Vaginal instillation
- 1. Prepared by- Aashish Parihar m.sc. nursing
- 2. Introduction Advantages Disadvantages Forms of medication General instructions Articles required Procedure
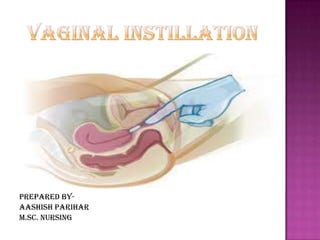
- 3. Introduction Vagina is route for administration for contraceptives, antifungal and anti microbial. It is used for the achievement of local and systemic absorption. Vaginal medications include suppositories, creams, gels, and ointments. Suppositories melt when they contact the vaginal mucosa, and their medication diffuses topically (as effectively as creams, gels, and ointments). Vaginal medications usually come with a disposable applicator that enables placement of medication in the anterior and posterior fornices.
- 4. Advantages Prolonged release. Minimal systemic side effects. An increase in bioavailability. Use of less total drug than an oral dose. First-pass metabolism can be avoided. Self medication is possible.
- 5. Disadvantages Patient incompliance. Only a few drugs are administered by this route. Variability in drug absorption related with menstrual cycle, menopause and pregnancy, can also limit vaginal drug delivery route usage. Influence with sexual intercourse. Gender specificity.
- 6. Forms of vaginal medication Many different types of formulations have been applied vaginally as- Tablets Vaginal suppositories or pessaries (globular, oviform or cone-shaped, and weighing about 5 g each. ) Douches (aqueous solutions that are administered into the vagina for cleansing purpose. ) Foams Sprays Gels Creams Vaginal rings (Creams, gels, sprays and foams are used as vehicles for drugs such as anti-infective or contraceptive agents.)
- 7. General instructions To prevent damage, suppositories must be stored in refrigerator. Foams, jellies, and cream are administered with an inserter or applicator. Perineal pads may be used to collect excess drainage after inserting a suppository. Good aseptic technique must be followed. Good perineal hygiene must be maintained. The patient should be encouraged to empty her bladder as she has to lie down for 20 minutes The patient can either lie supine with knees up or lateral with knees up Always lubricate the pessary or applicator before inserting
- 8. Articles required A clean tray containing- Medication administration record (MAR) Nonsterile gloves Mackintosh Prescribed vaginal suppository or any other form of vaginal medication Perineal pads Water-soluble lubricant Disposable applicator Tissue paper/ cotton balls Paper bag Kidney tray And Side screen
- 9. Procedure Preliminary assessment- Review the physician’s order, patient’s name, name and form of vaginal medication, dosage and time. Explain procedure to patient. If client plans to self-administer, be very specific with instructions. Gather necessary equipment. Follow the rights of medication administration. Ask the client to void. Provide for privacy. Wash hands Don Nonsterile gloves. Position the client in a dorsal recumbent position with knees flexed and hips rotated laterally or in a Sims’ position. Assess perineal area, inspect vaginal orifice, note any odor or discharge from the vagina, and inquire about any problems such as itching or discomfort.
- 10. Procedure If secretion or discharge is present, cleanse the perineal area with soap and water. Remove suppository from the foil wrapper and, if applicable, insert into applicator tip. Apply a small amount of lubricant to rounded tip of suppository. If not using an applicator, apply a small amount of lubricant to gloved index finger. With non dominant hand, spread labial folds. Insert the suppository into the vaginal canal at least 2 inches (5 cm) along the posterior wall of the vagina or as far as it will go If using an applicator, insert as described above and depress plunger to release suppository.
- 11. Procedure After care- Wipe the perineum with clean, dry tissue. Instruct the client to remain in bed for 15 minutes. Wash applicator under cool running water to clean and return to appropriate storage in the client’s room. Remove gloves, turning them inside out, dispose them. Wash hands. Record on the MAR the drug’s name dosage, route, and date and time of administration; document any evidence of discharge or odor from the vagina. Check with the client in 15 minutes to ensure that the suppository did not slip out and to allow the client to verbalize any problems or concerns. Observe for effectiveness of the medication; inspect the condition of the vaginal canal and external genitalia between applications.
