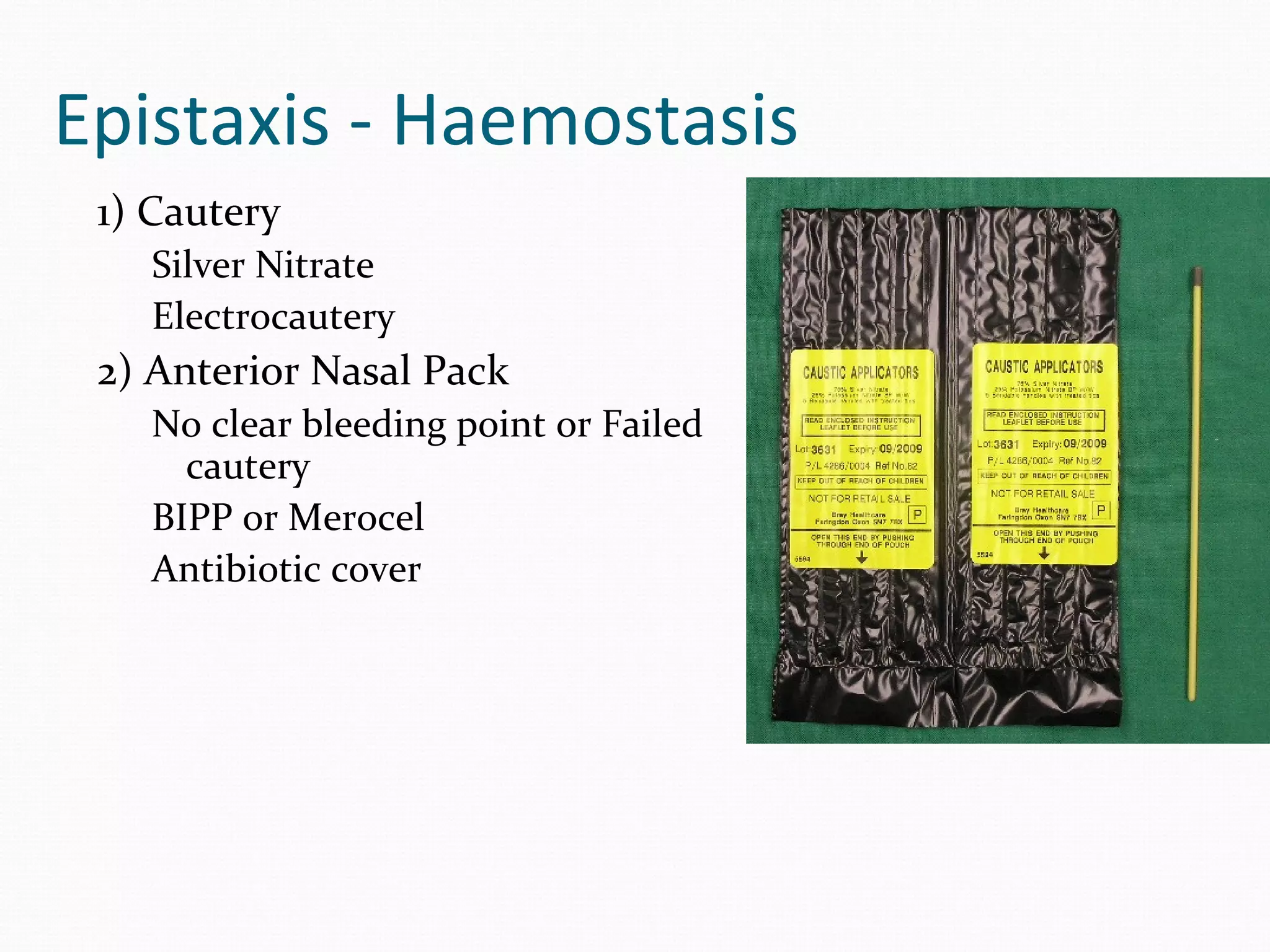
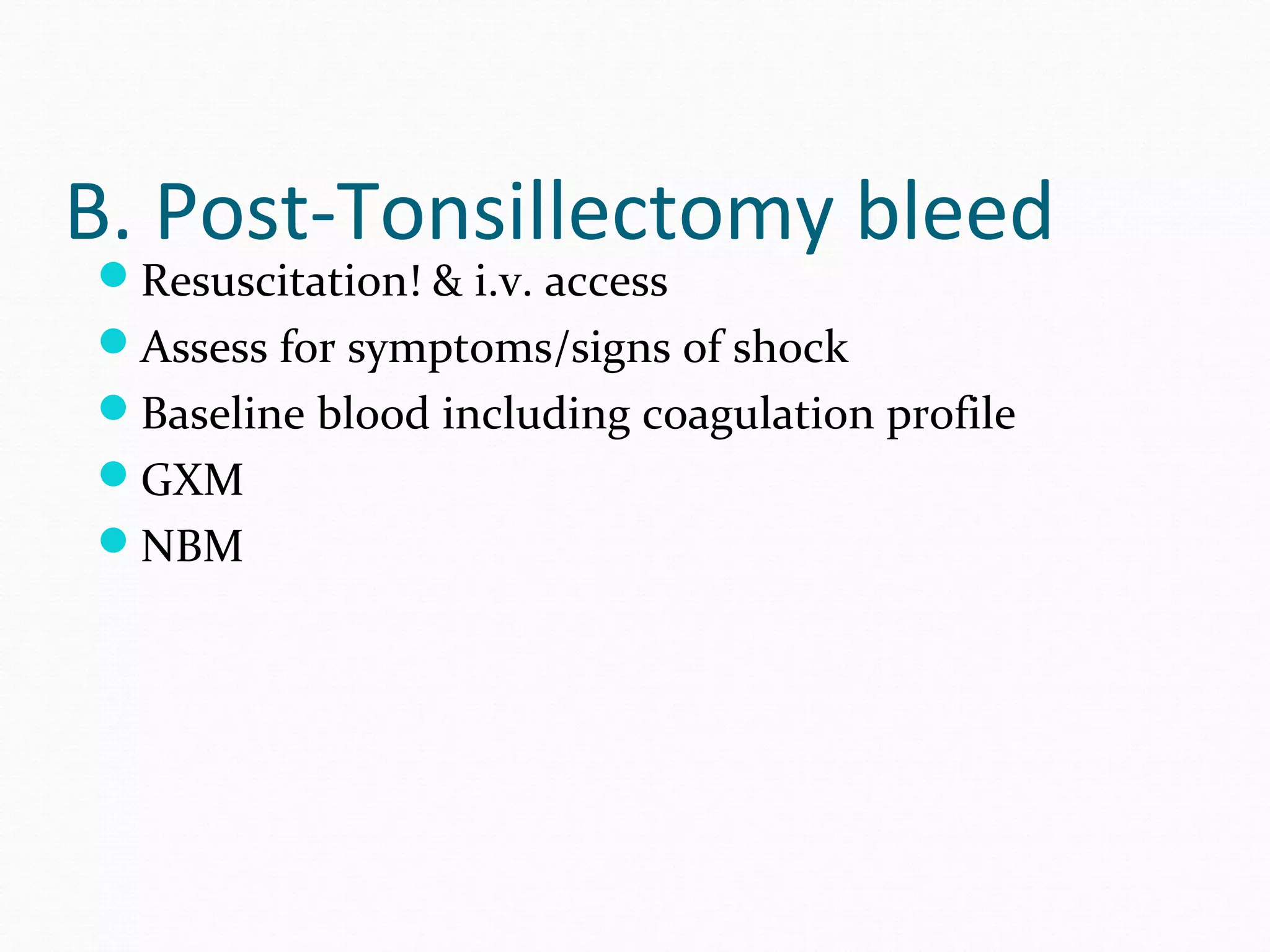
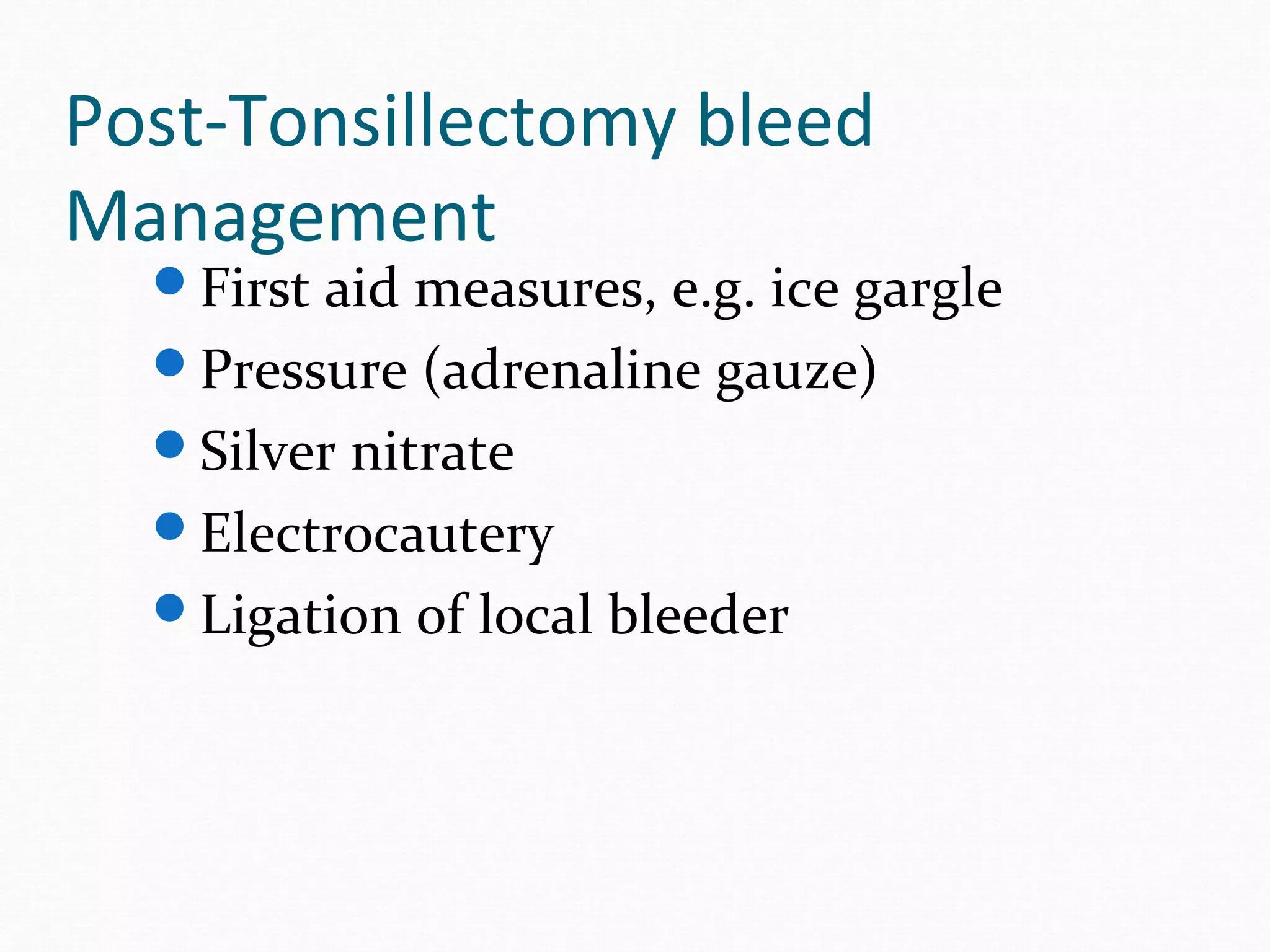
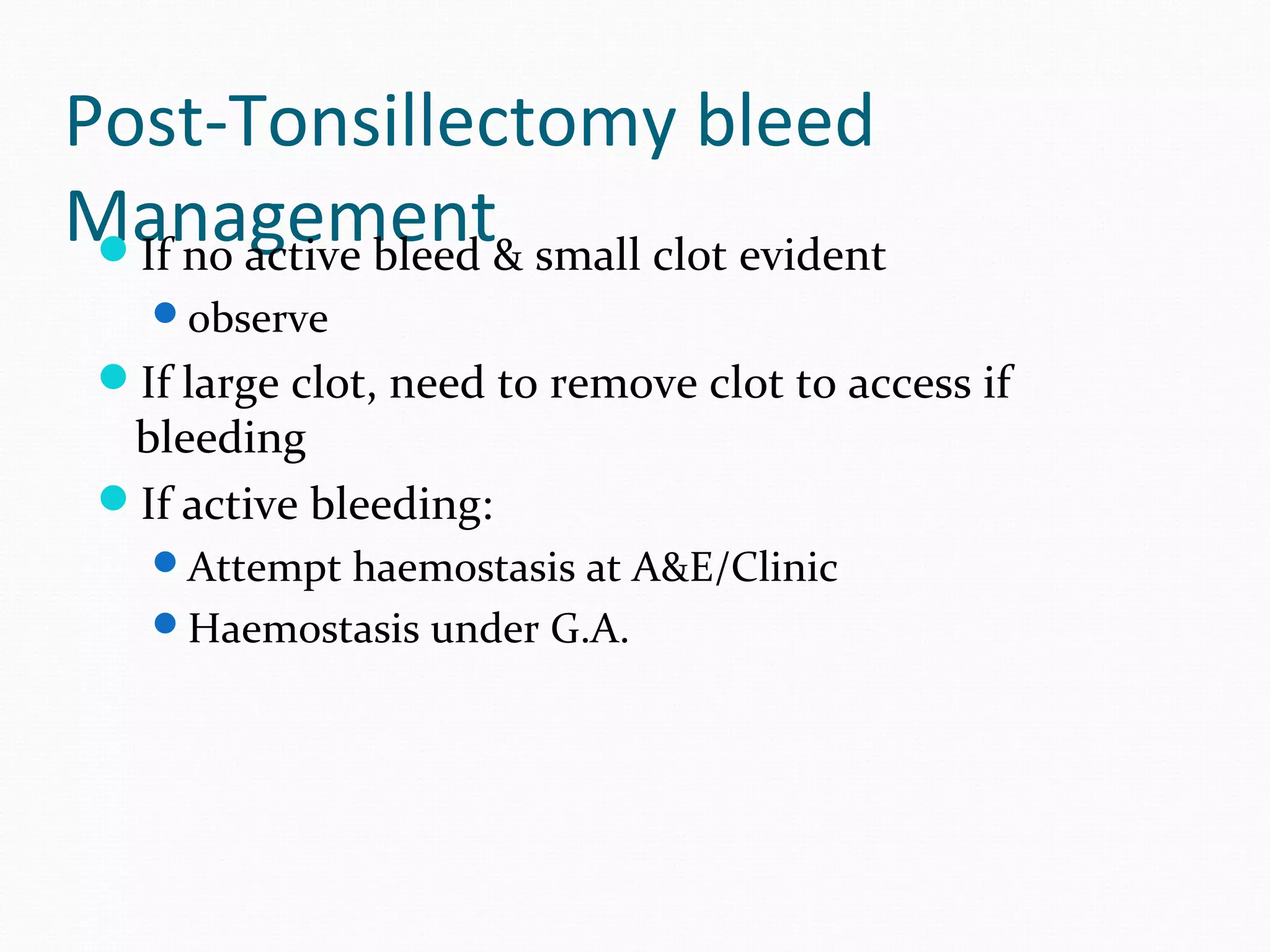
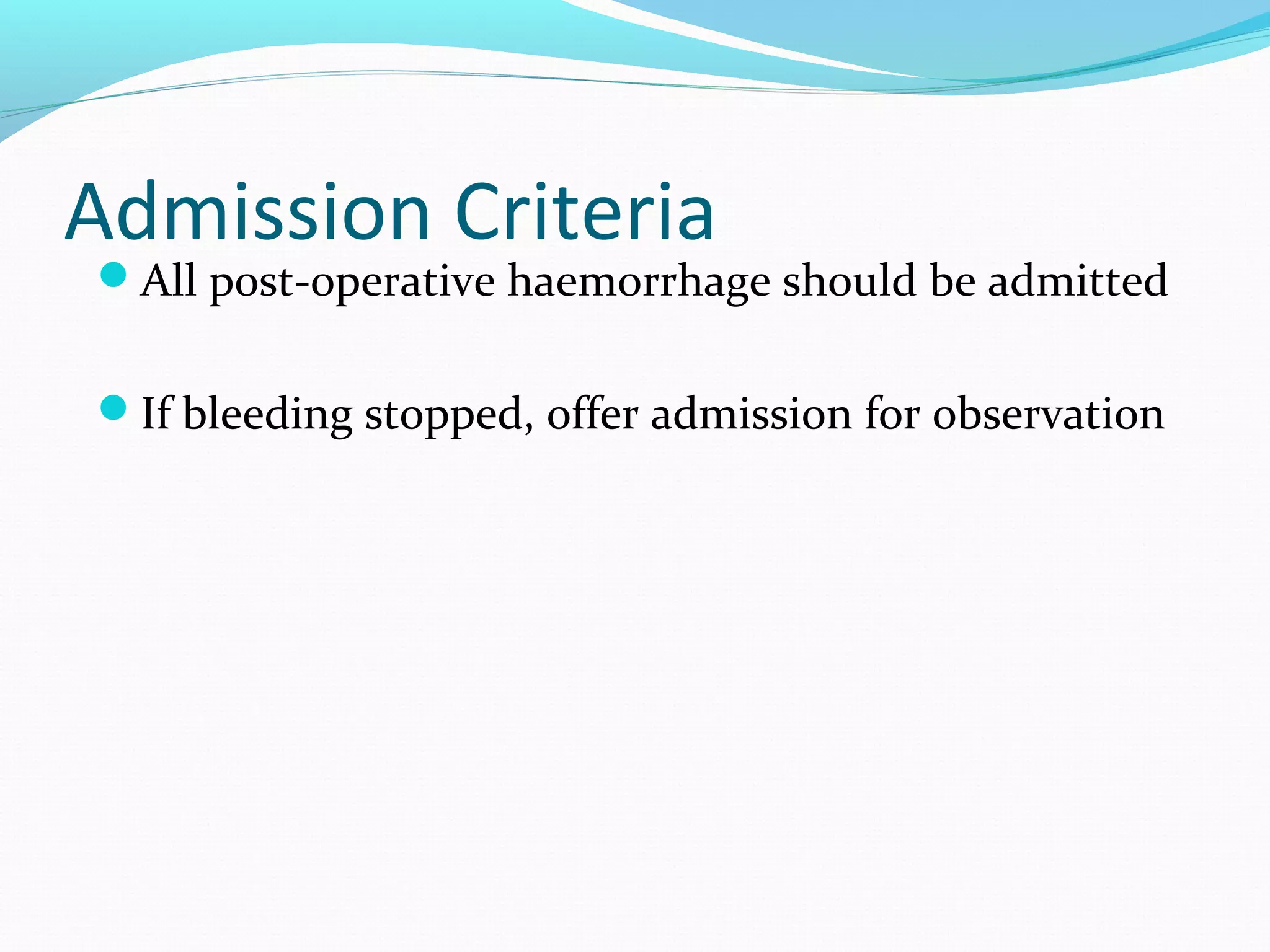
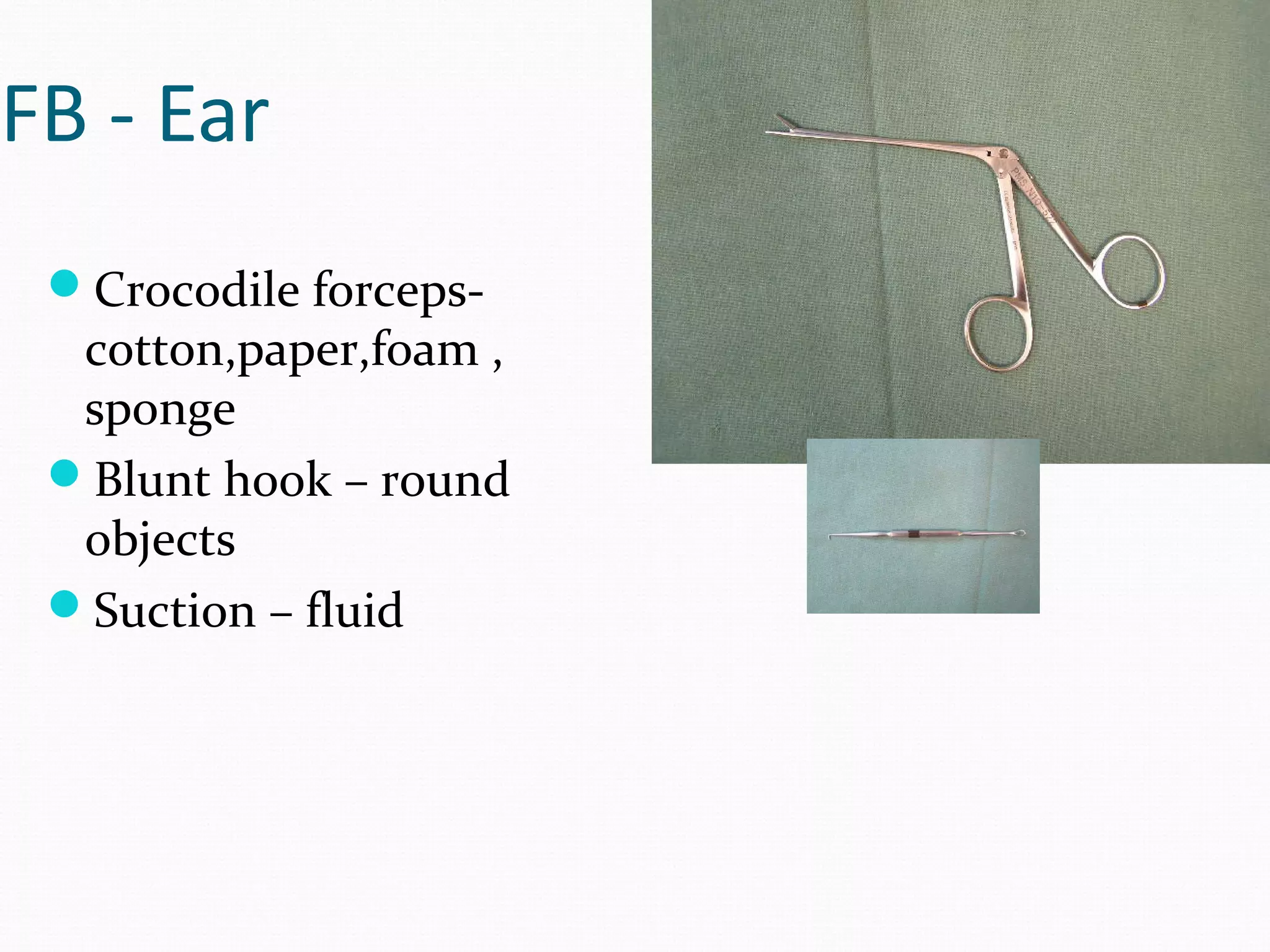
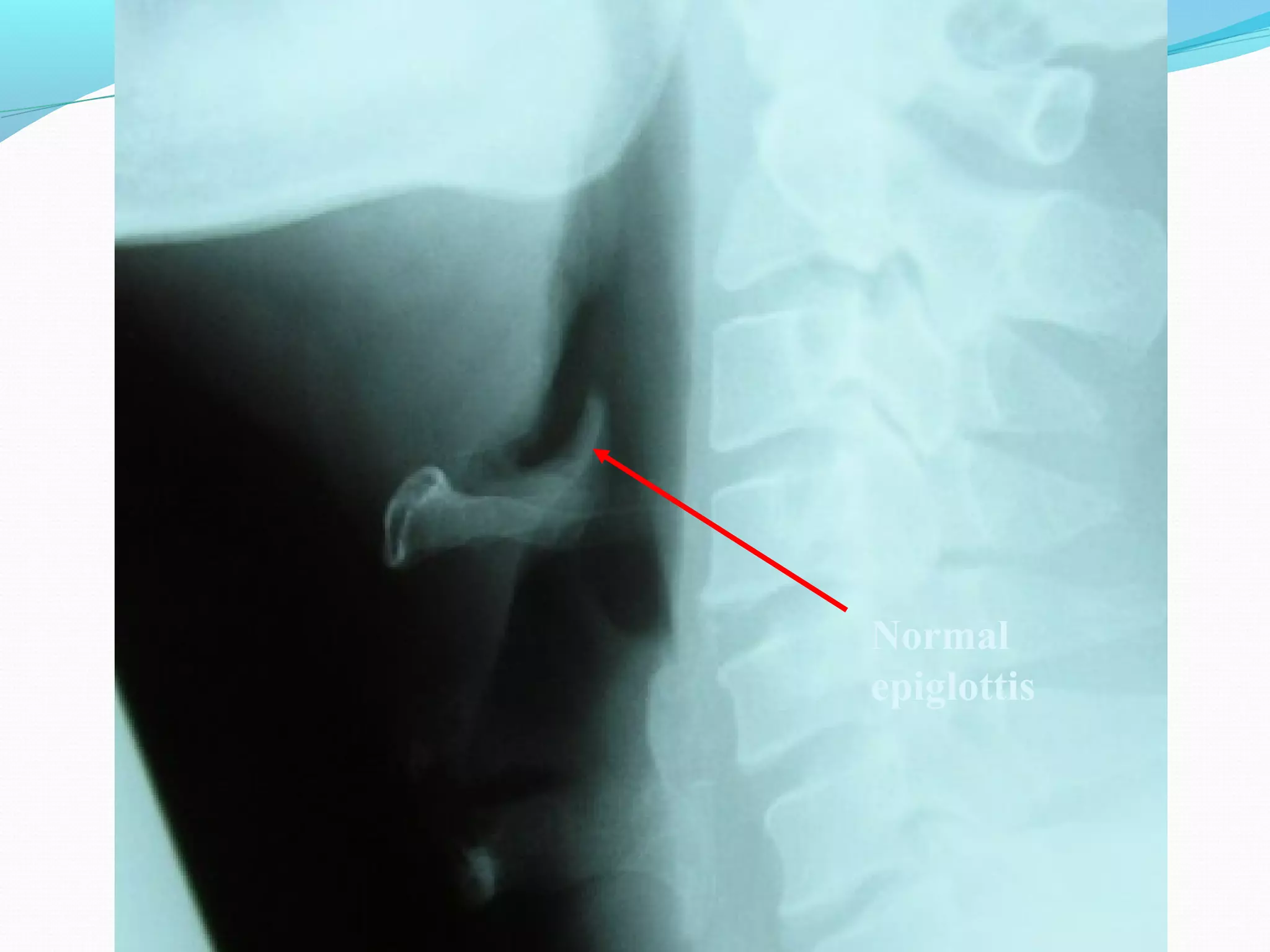
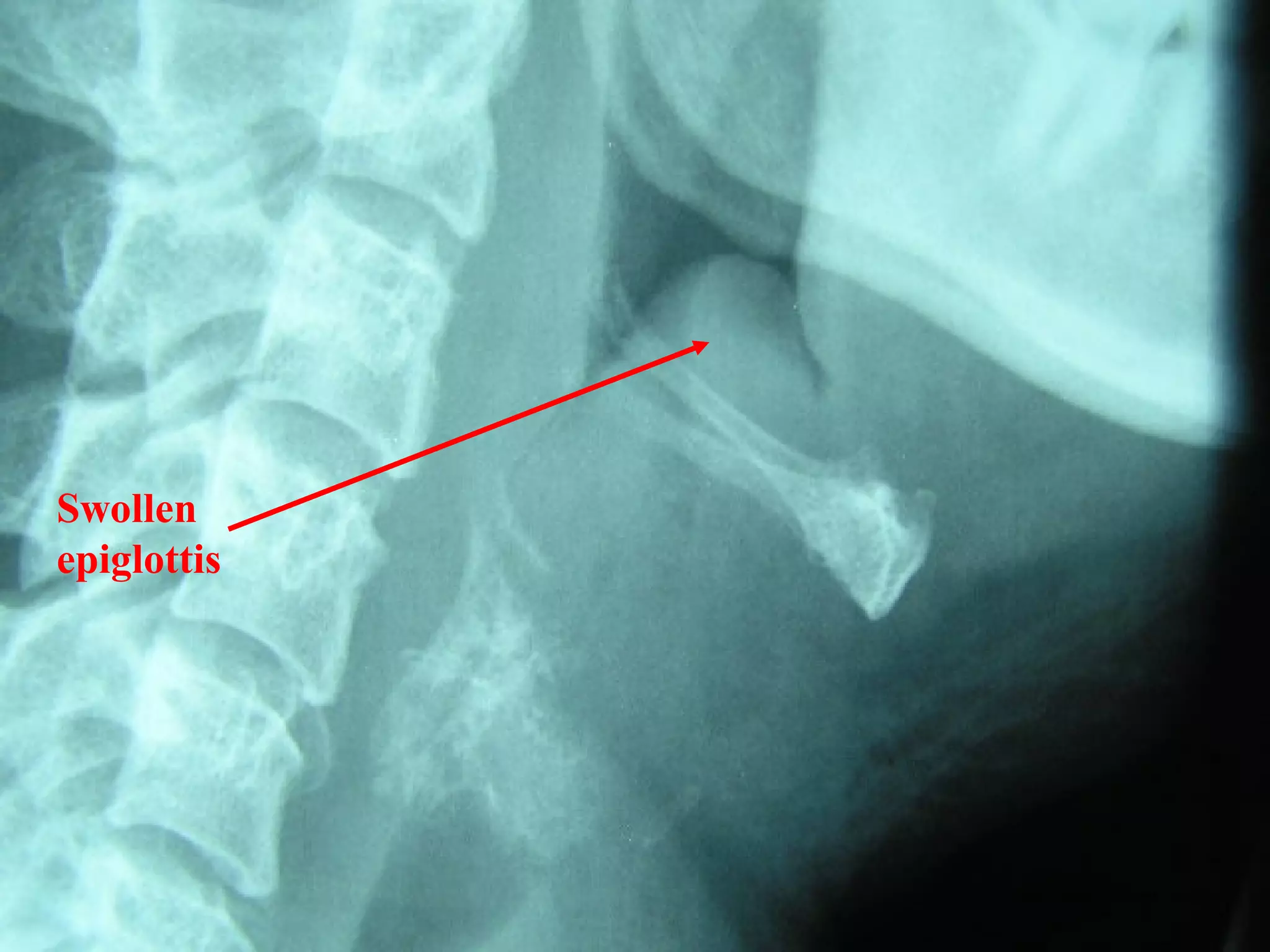
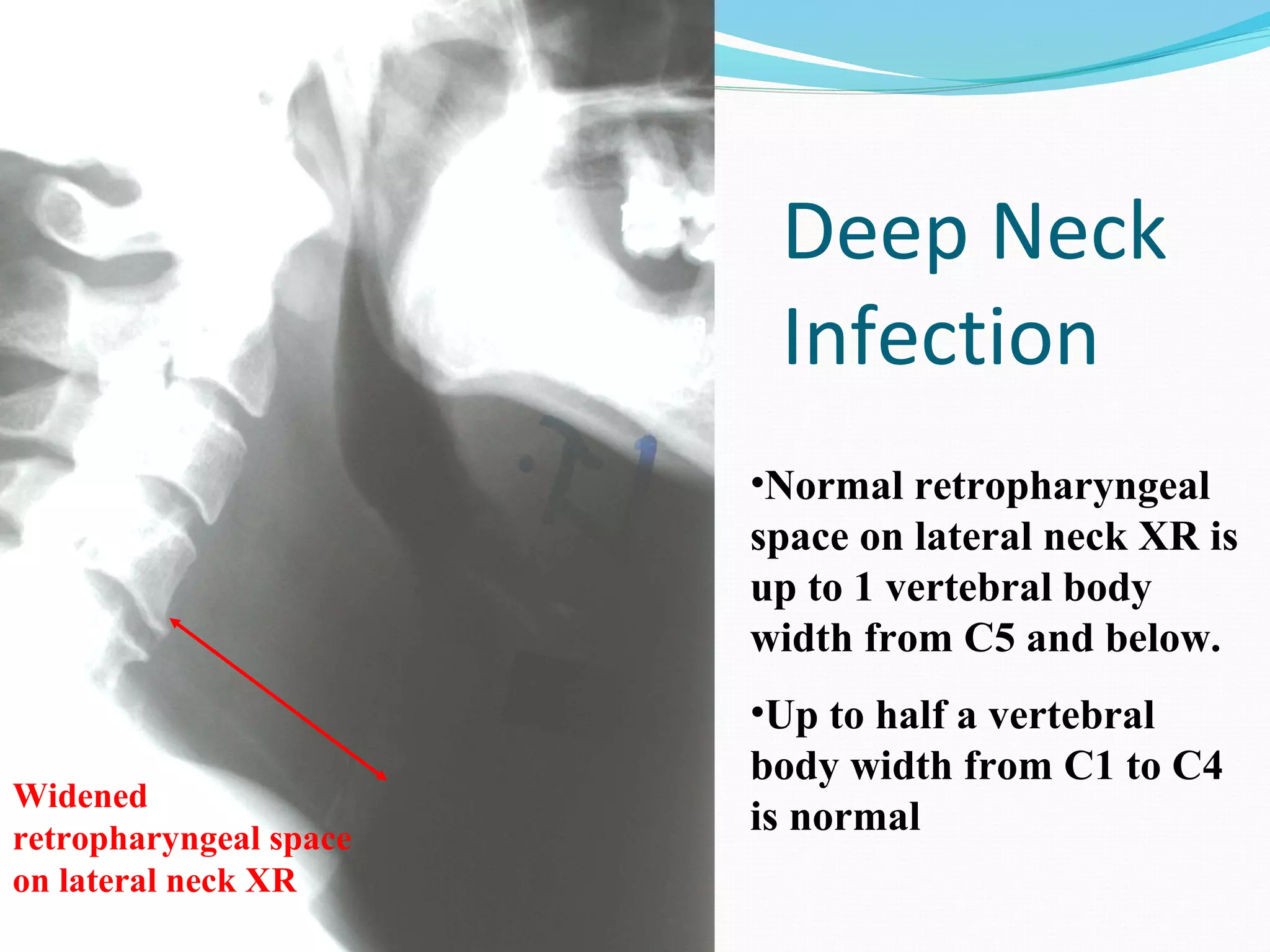
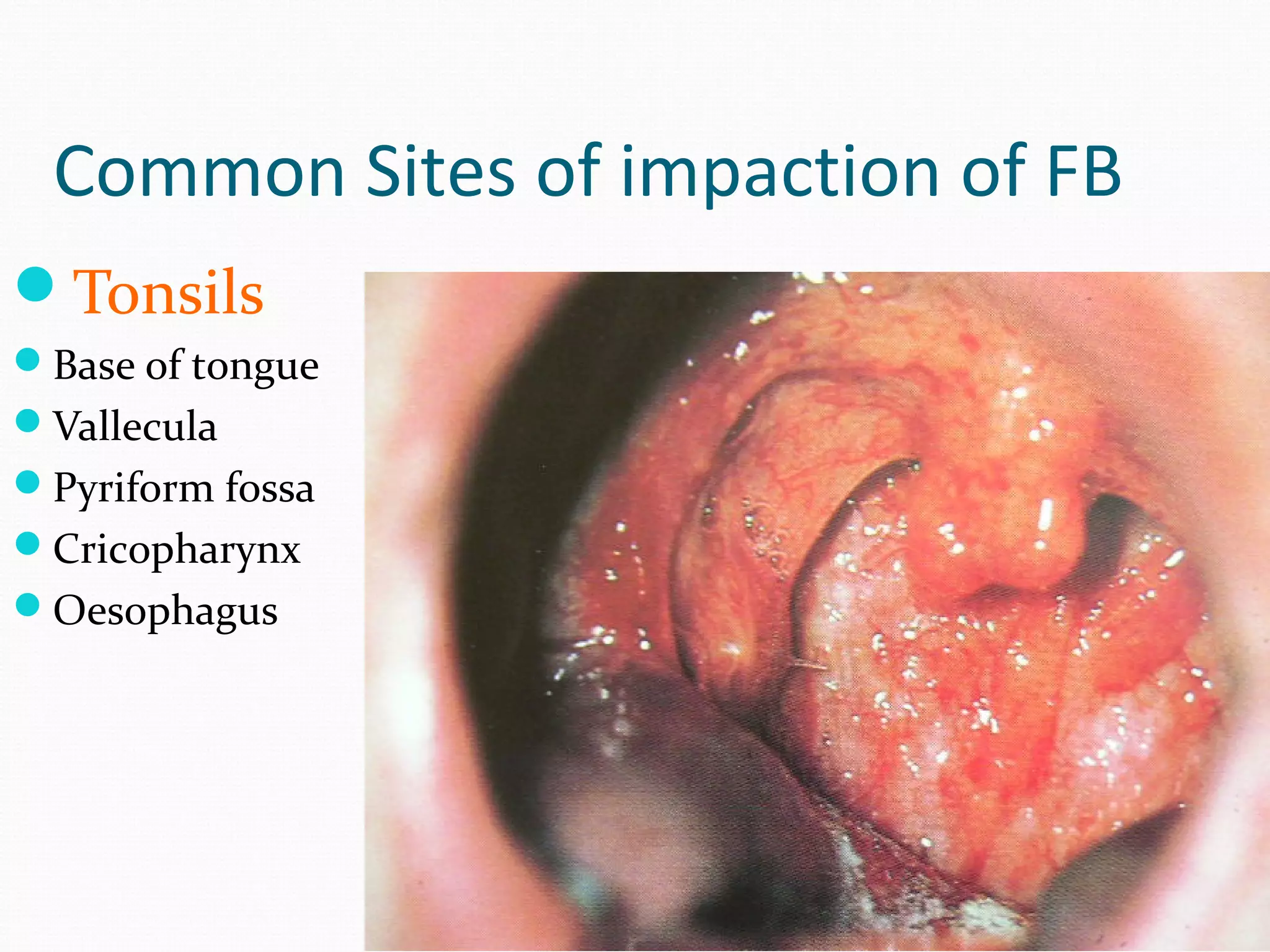
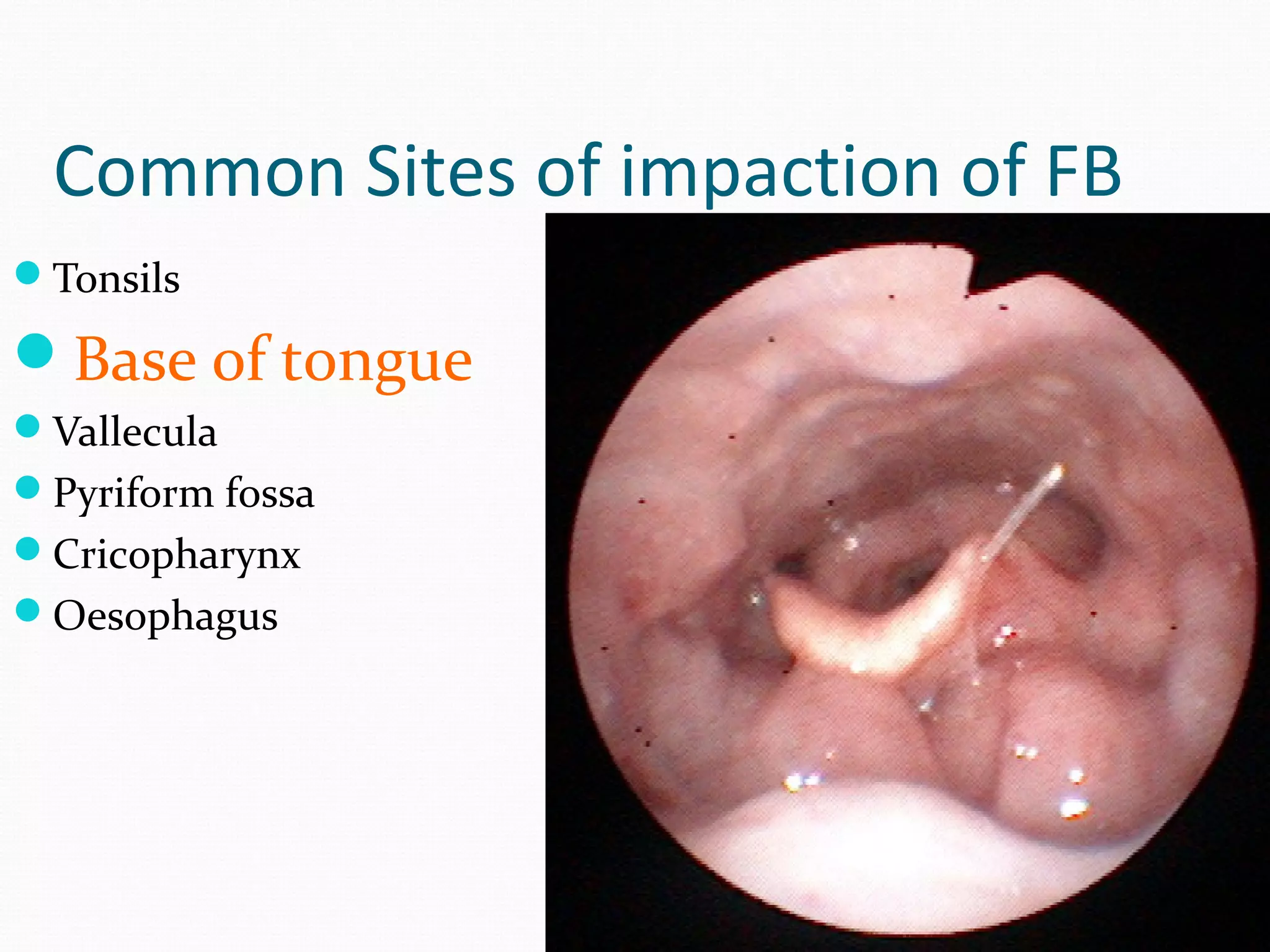
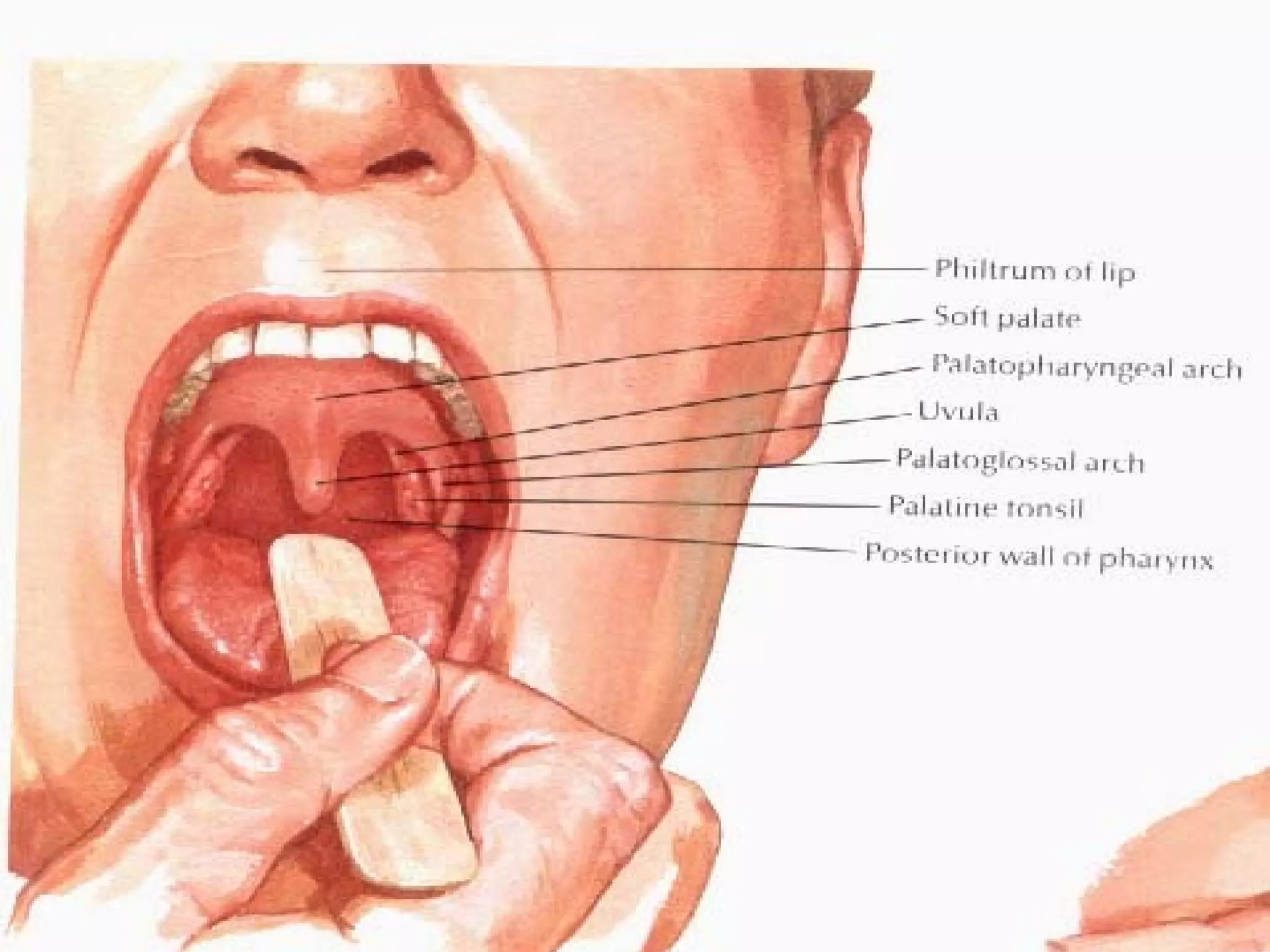
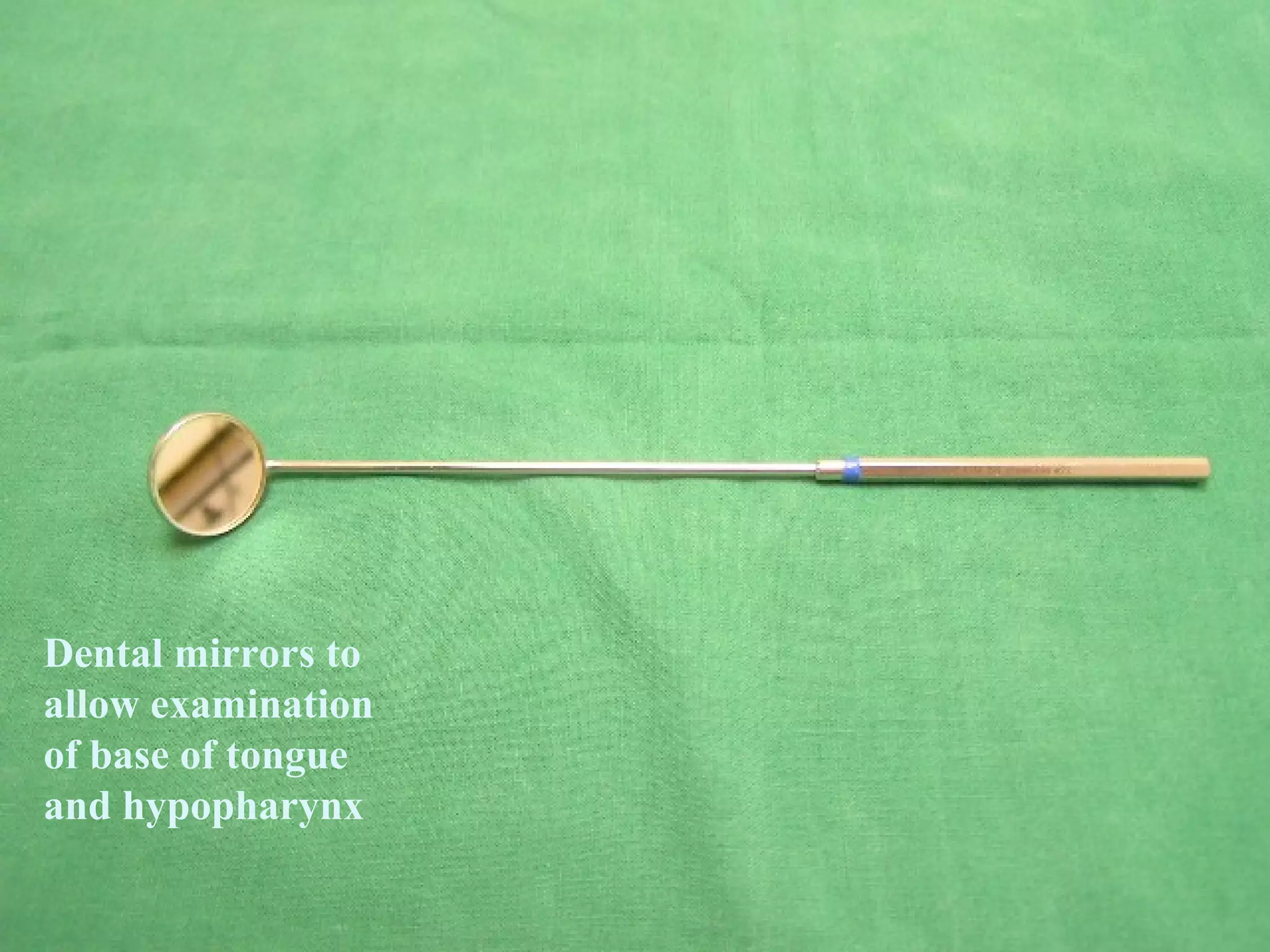
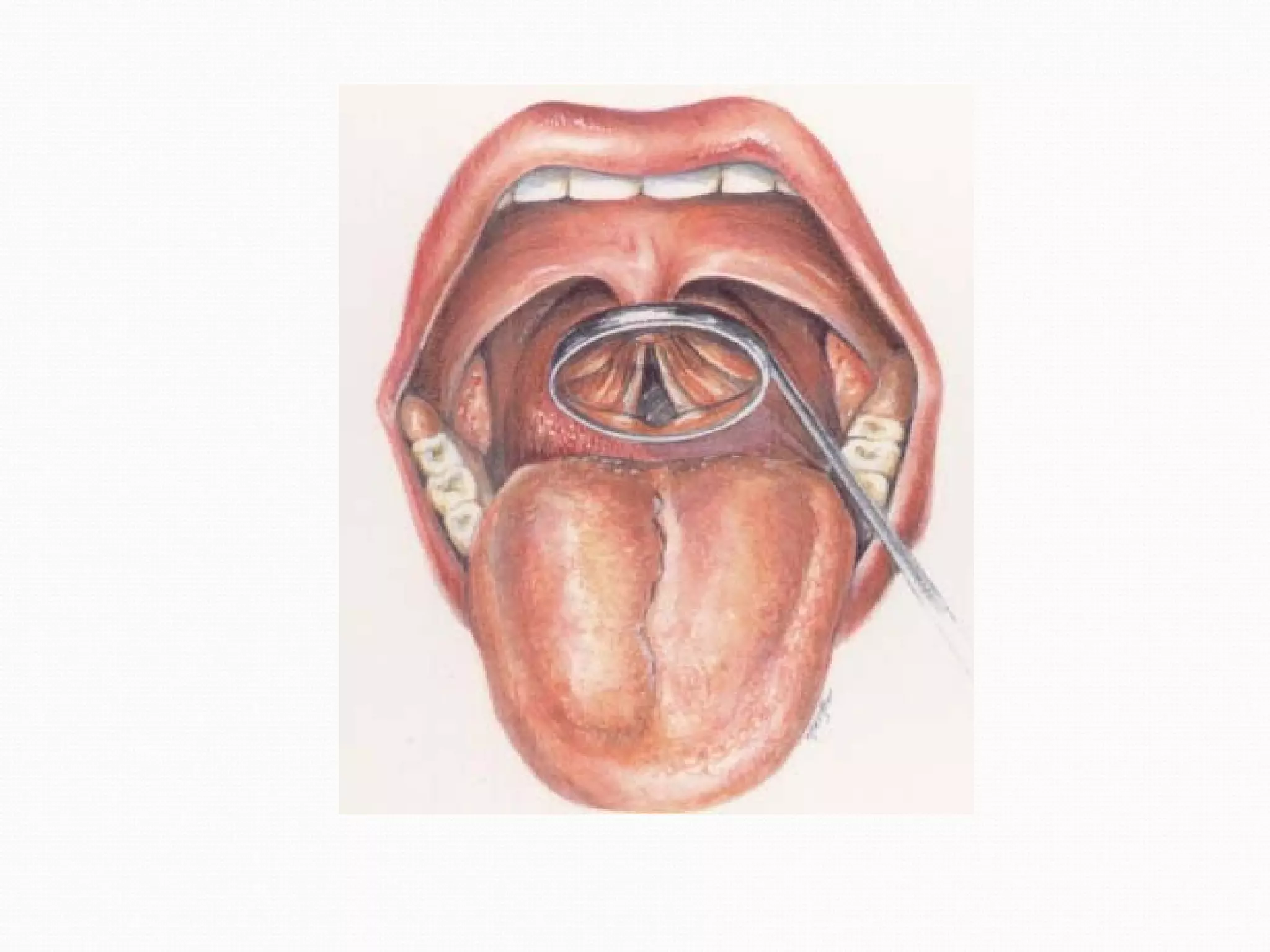
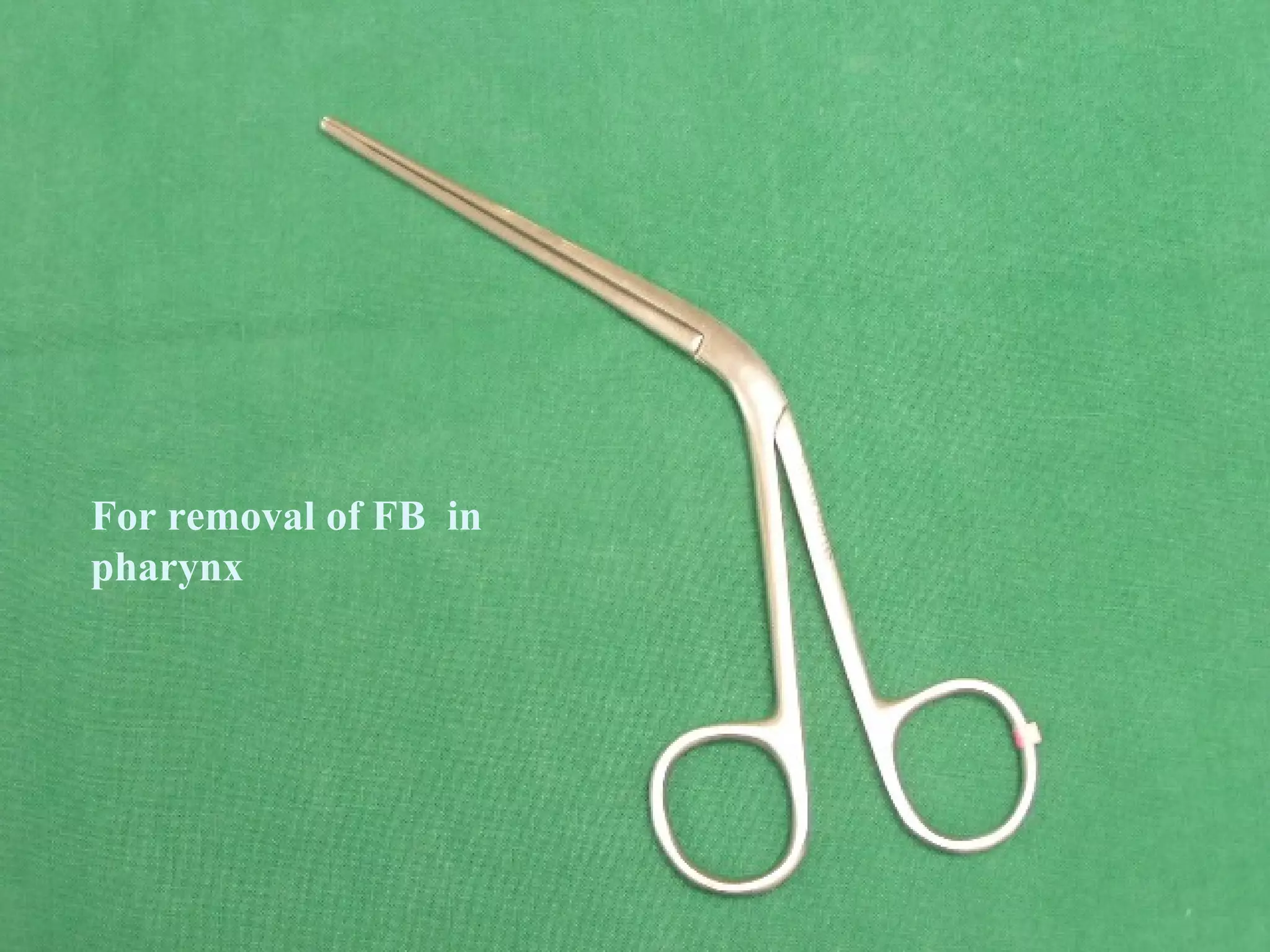
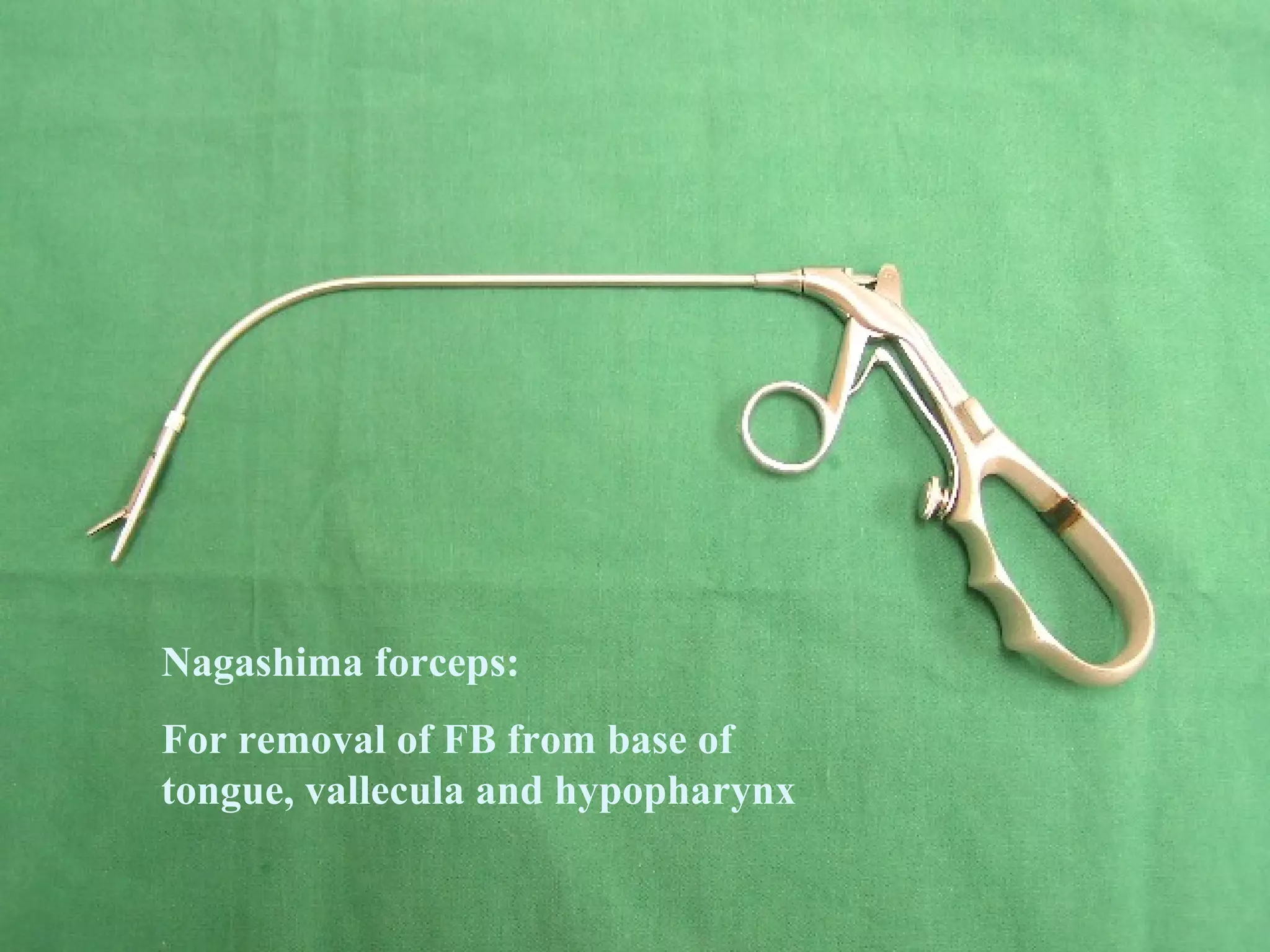
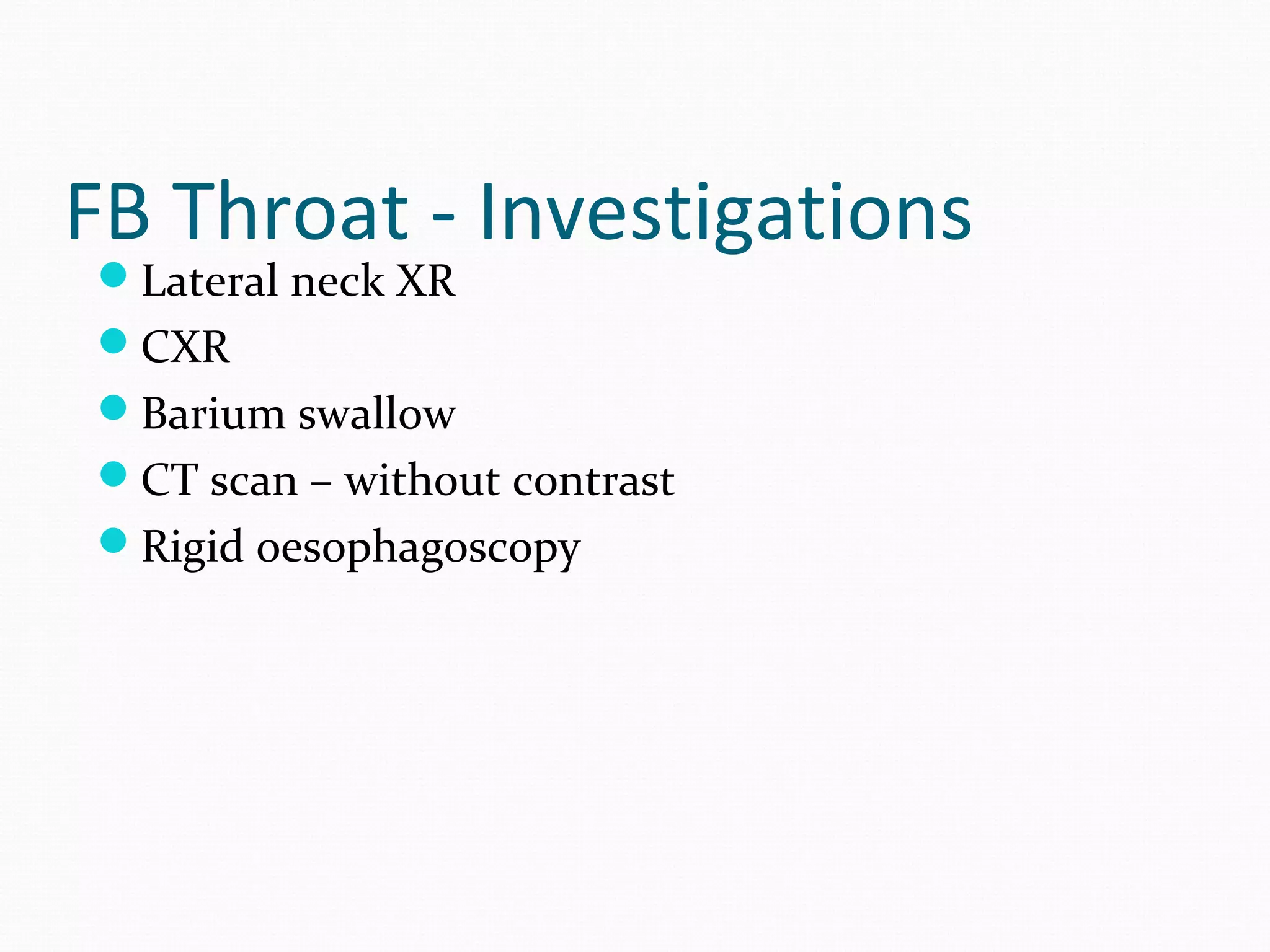
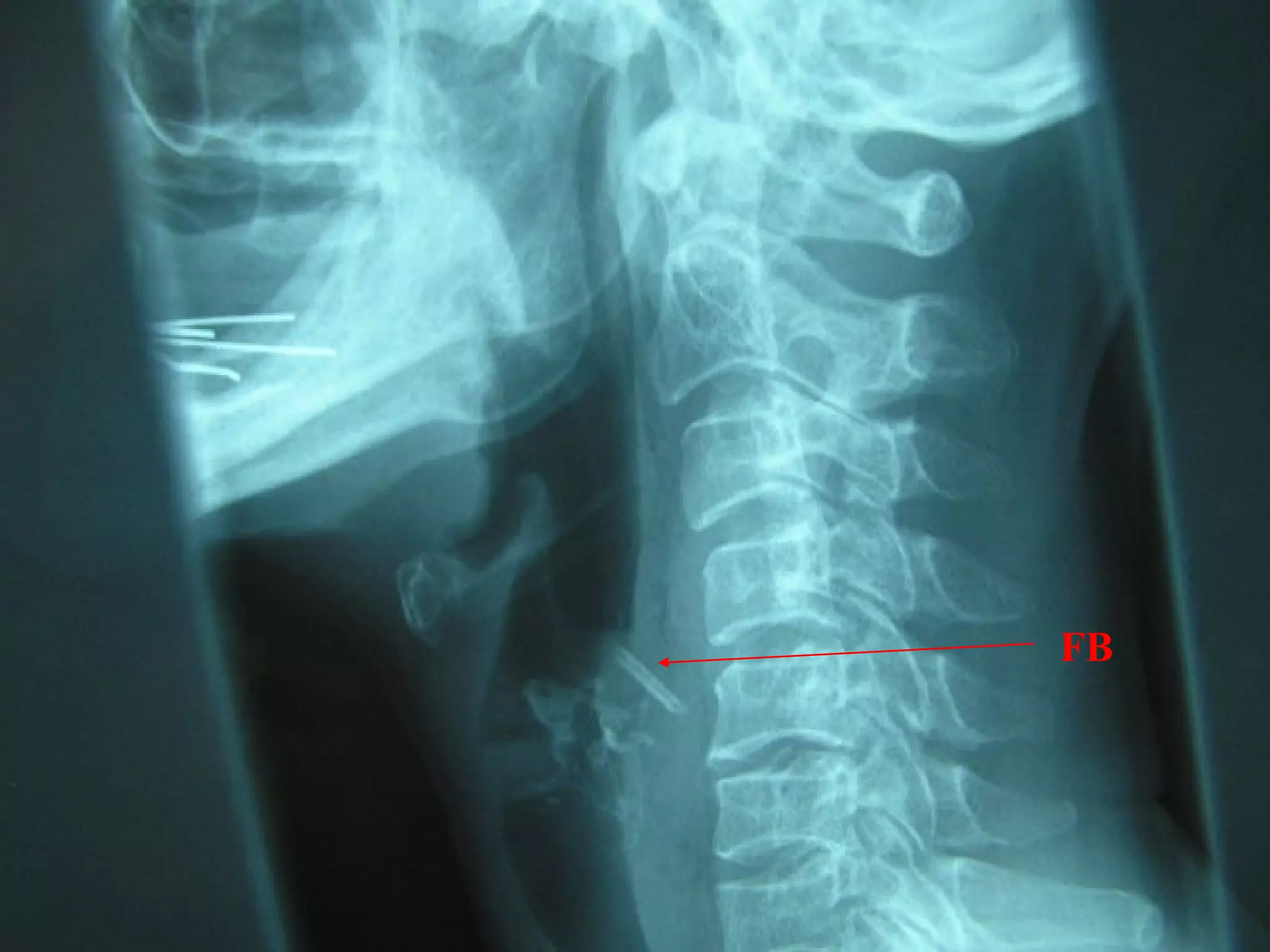
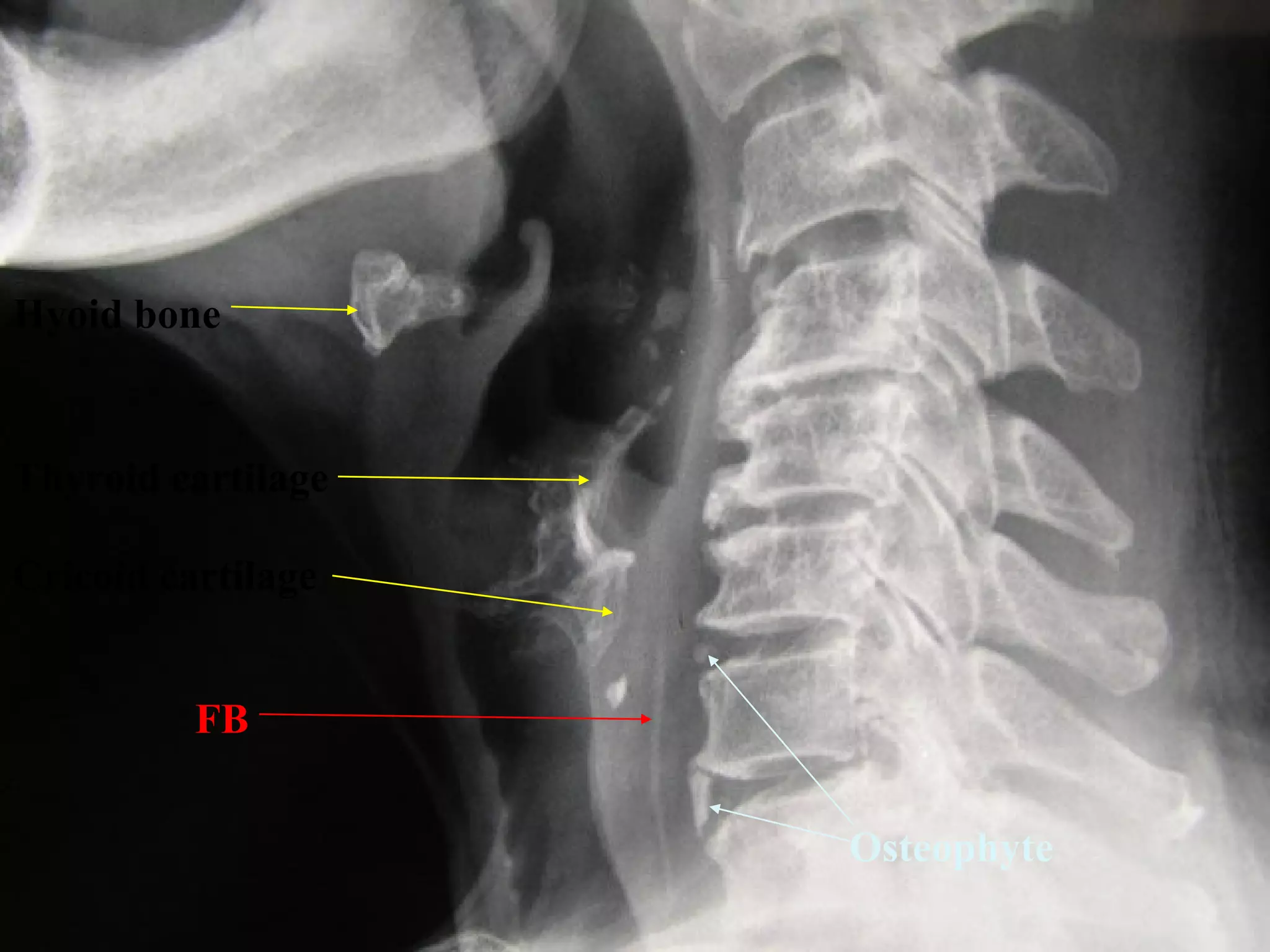
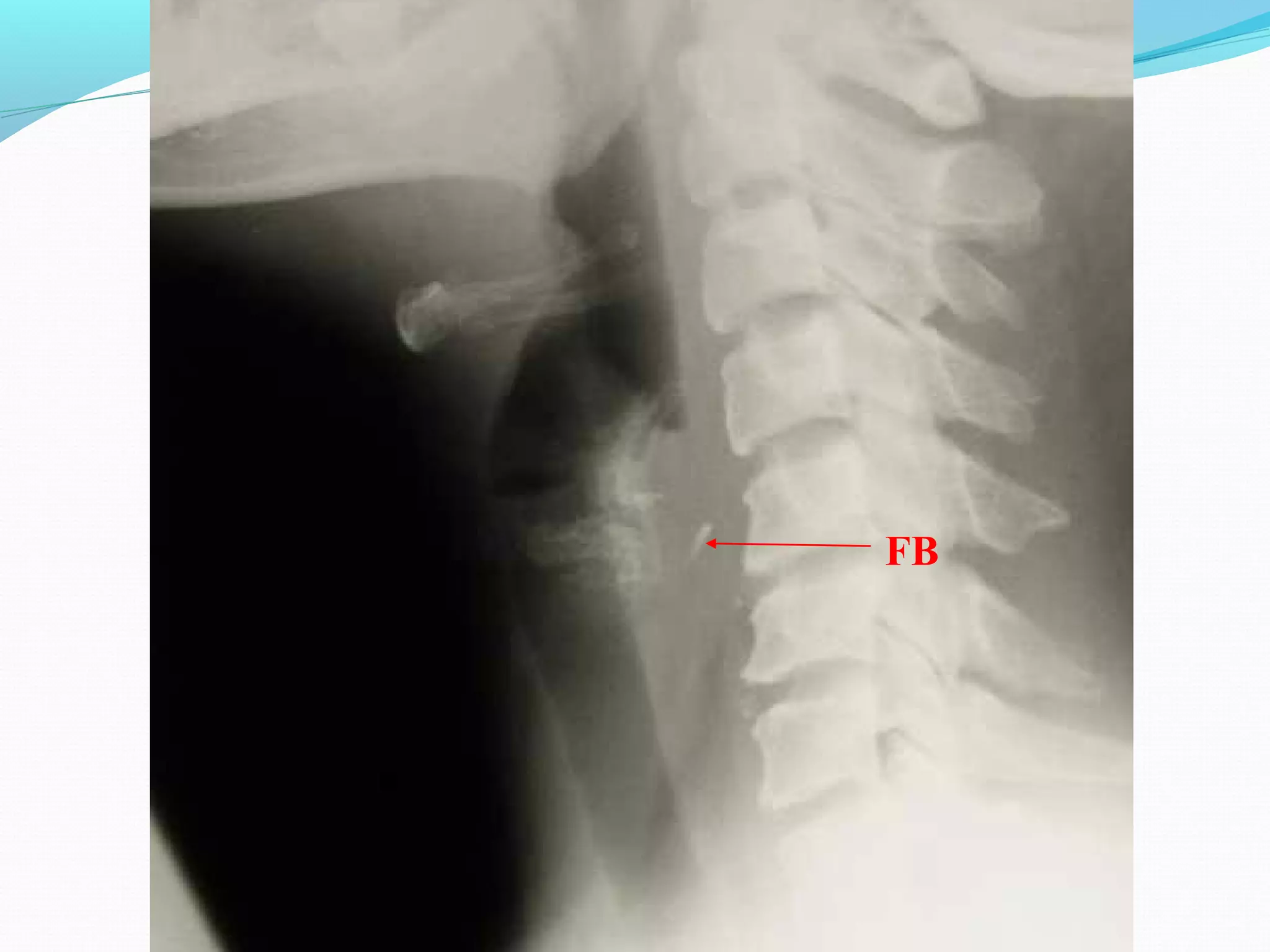
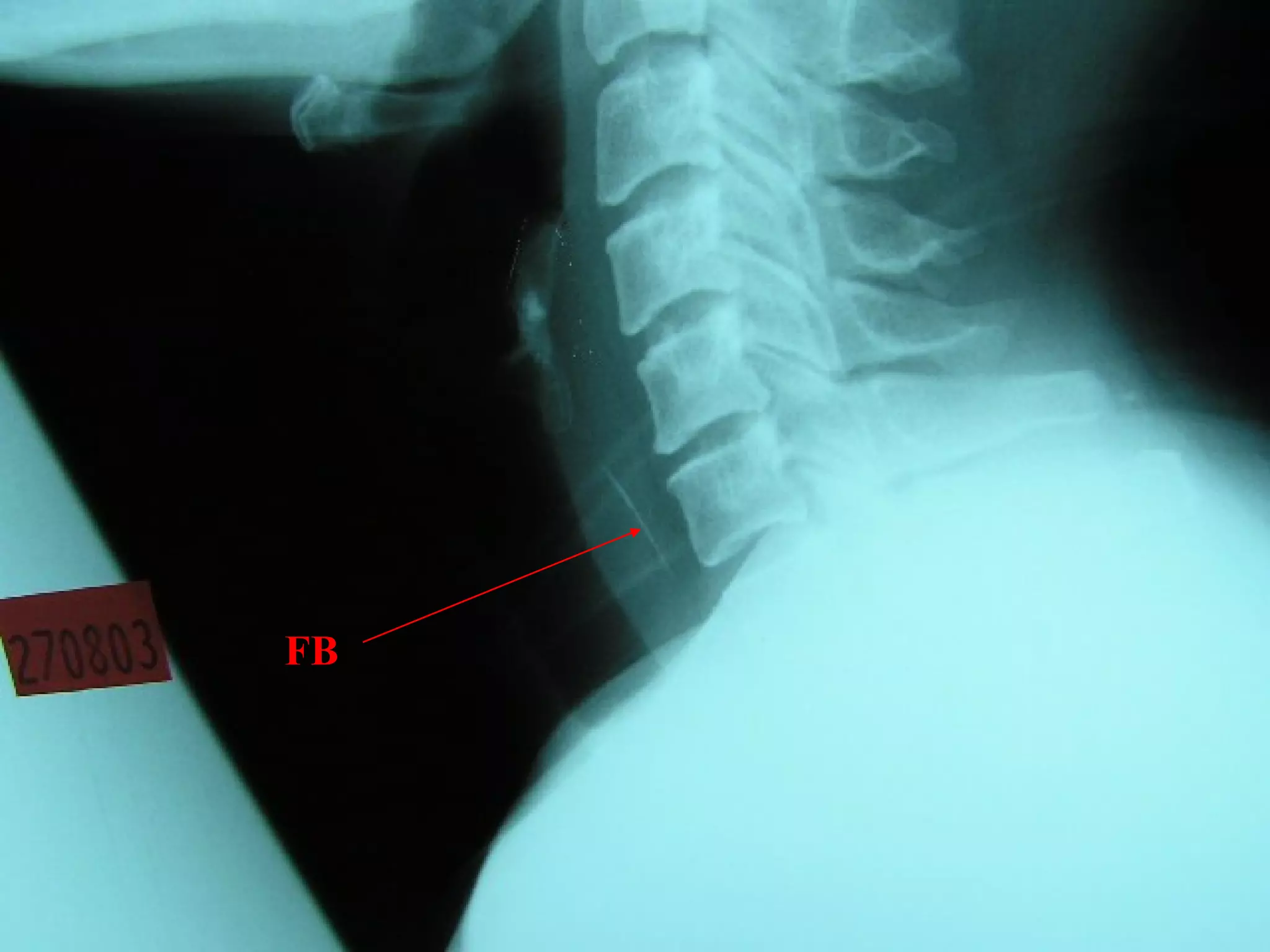
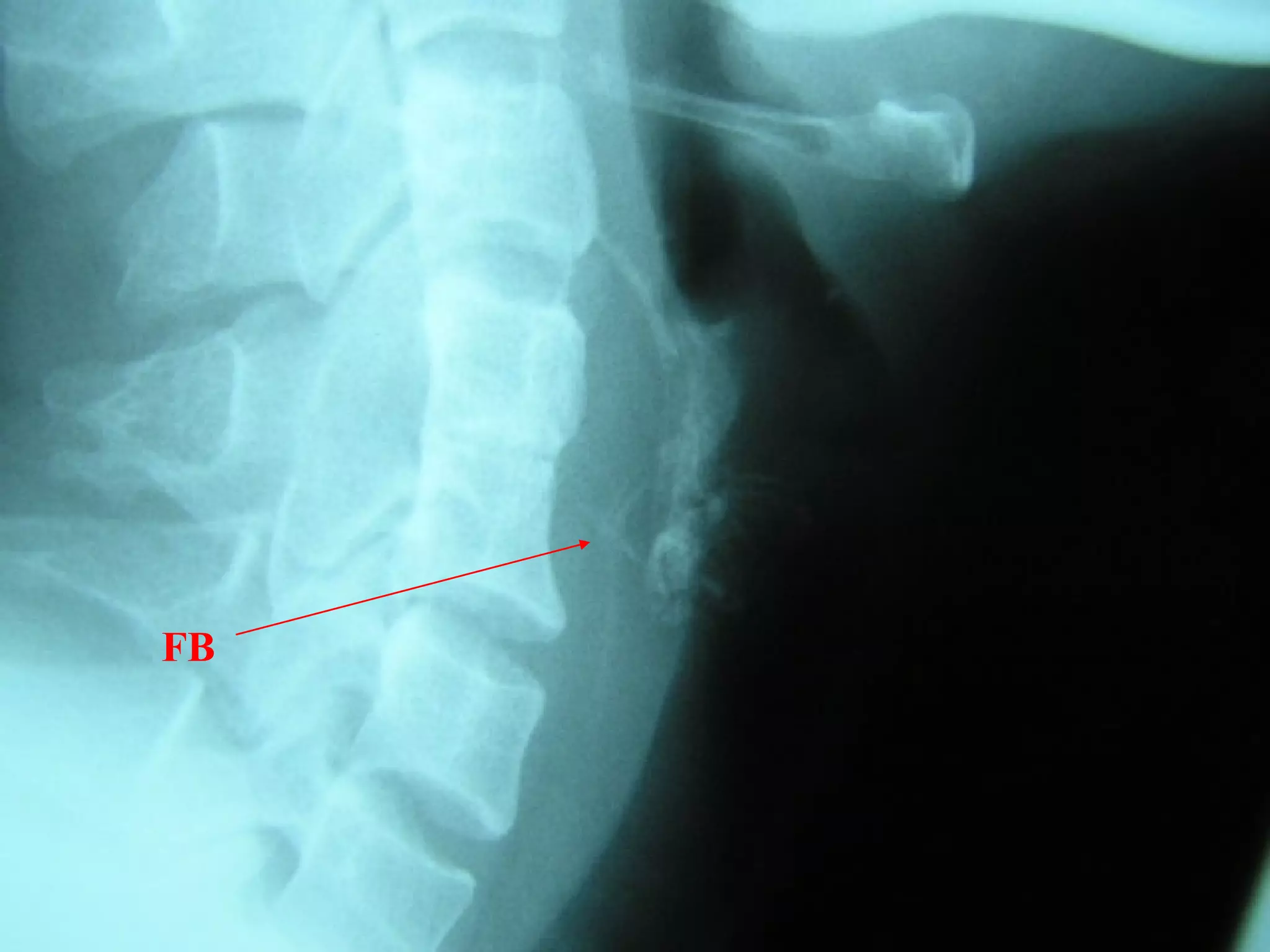
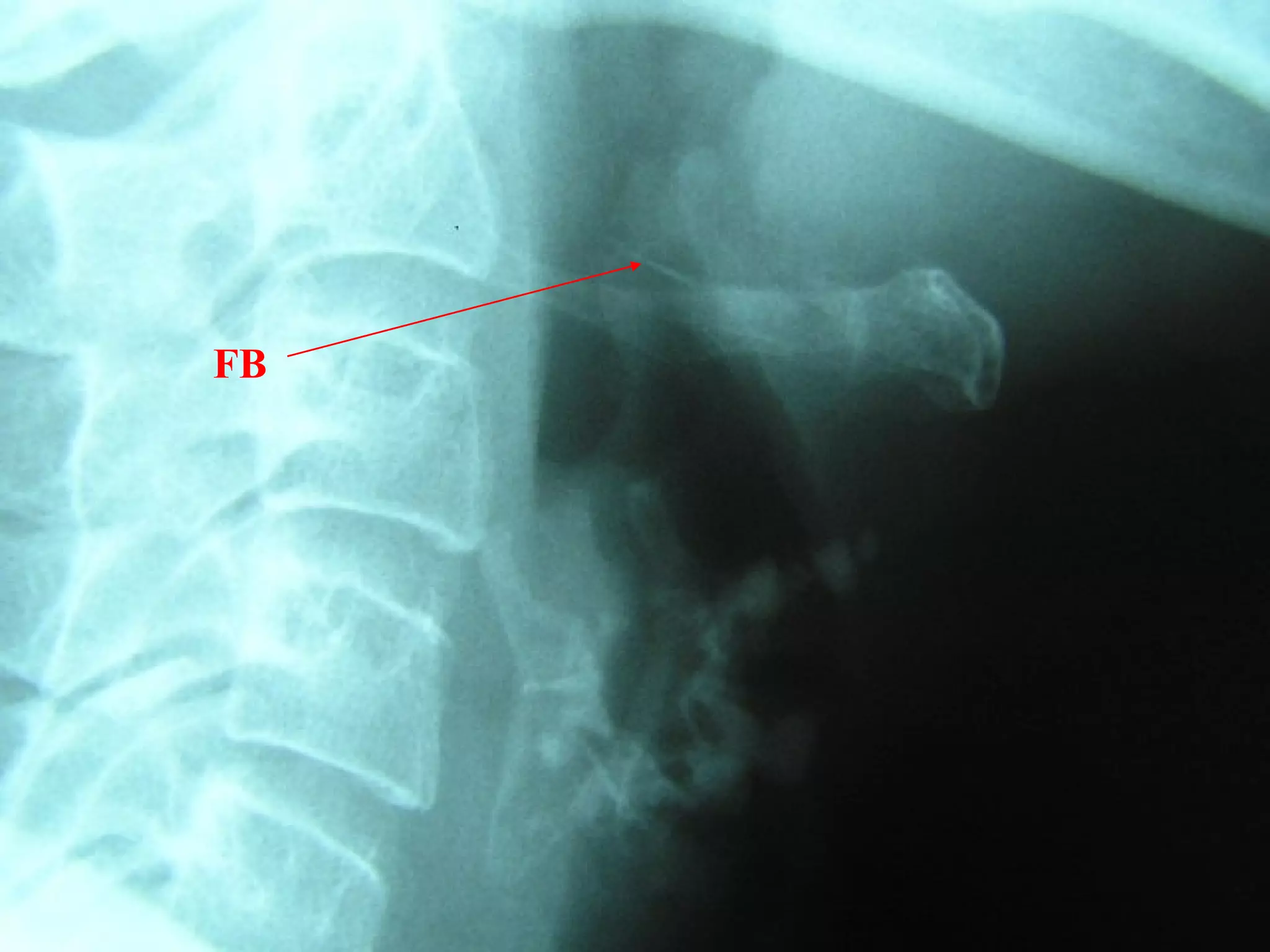
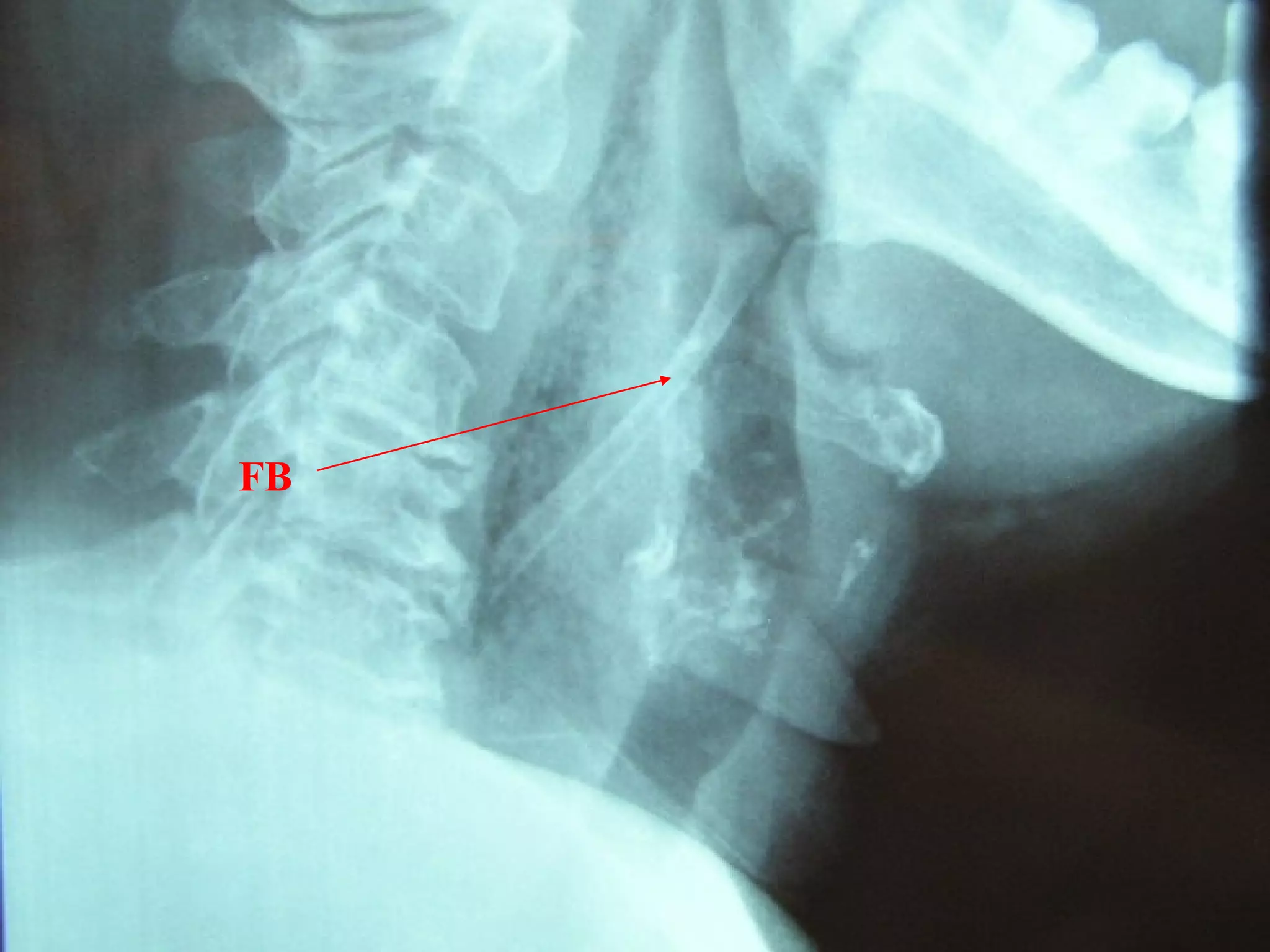
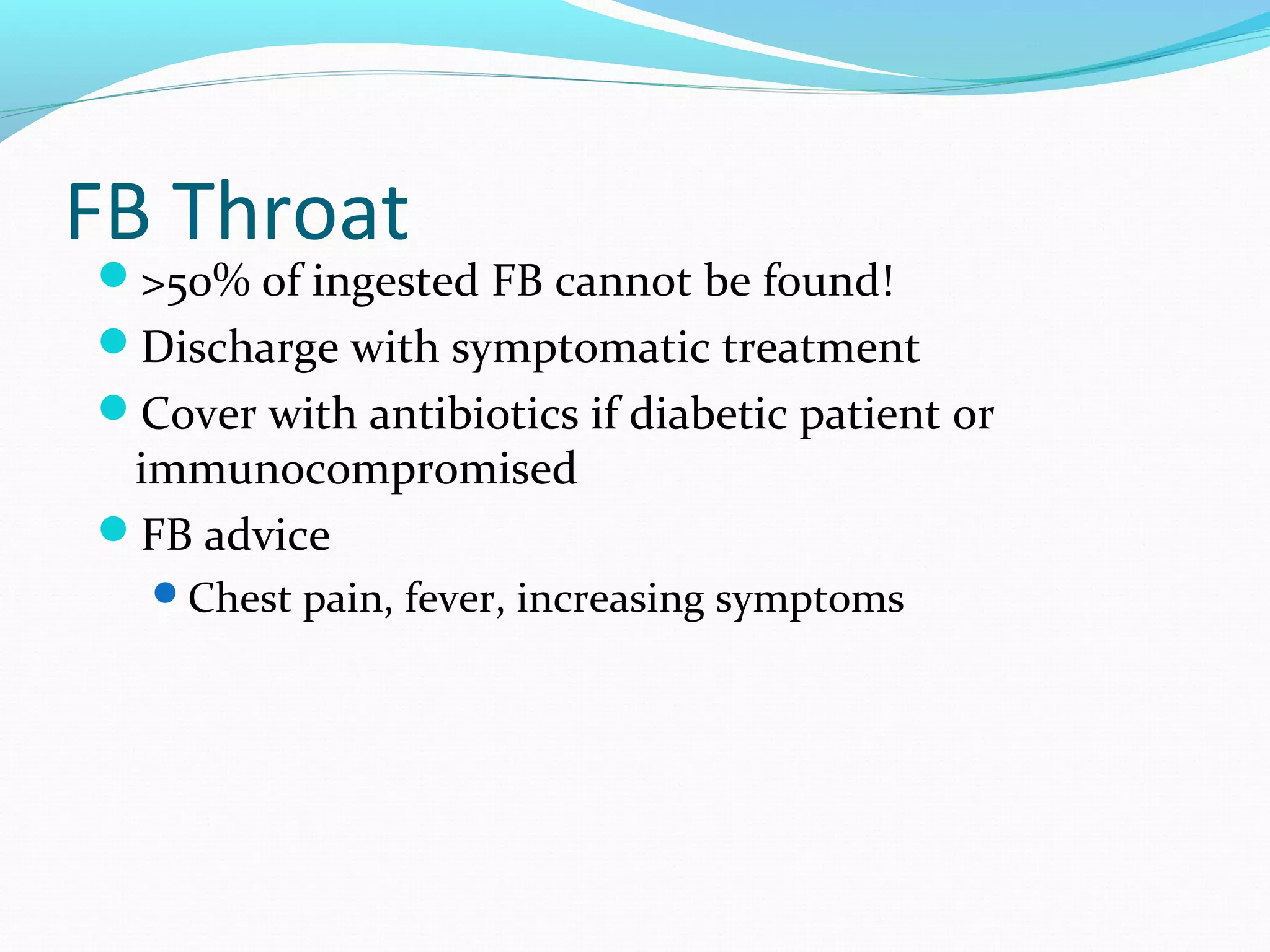
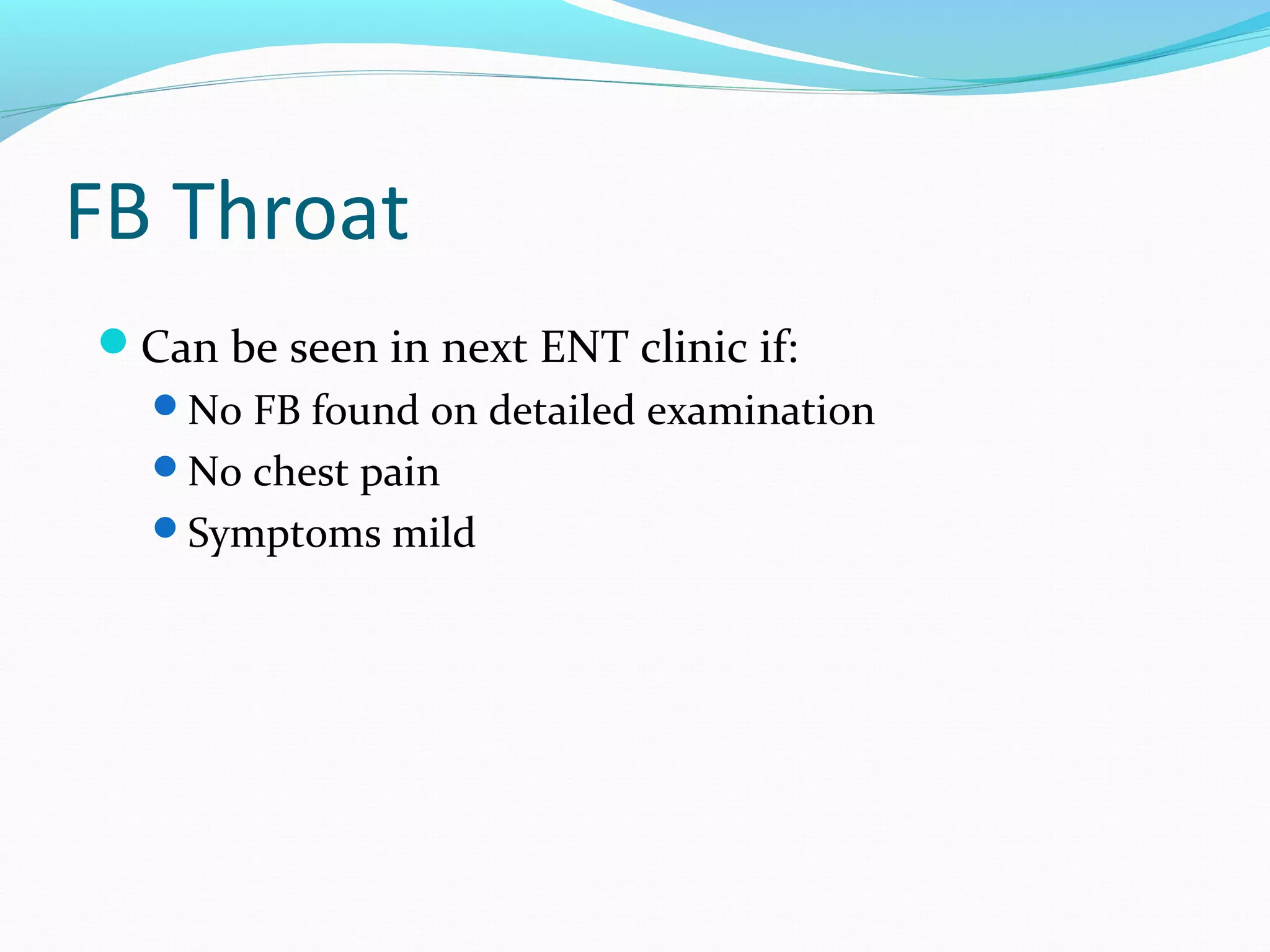
This document provides information on various ear, nose, throat and head and neck conditions commonly seen in emergency departments. It discusses the presentation, investigations, management and criteria for admission of nasal fractures, epistaxis, post-tonsillectomy bleeding, ear emergencies, head and neck infections, and ingested foreign bodies. Procedures for examining and removing foreign bodies from the throat are also outlined. The document serves as a guide for evaluating and treating ENT emergencies.