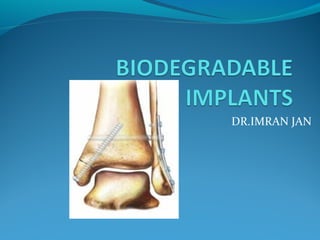
This document discusses biodegradable implants and their use in orthopedic surgery. It provides details on:
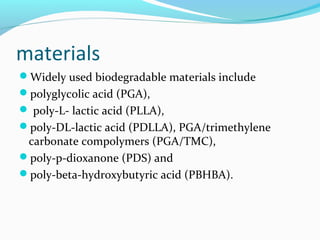
- Common biodegradable materials used like PGA, PLLA, PDLLA which degrade over time in the body from 1-6 months.
- Their applications include fixation of fractures, ligament surgery, and drug/growth factor delivery.
- Advantages are that removal surgery is not needed but disadvantages are they are typically more expensive and weaker than metals.
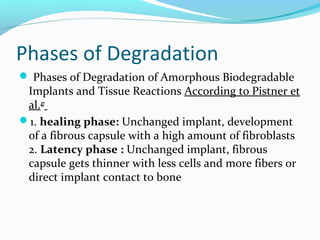
- The degradation process involves hydrolysis breaking down the implant into fragments which are then absorbed.