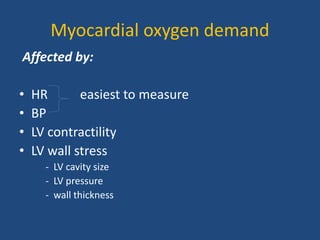
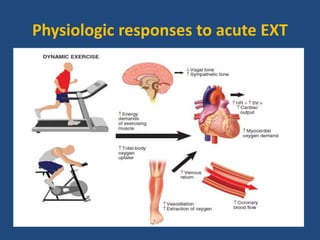
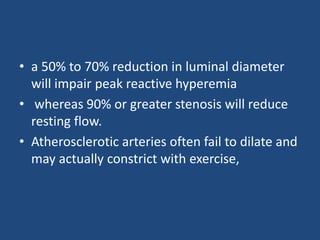
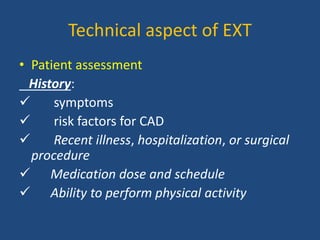
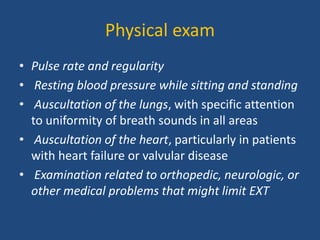
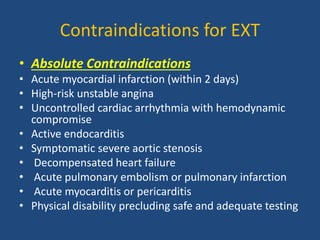
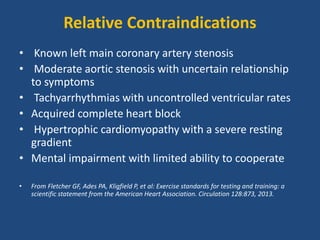
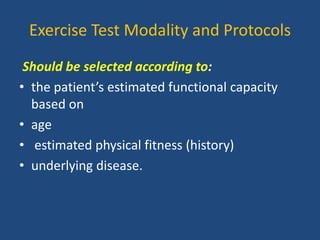
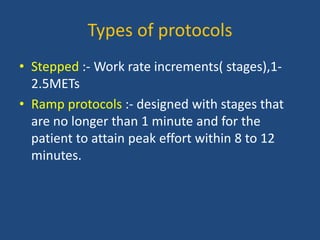
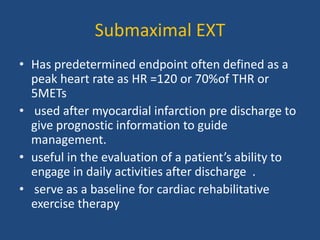
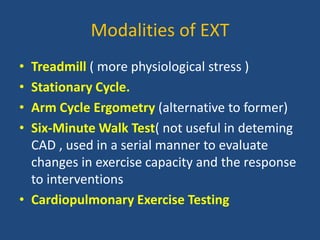
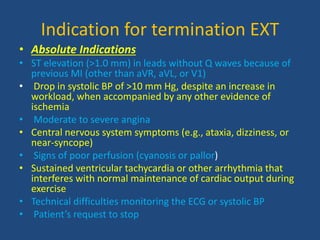
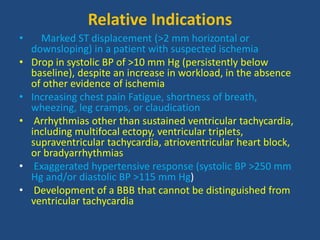
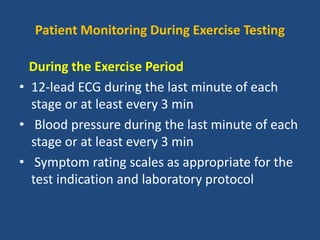
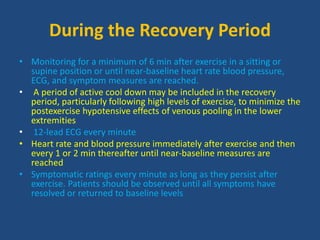
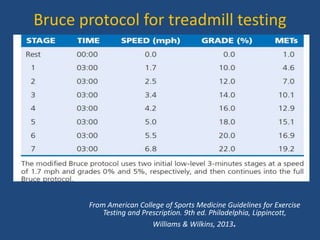
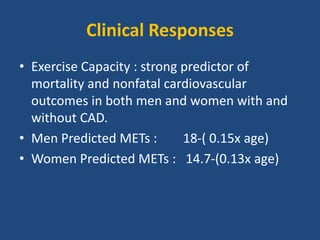
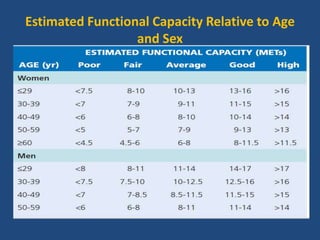
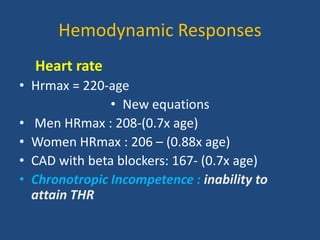
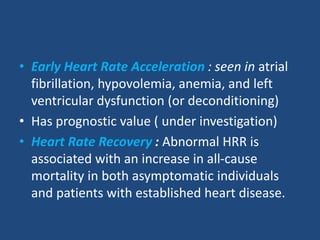
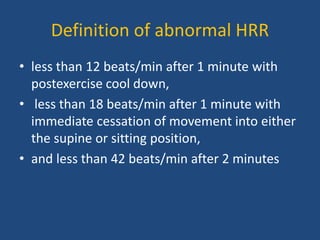
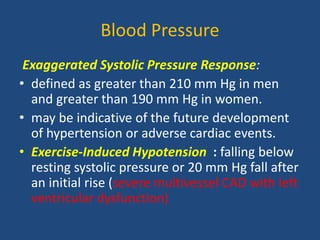
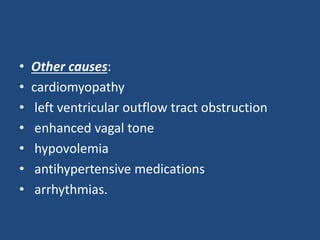
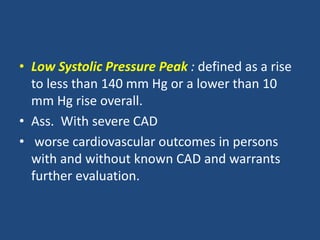
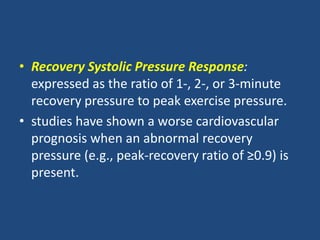
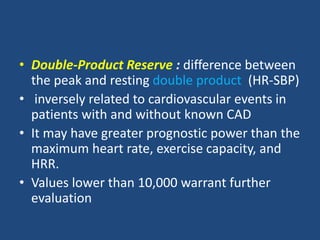
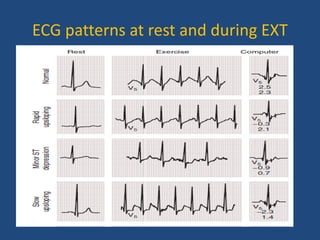
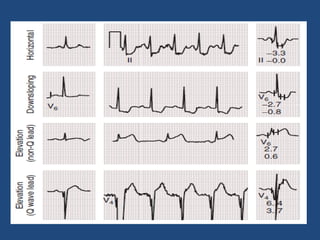
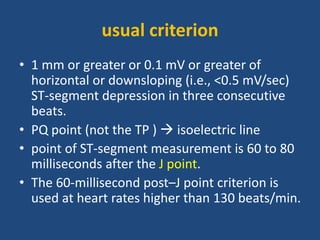
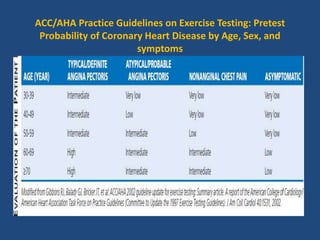
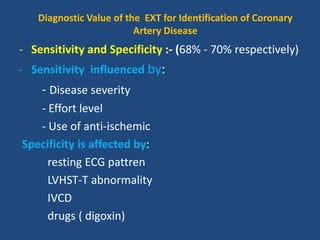
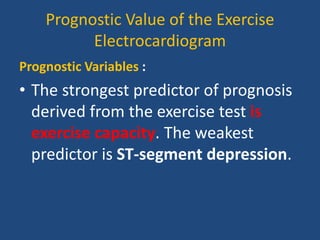
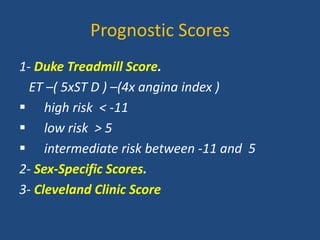
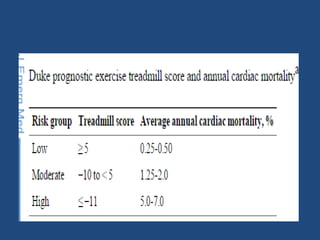
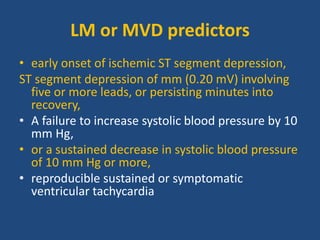
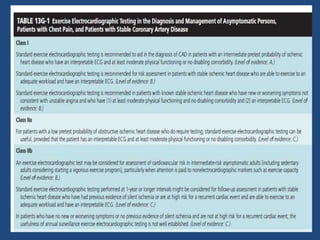
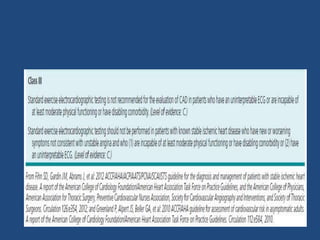
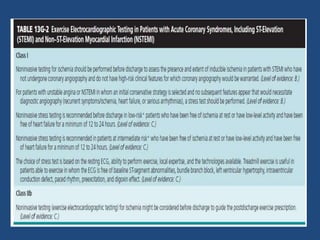
The document outlines an exercise tolerance test for diagnosing coronary artery disease (CAD) and assessing patient prognosis and functional capacity, covering physiological aspects, contraindications, and technical considerations of testing. It details the physiological responses to exercise, optimal protocols, monitoring during tests, and the interpretation of various metrics, including heart rate and blood pressure changes. Furthermore, it discusses diagnostic and prognostic values of the exercise electrocardiogram and provides guidelines for interpreting test results.