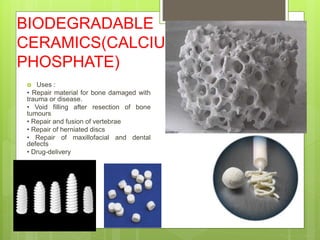
Biodegradable implants are made of materials like polyglycolic acid and polylactic acid that degrade over time and are absorbed by the body, eliminating the need for removal surgery. Such implants have been used since the 1960s and are increasingly used in orthopedic procedures of the knee, shoulder, spine, foot and ankle to fix fractures and injuries. While they avoid long-term complications of metallic implants, biodegradable implants may cause delayed inflammatory reactions and currently do not provide as rigid of a fixation as metals. Researchers continue working to develop biodegradable implants that degrade at optimized timeframes and can be used for a wider range of fractures and procedures.