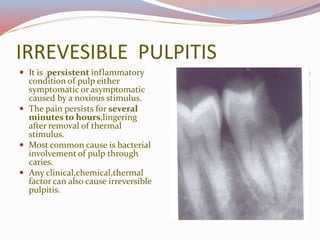
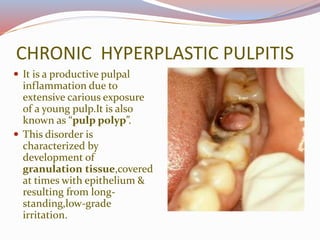
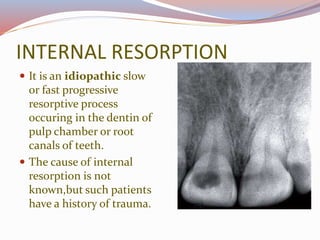
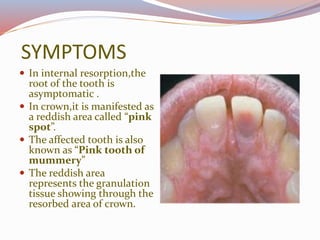
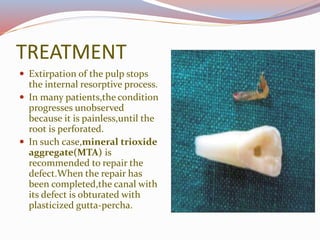
The document provides a detailed overview of pulpitis, its definitions, types (reversible and irreversible), symptoms, and treatment options. Reversible pulpitis is characterized by mild inflammation and pain that can be alleviated by removing irritants, whereas irreversible pulpitis involves persistent inflammation and severe pain often caused by bacterial infection. Additional conditions discussed include chronic hyperplastic pulpitis and internal resorption, each with unique histopathological features and treatment approaches.