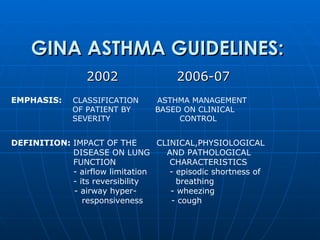
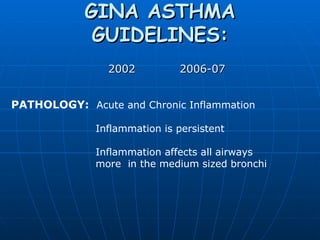
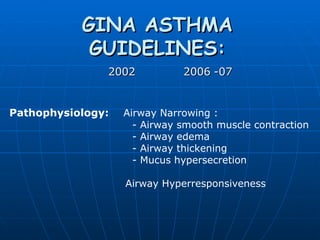
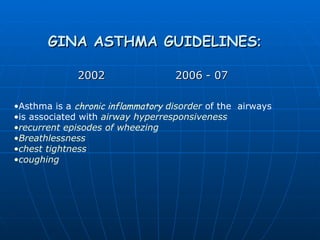
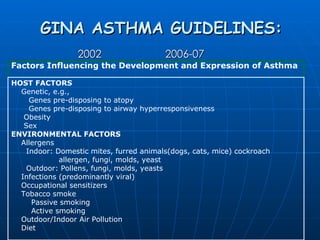
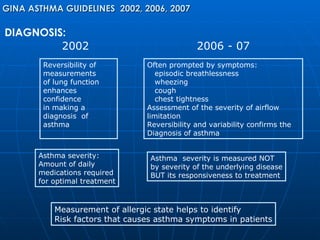
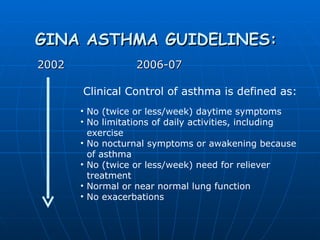
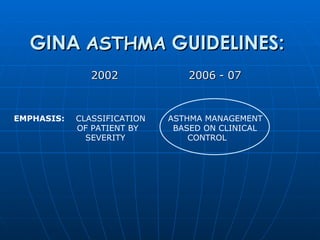
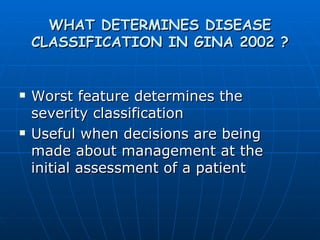
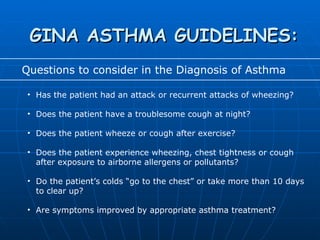
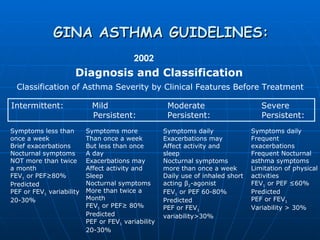
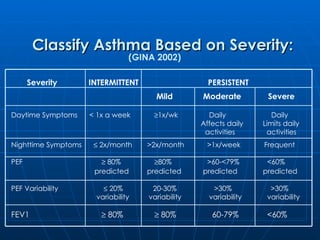
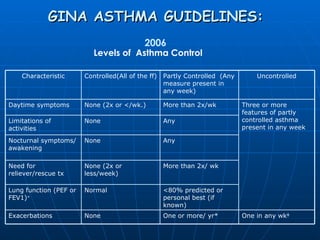
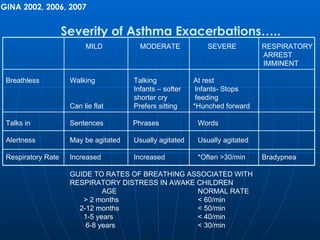
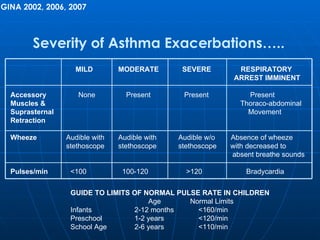
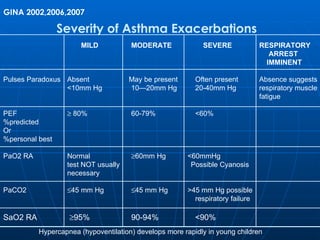
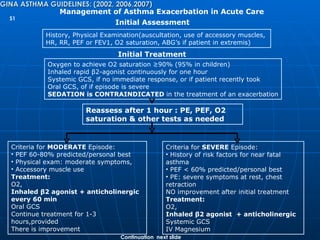
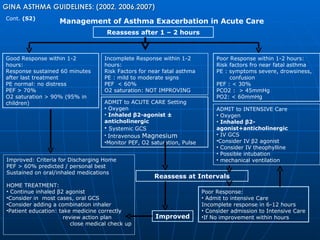
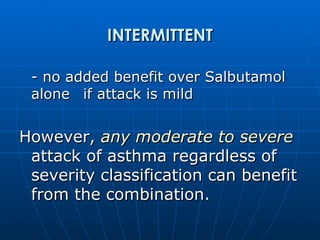
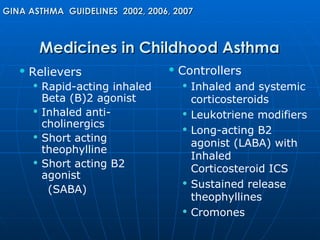
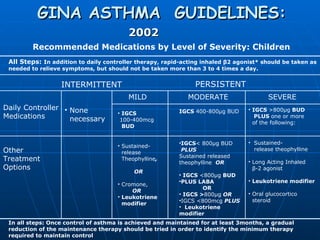
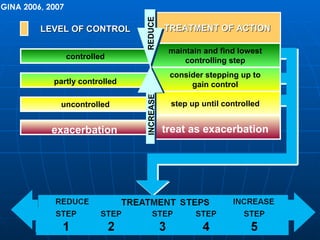
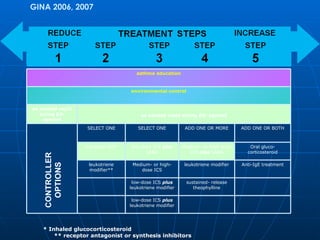
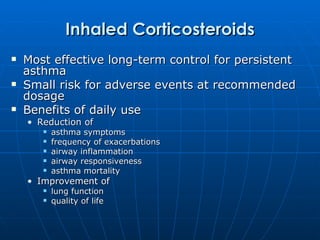
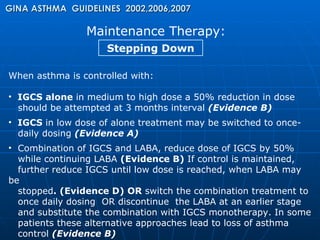
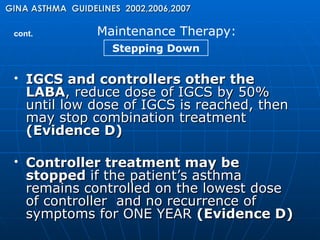
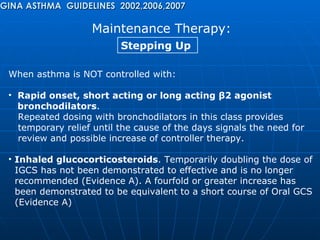
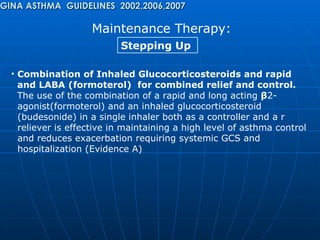
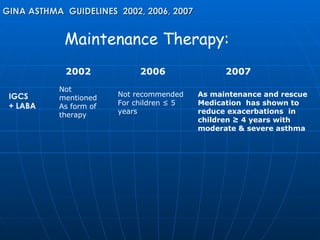
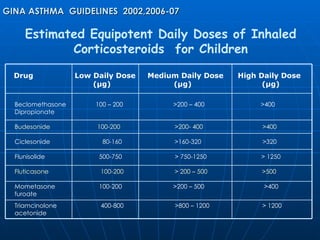
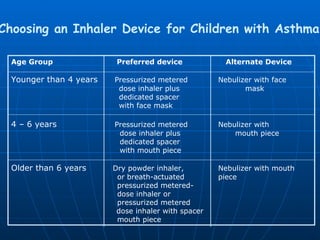
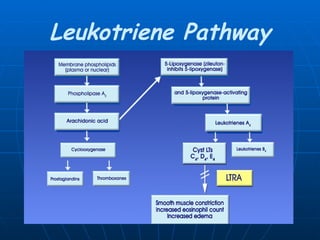
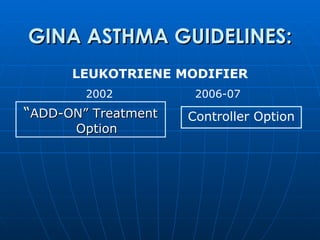
The document summarizes guidelines from the Global Initiative for Asthma (GINA) from 2002, 2006, and 2007. The key changes between the guidelines were a shift from classifying asthma severity based on clinical features to classifying control based on impairment. The 2002 guidelines emphasized classifying patients by severity determined by symptoms, lung function, and medication use. The 2006-2007 guidelines emphasized classifying asthma based on level of control determined by impairment and risk of exacerbations. Both guidelines provided recommendations for diagnosis, treatment including medications, and management of exacerbations.