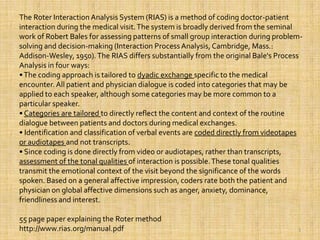
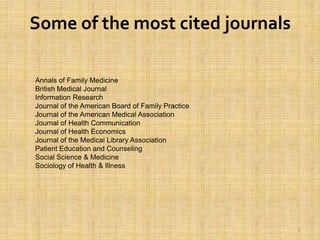
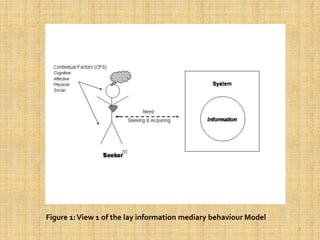
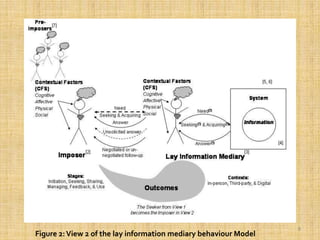
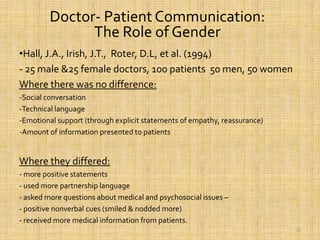
This document discusses doctor-patient communication and interactions. It provides an overview of some of the most cited authors on this topic, including DiMatteo, Hall, Kaplan, and Roter. It describes the Roter Interaction Analysis System (RIAS), a method for coding doctor-patient interactions. The document also lists some of the most cited journals on this subject and discusses lay information mediaries, models of mediary behavior, and methods used to study doctor-patient communication such as observational scales.