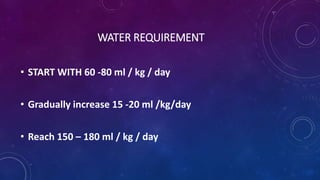
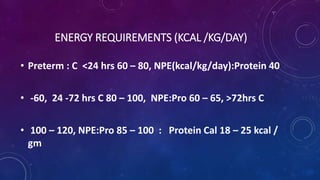
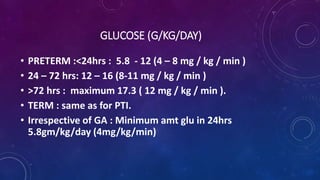
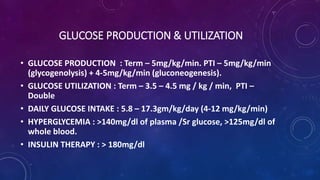
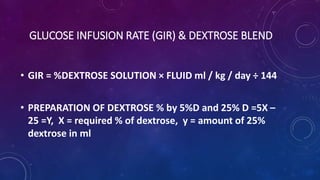
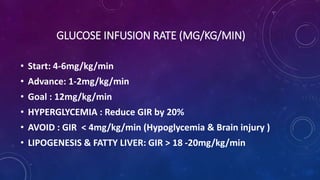
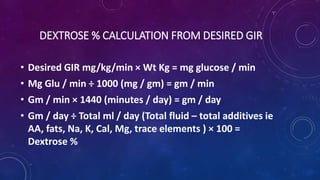
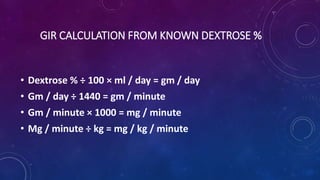
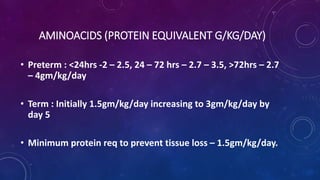
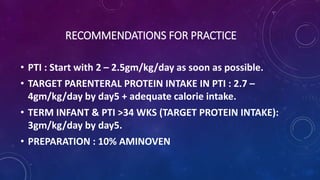
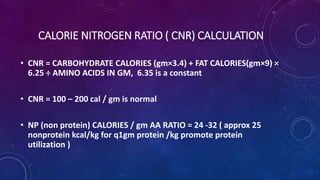
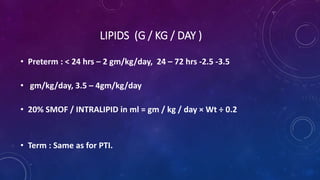
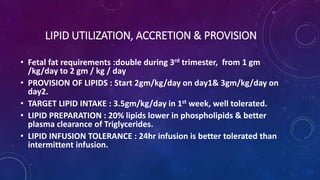
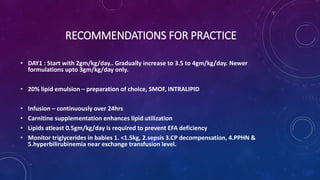
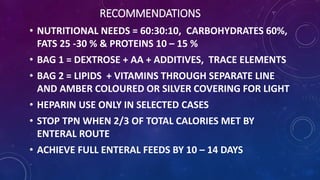
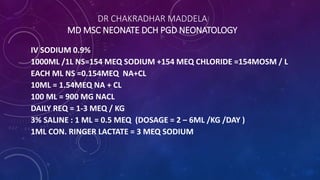
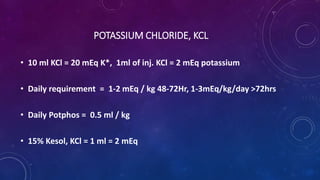
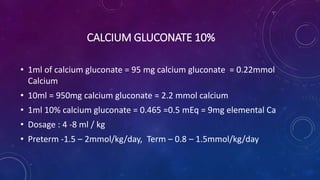
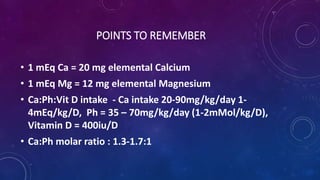
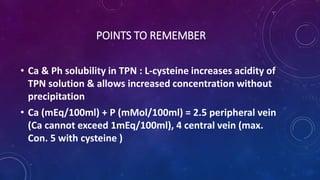
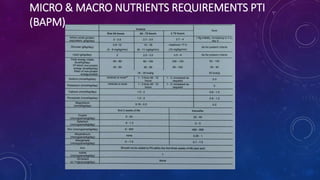
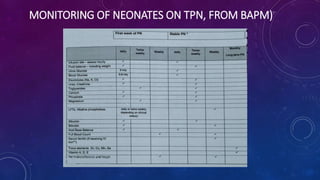
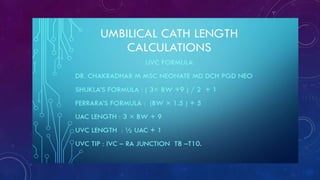
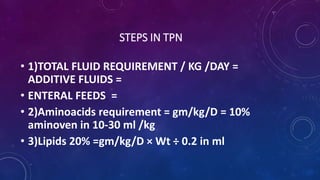
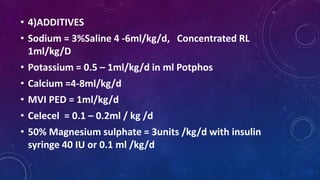
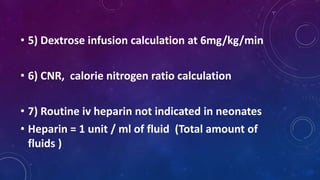
Dr. Chakradhar Maddela provides comprehensive guidelines on nutritional requirements for term and preterm infants, focusing on total parenteral nutrition (TPN), including specific recommendations for fluid, energy, glucose, protein, and lipid intake. The document details how to calculate glucose infusion rates, amino acid and lipid administration, and the importance of monitoring for potential complications like hyperglycemia and fatty liver. Recommendations for practice emphasize starting TPN promptly, achieving full enteral feeds within 10 to 14 days, and ensuring appropriate macro and micronutrient intake.