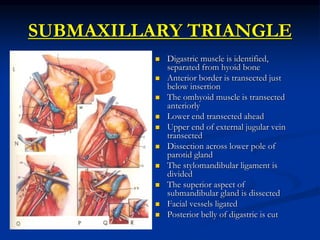
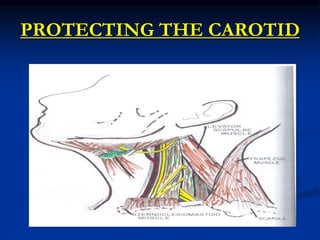
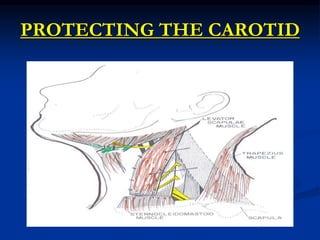
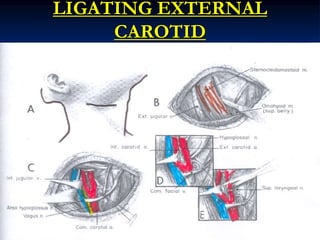
Elevate the skin flaps superiorly to the level of the ramus of mandible. Identify and protect the external jugular vein.
Surgeon: Okay, elevating the skin flaps now. Carefully dissecting in the plane just deep to the platysma muscle. There's the external jugular vein, I'm protecting that as I elevate the flap. Almost to the level of the ramus now.