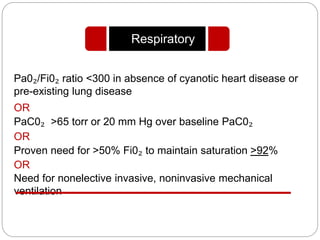
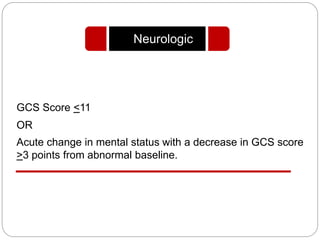
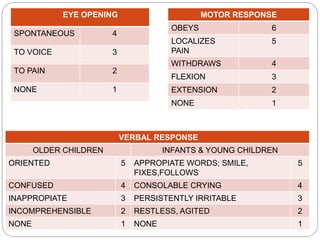
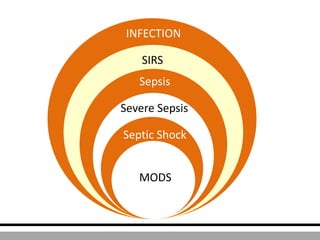
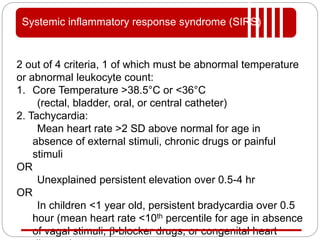
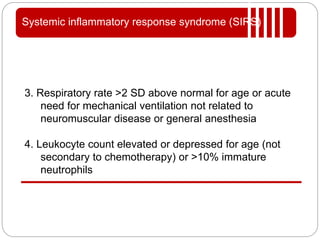
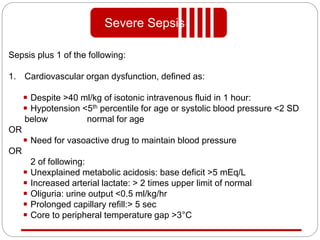
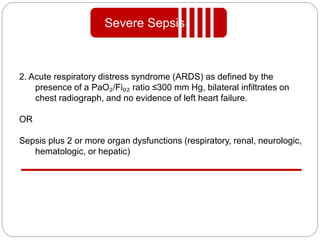
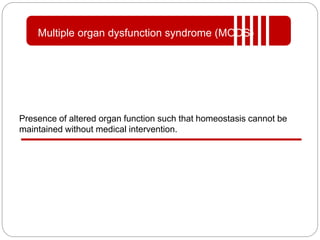
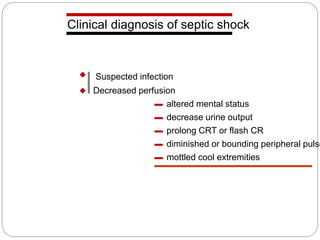
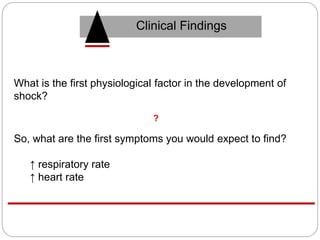
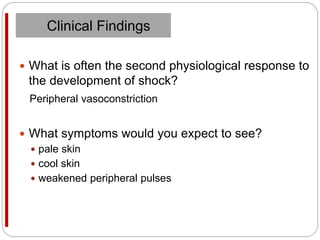
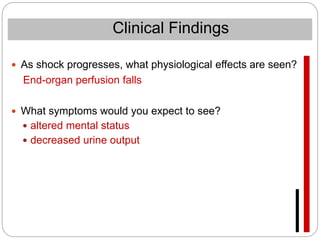
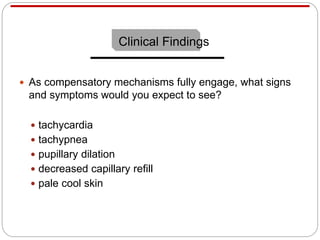
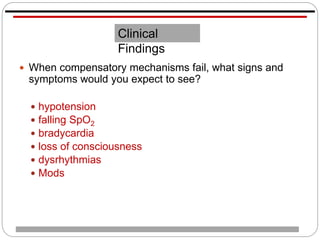
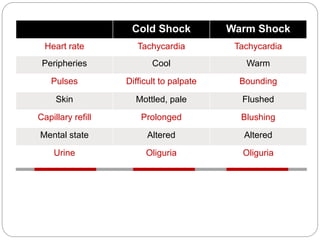
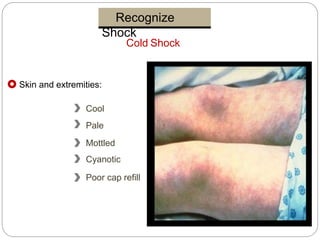
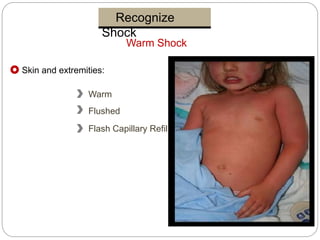
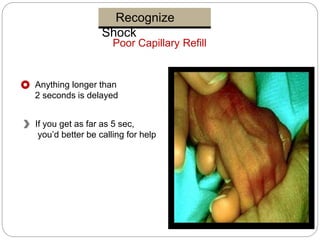
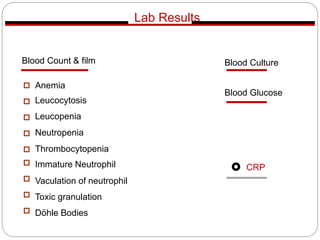
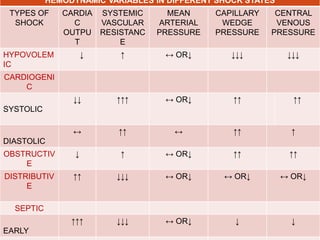
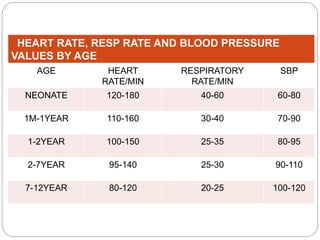
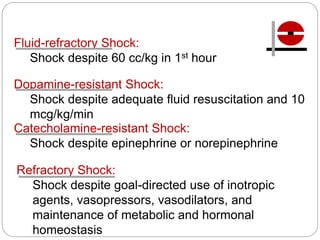
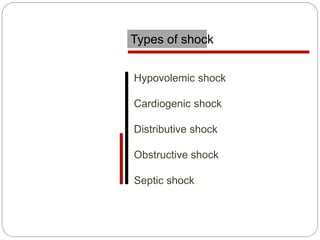
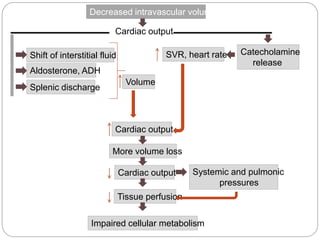
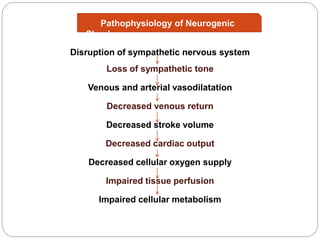
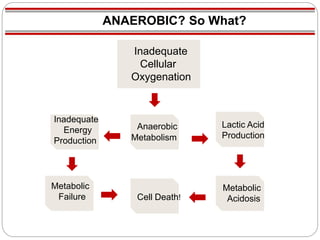
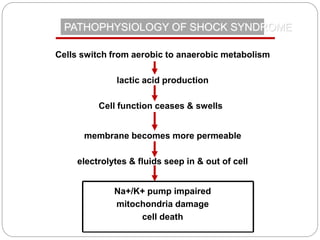
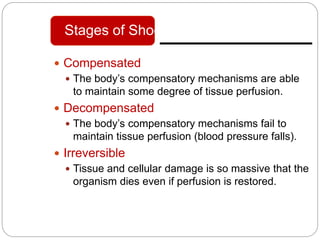
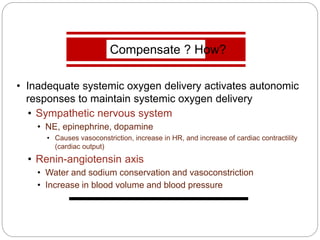
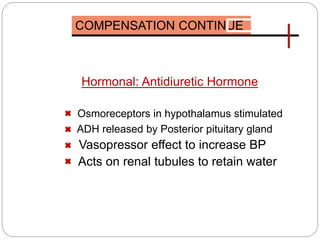
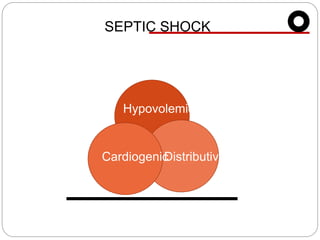
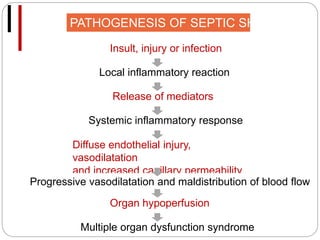
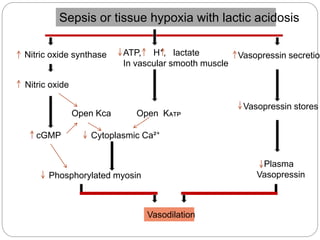
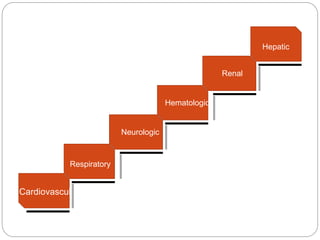
The document presents an extensive overview of shock, including its definition, types (hypovolemic, cardiogenic, distributive, obstructive, and septic shock), and pathophysiology. It describes the compensatory mechanisms the body engages to maintain tissue perfusion, as well as the progression from compensated to irreversible shock. Key clinical findings and criteria for diagnosing shock and multiple organ dysfunction syndrome (MODS) in pediatric patients are also detailed.

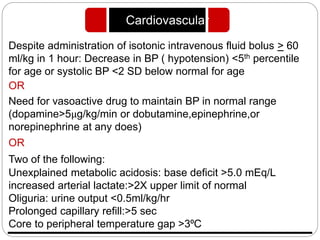
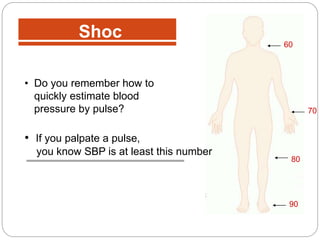
![MAP <5th PERCENTILE FOR AGE
LOWEST ACCEPTABLE SBP = 70 + [2x AGE IN YEARS]
AGE LOWEST ACCEPTABLE SBP
TERM NEONATE 60
INFANT 1-12 MONTHS 70
CHILDREN 1-10 YRS 70 +[2x AGE IN YEARS]
CHILDREN >10 YRS 90
HYPOTENSION](https://image.slidesharecdn.com/shock-150130114557-conversion-gate01/85/Shock-and-it-s-classification-20-320.jpg)