This document discusses several important aspects of the doctor-patient relationship, including:
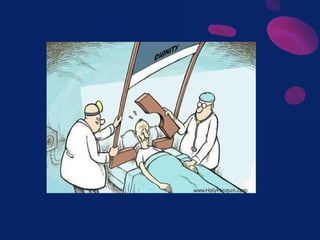
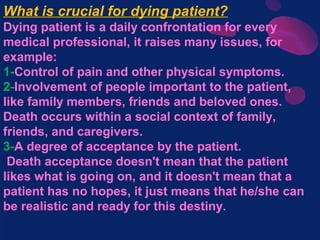
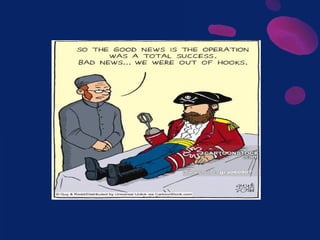
1) Doctors have a duty to act in their patients' best interests according to ethical principles. An effective relationship requires respect, understanding, and trust between doctors and patients.
2) Factors like mutual understanding, clear guidelines for care options, comfort during illness, and open discussion even during uncertainty are important.
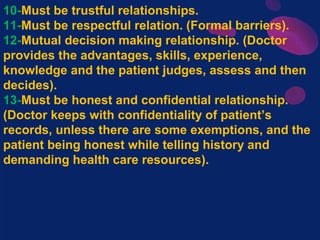
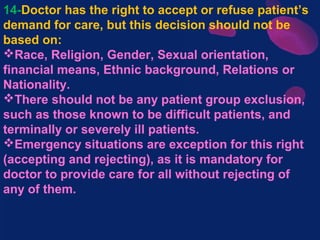
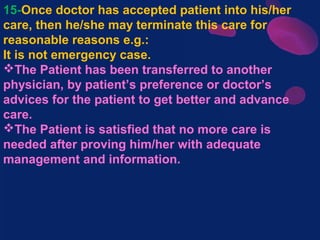
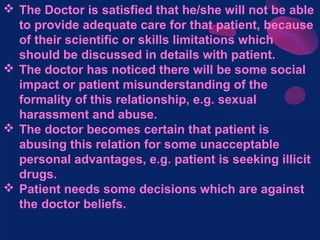
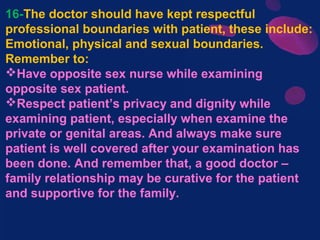
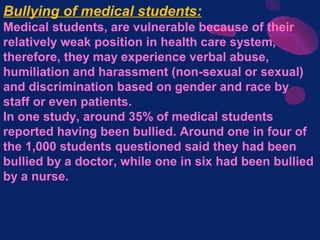
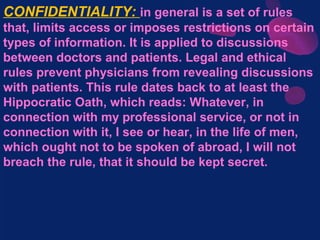
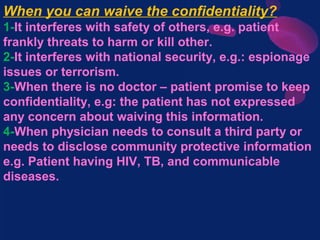
3) The relationship must maintain patient confidentiality, honesty, and informed mutual decision-making while avoiding discrimination, abuse, or neglect. Terminating a relationship requires reasonable cause and respecting professional boundaries is important.