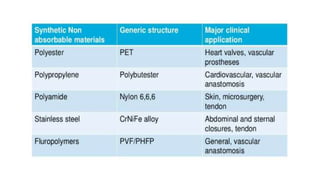
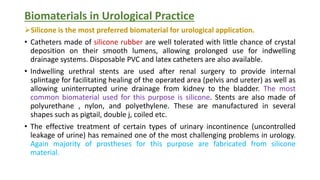
This document discusses various soft tissue applications of biomaterials. It begins by defining soft tissues and listing minimal requirements for soft tissue implant materials. It then describes five main categories of implants: shunts, percutaneous devices, space fillers, load carriers/scaffolds, and electrodes. The document goes on to discuss specific types of implants in more detail, including bulk space fillers, functional load-carrying implants, sutures, wound dressings, tissue adhesives, percutaneous devices, and biosensors. It concludes by covering biomaterials applications in urological practice such as catheters, stents, and implants for urinary incontinence.