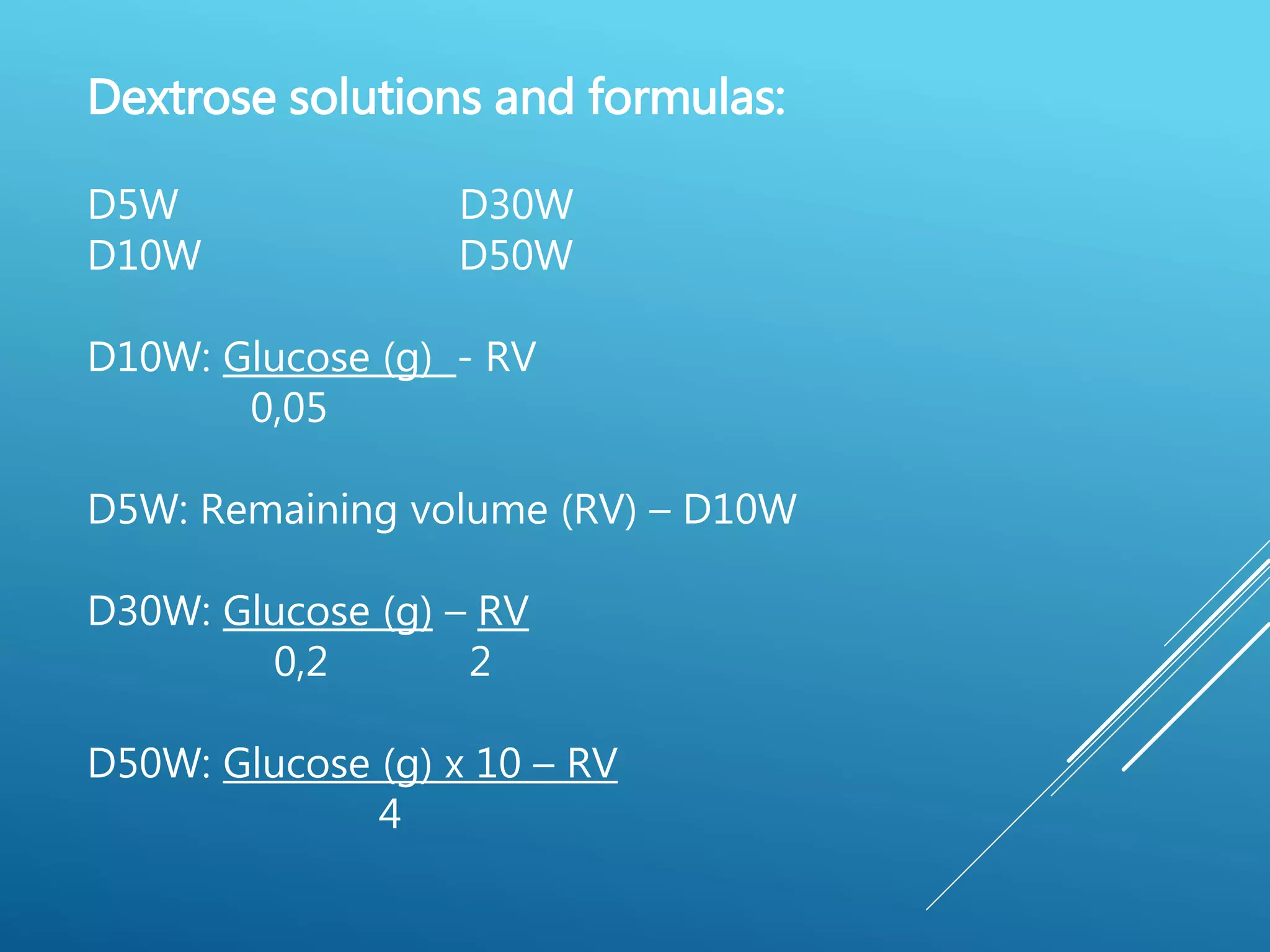
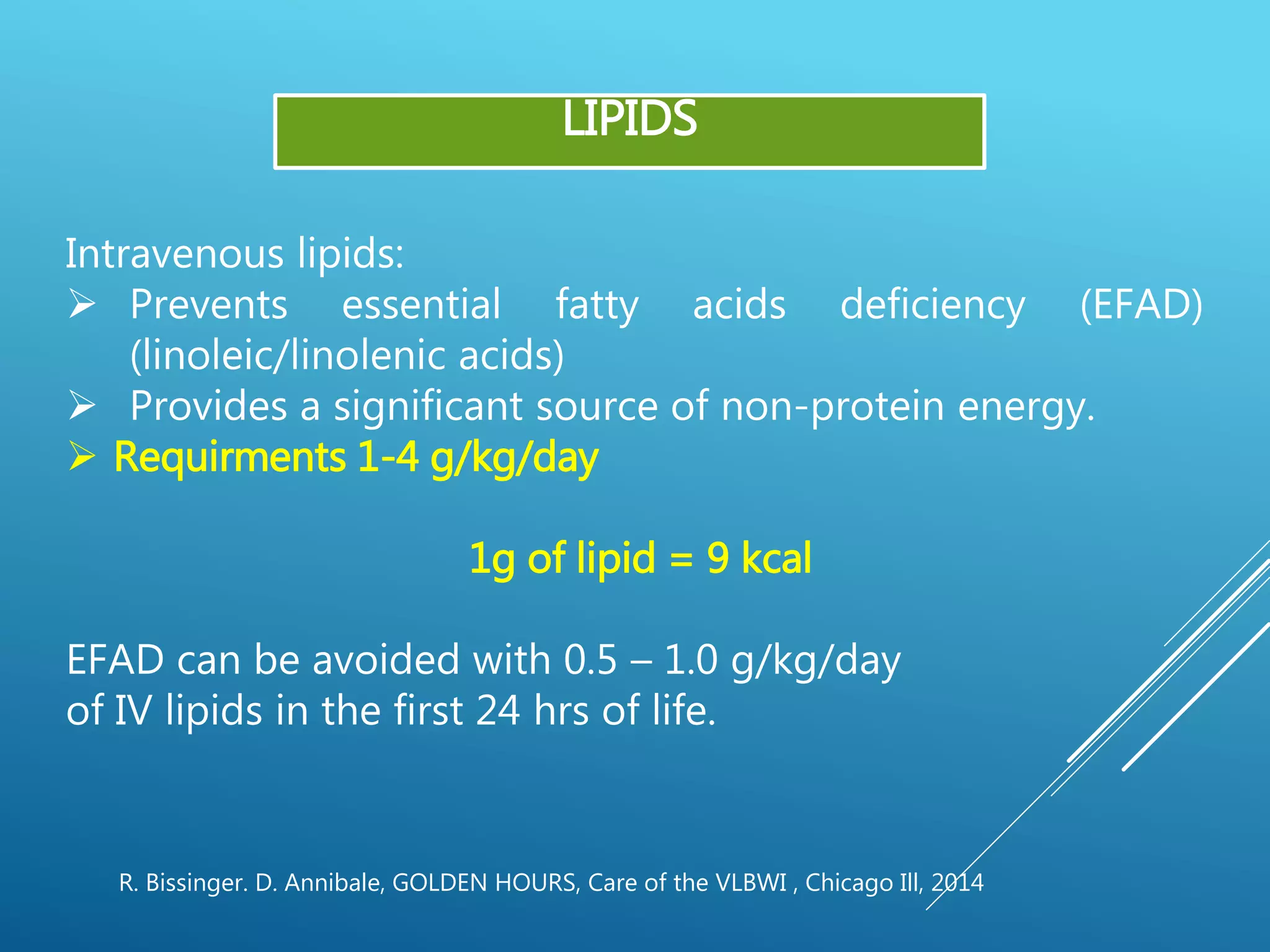
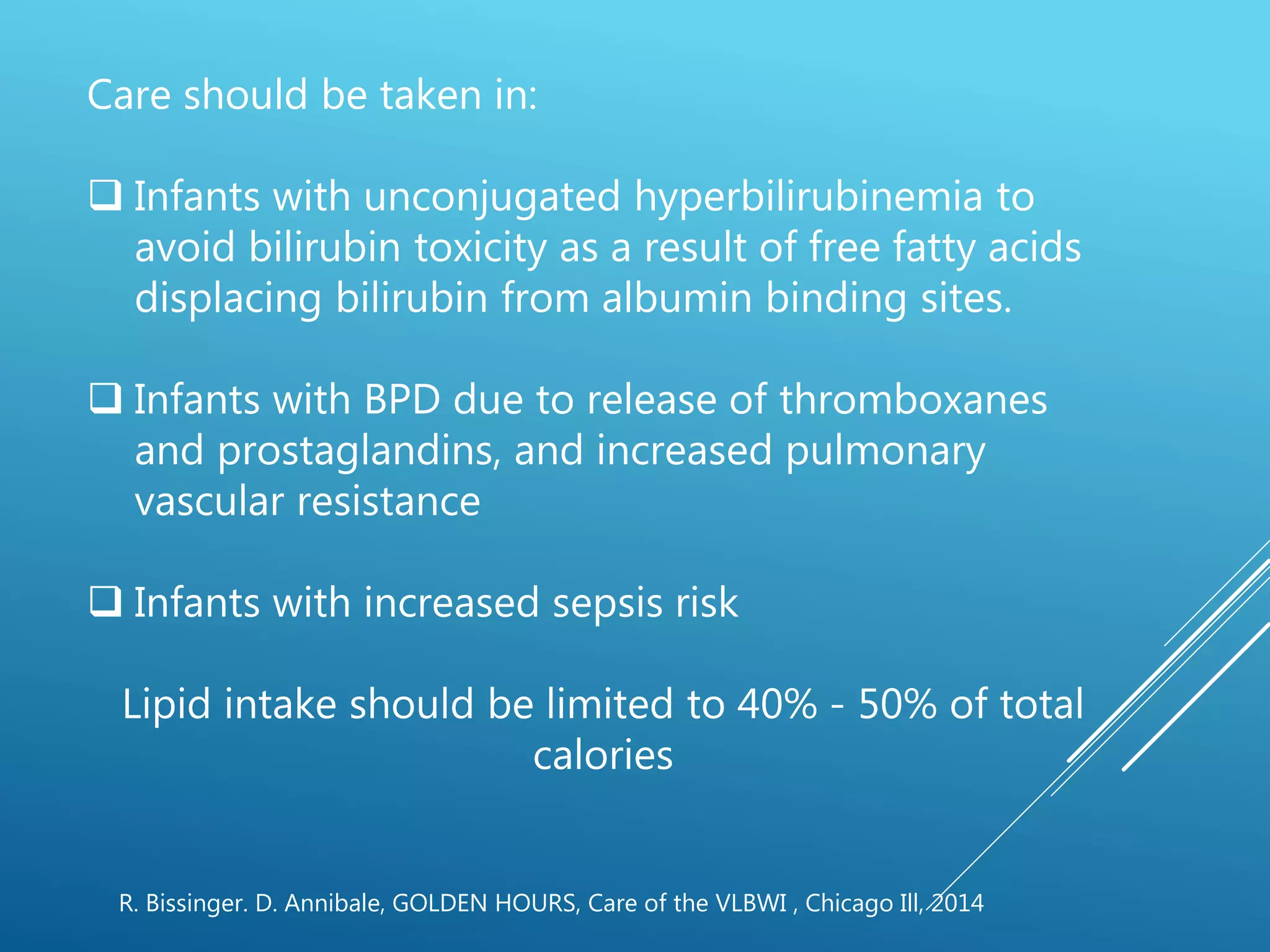
This document discusses parenteral nutrition in newborns. It defines key terms like total body water and insensible water loss. It provides guidelines for fluid, glucose, amino acid, lipid and electrolyte requirements for very low birth weight infants. Close monitoring of electrolytes and renal function is important when providing parenteral nutrition to newborns.