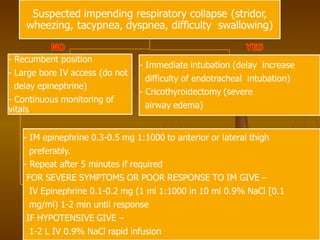
This document provides an overview of shock, including definitions, classifications, causes, pathophysiology, signs and symptoms, diagnosis, and management. It discusses the main types of shock: hypovolemic, cardiogenic, distributive (septic), and obstructive. For each type, it outlines the etiology, pathophysiology, clinical presentation, evaluation and treatment. It provides detailed information on septic shock, including terminology, recognition of early vs. late septic shock, diagnostic criteria involving general, inflammatory, hemodynamic and organ dysfunction variables, and definitions of severe sepsis. The document aims to comprehensively review shock for medical education purposes.