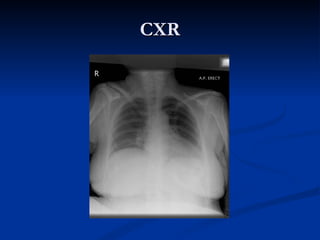
This document discusses a case of a 56-year-old female patient presenting with bilateral lower leg cellulitis and hyponatremia. She has a history of epilepsy, intellectual disability, and is on multiple medications including Moduretic. Initial workup found sodium of 118 mmol/L. She was started on IV saline and diuretics. Carbamazepine was identified as a potential cause of drug-induced hyponatremia and was replaced with levetiracetam. She was discharged on frequent sodium monitoring. The document then reviews hyponatremia causes, presentation, evaluation, and treatment considerations including the risk of rapid correction.