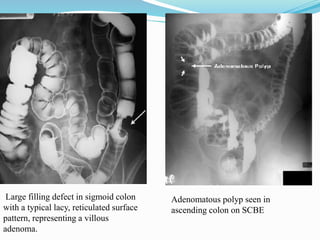
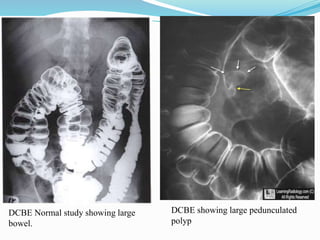
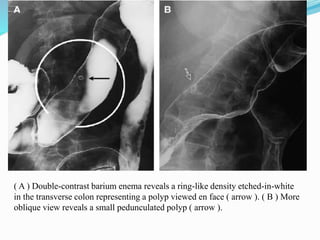
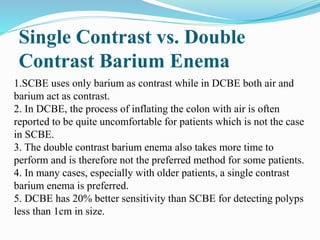
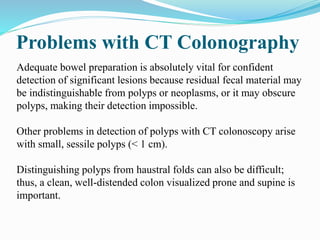
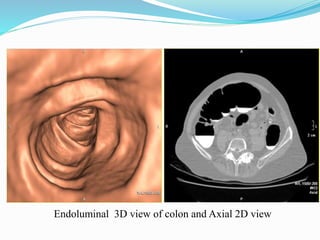
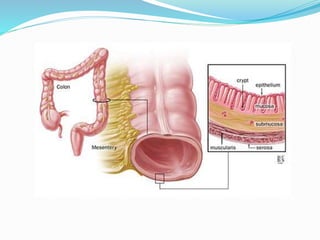
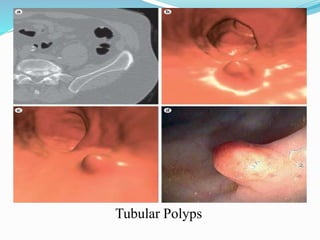
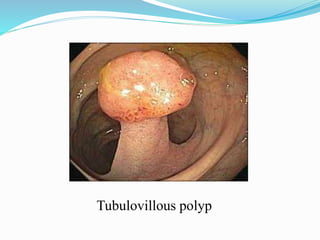
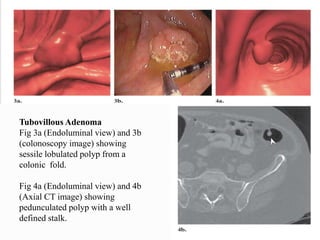
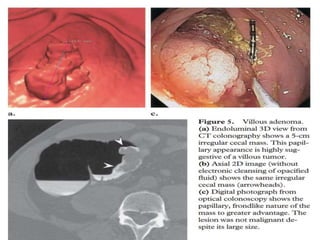
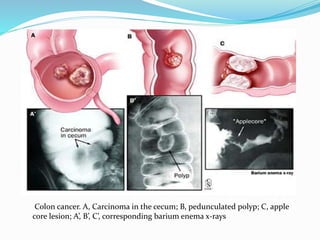
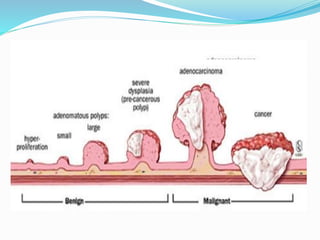
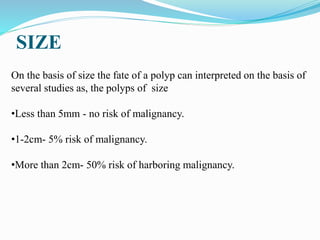
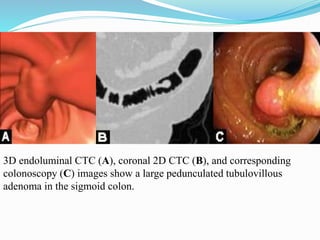
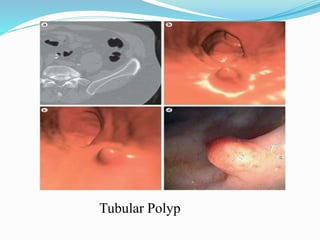
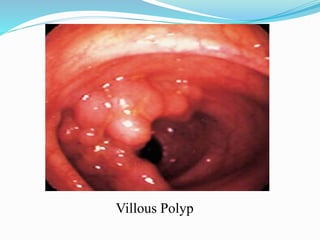
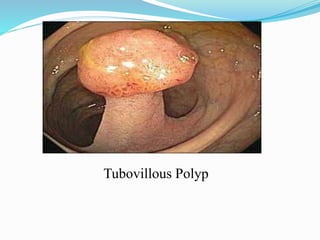
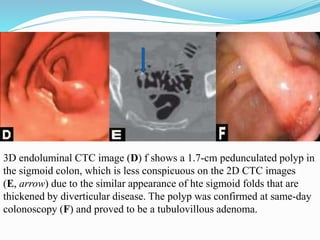
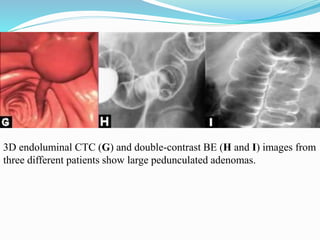
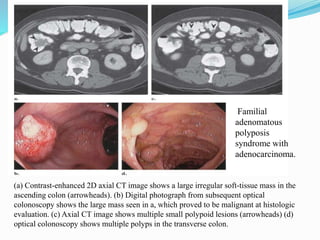
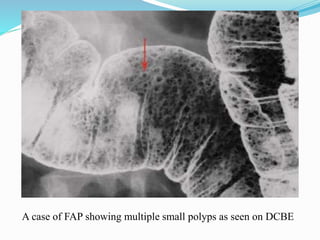
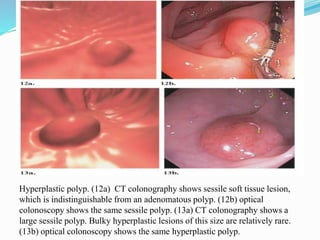
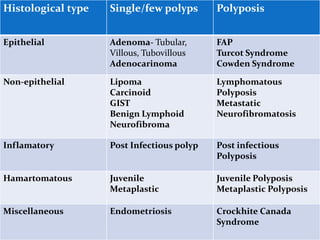
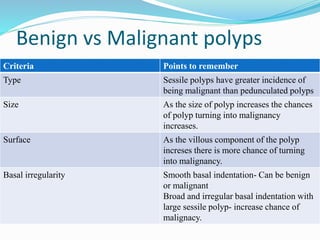
This document discusses colorectal polyps. It defines polyps and describes their types, including neoplastic and non-neoplastic polyps. It discusses adenomatous polyps in depth, noting their malignant potential increases with size over 1cm and villous architecture. Radiological diagnostic methods for polyps including single and double contrast barium enema and CT colonography are explained. The document provides an overview of polyp pathogenesis and genetic syndromes like FAP that increase cancer risk.