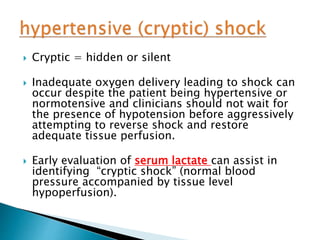
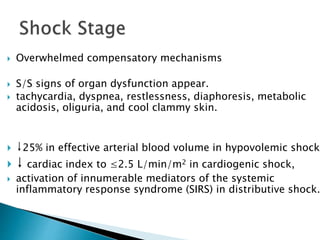
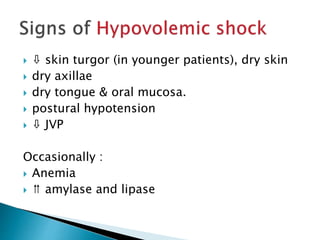
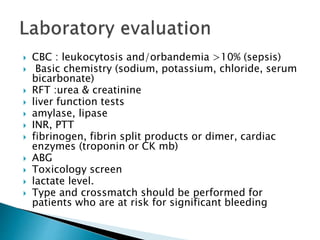
This document discusses shock, defined as a significant reduction in systemic tissue perfusion and oxygen delivery. Shock results in cell membrane and organ dysfunction, which can progress to multi-system organ failure and death if not reversed. The causes of shock include hypovolemia, cardiogenic, and distributive origins. Early goal-directed resuscitation is important to restore perfusion before end-organ damage becomes irreversible. A thorough history, physical exam, and initial lab tests can help identify underlying causes but definitive diagnosis may require further testing.