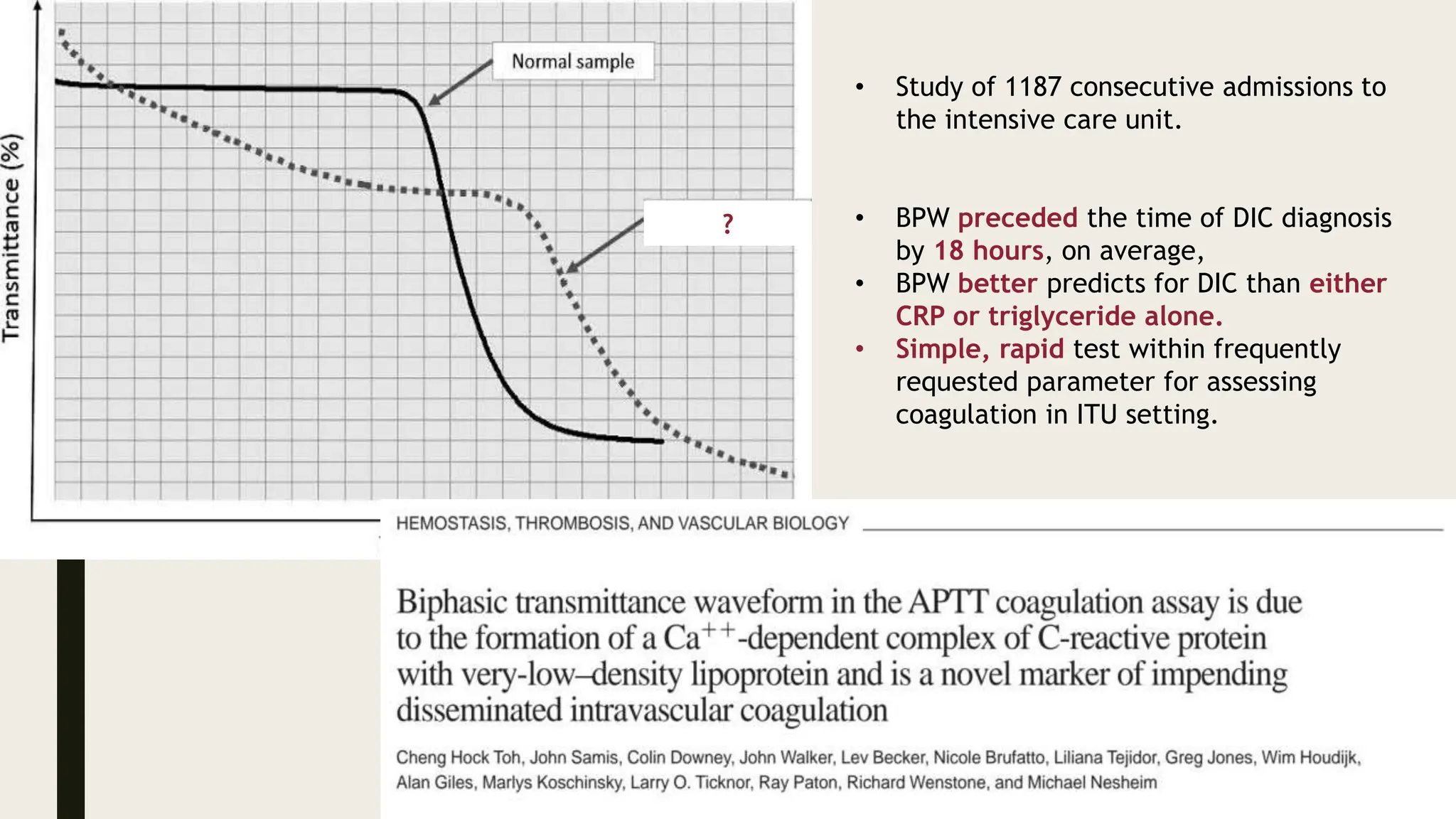
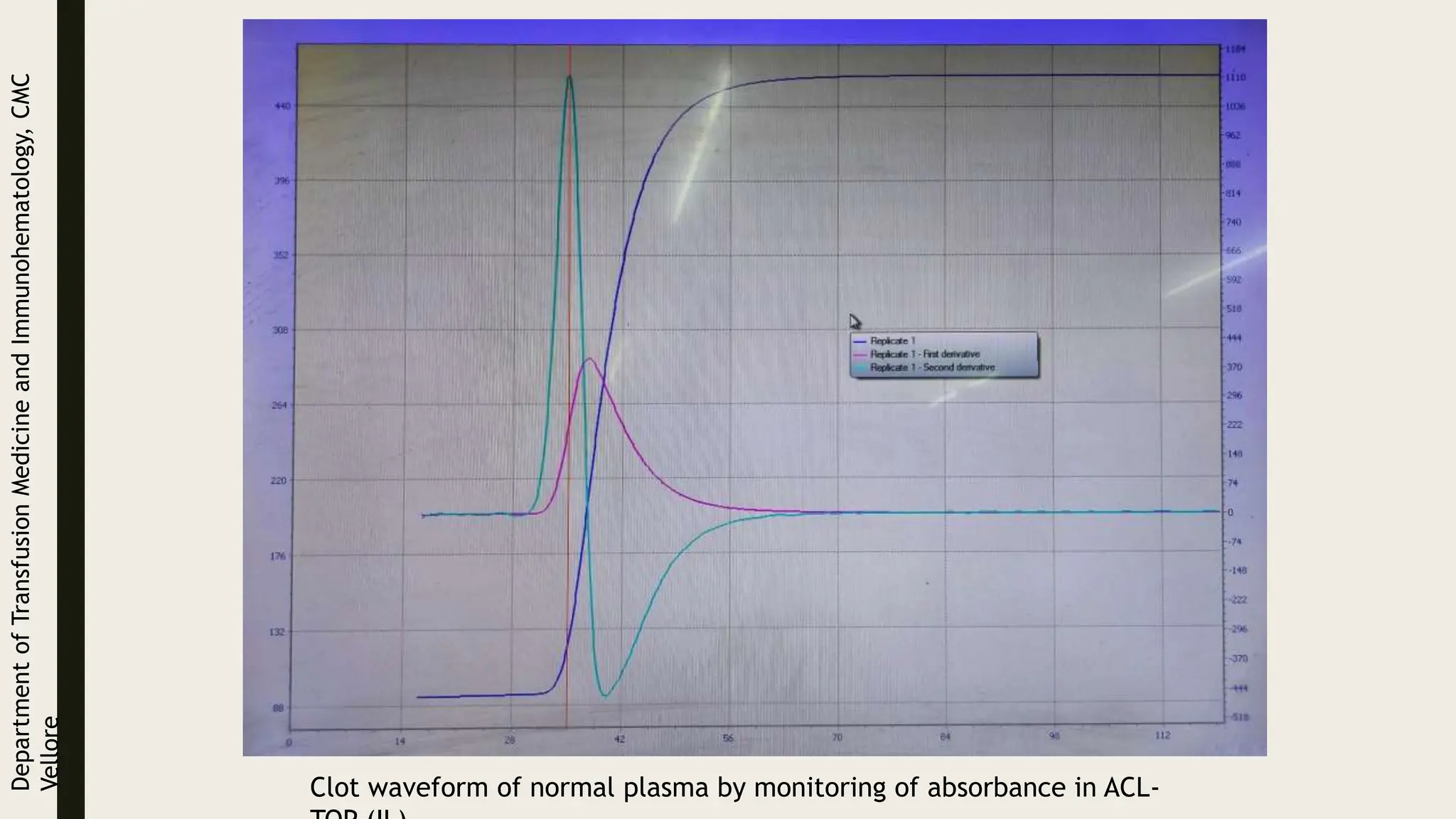
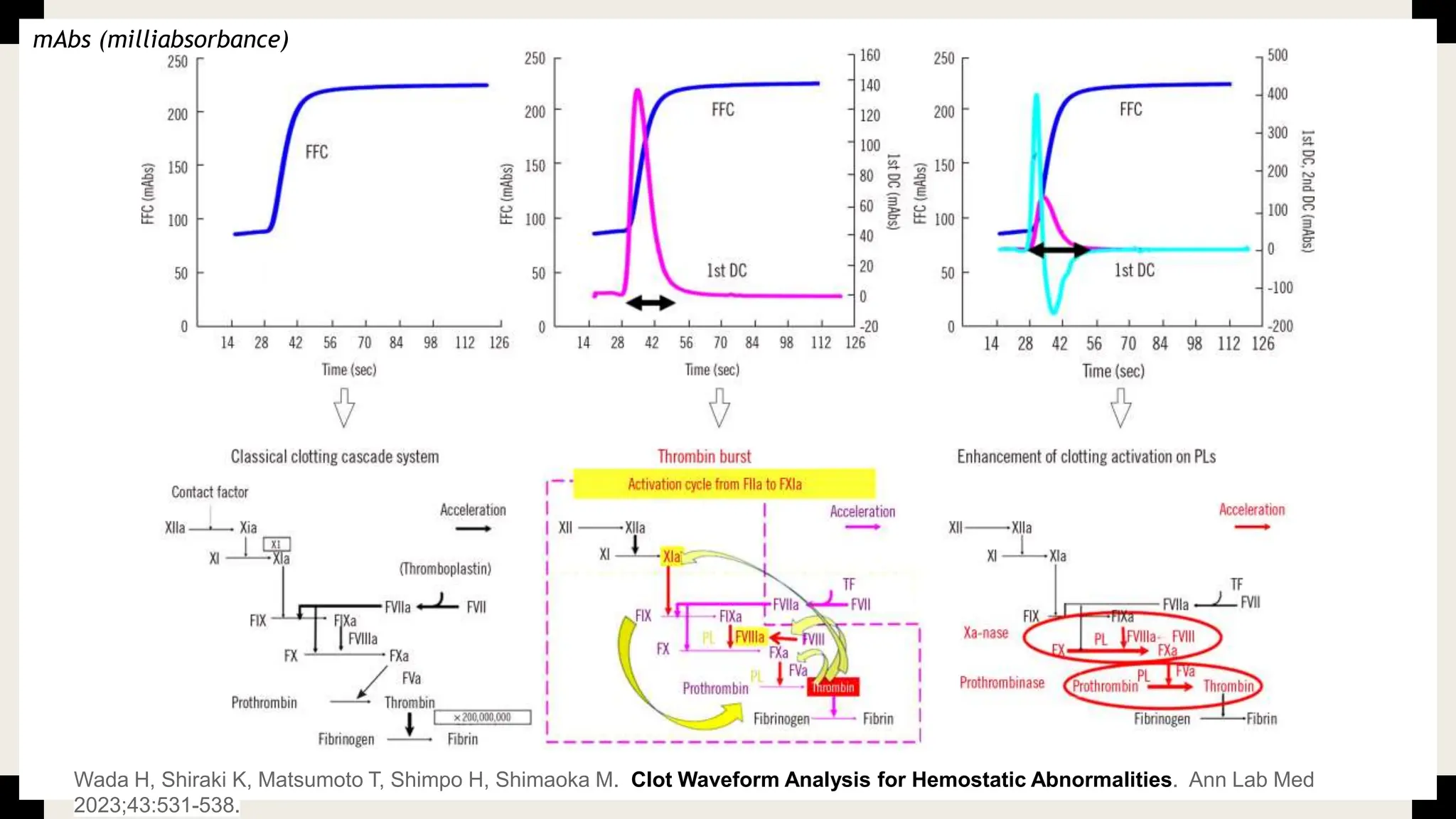
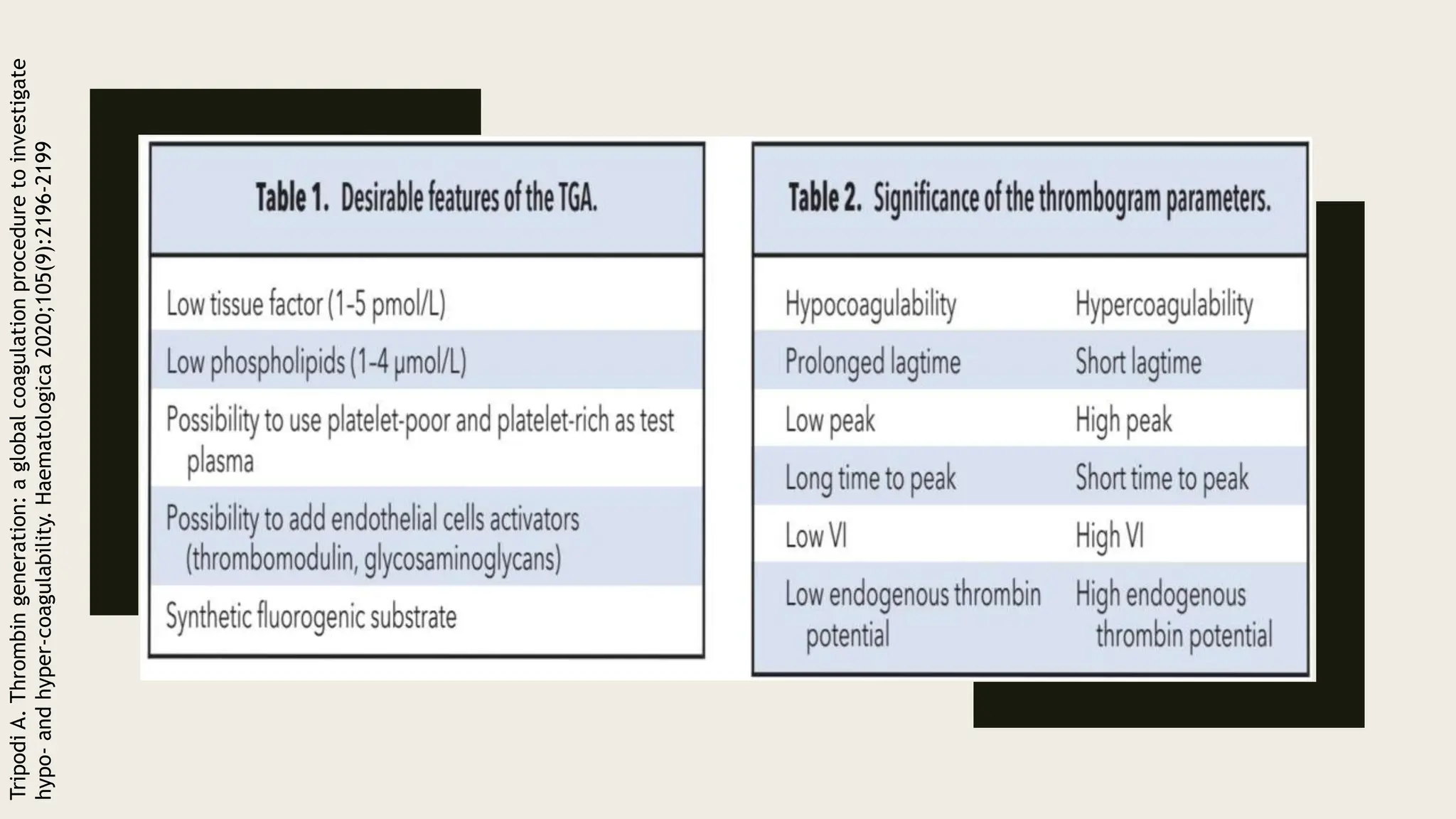
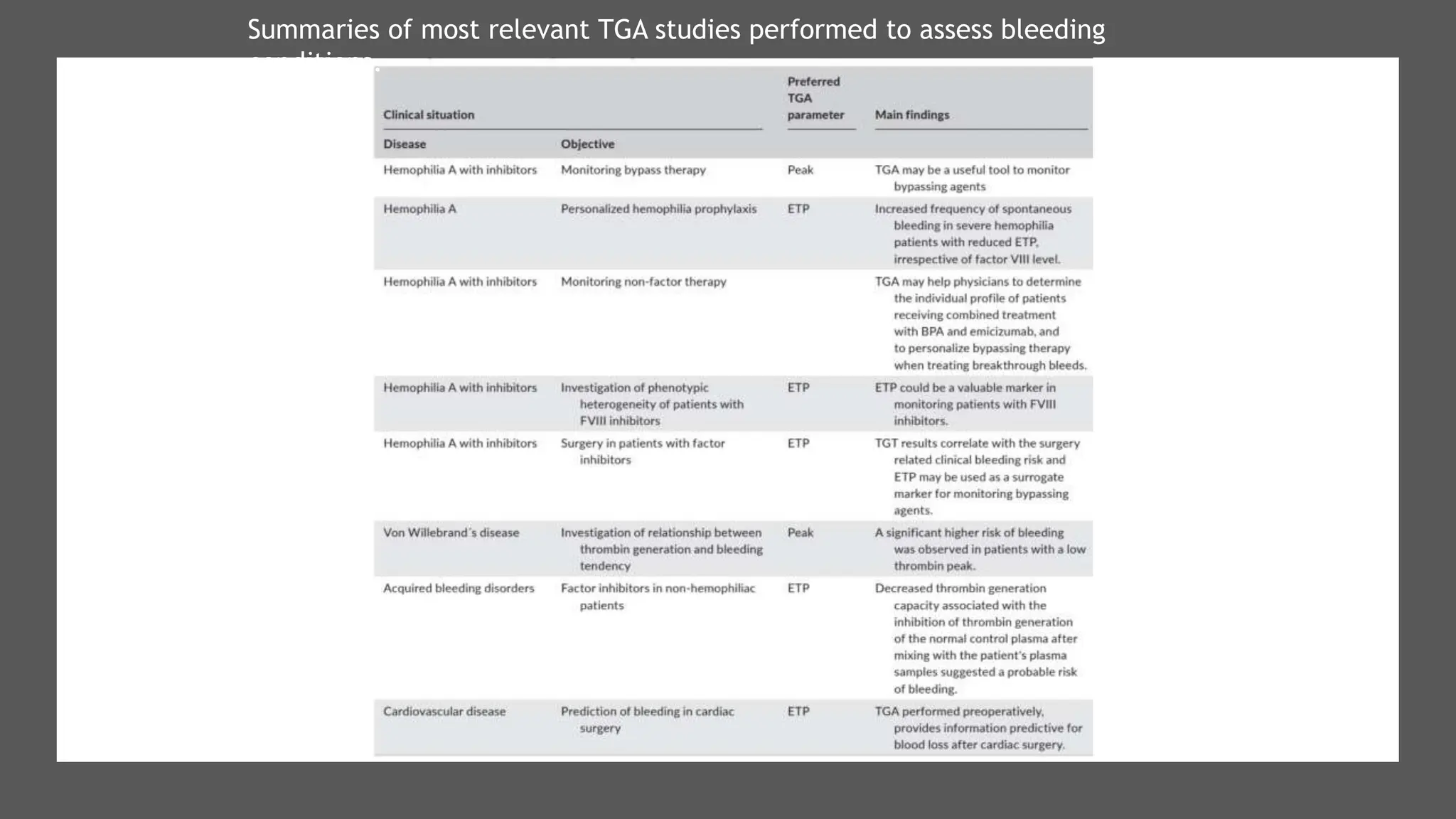
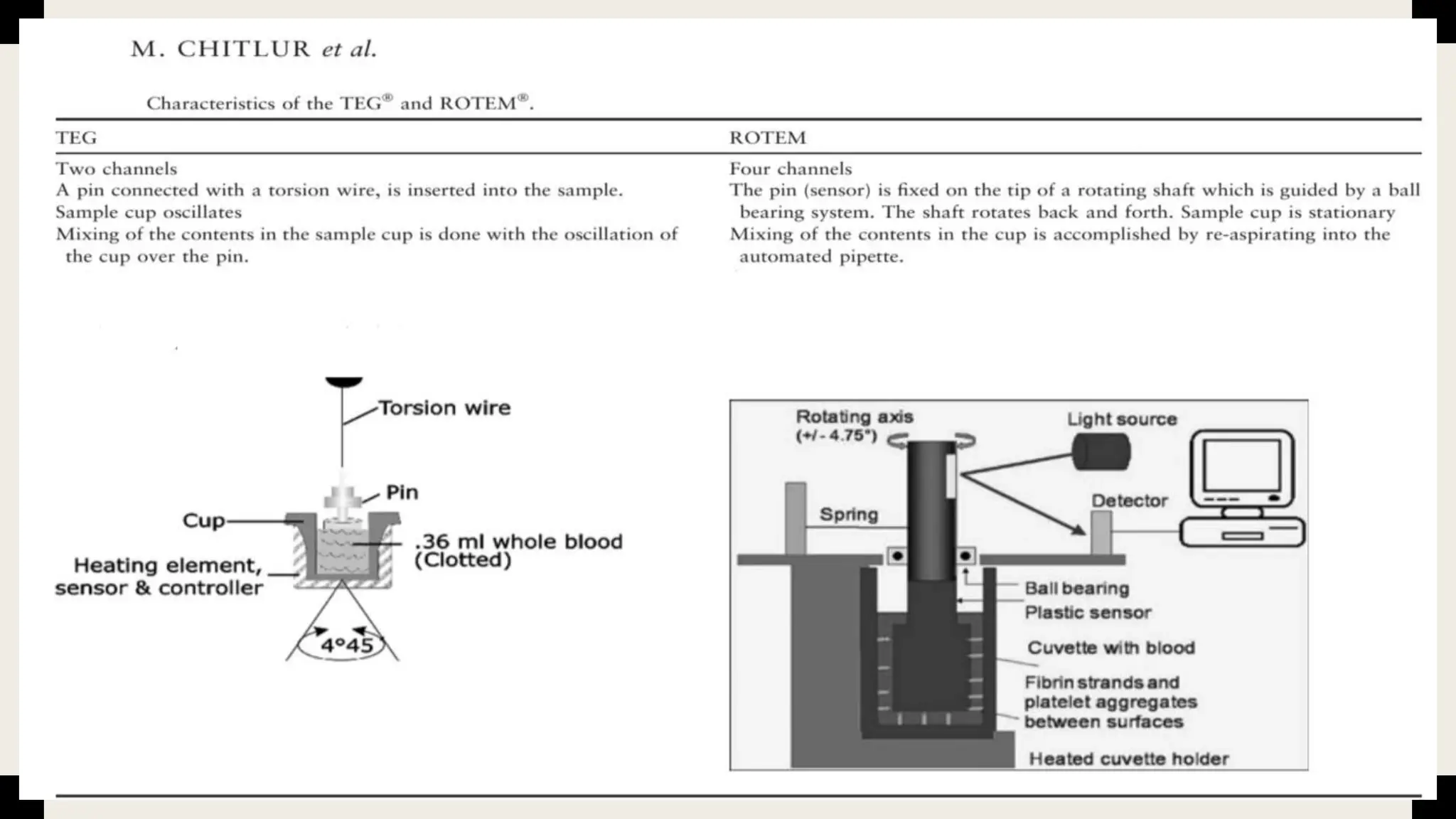
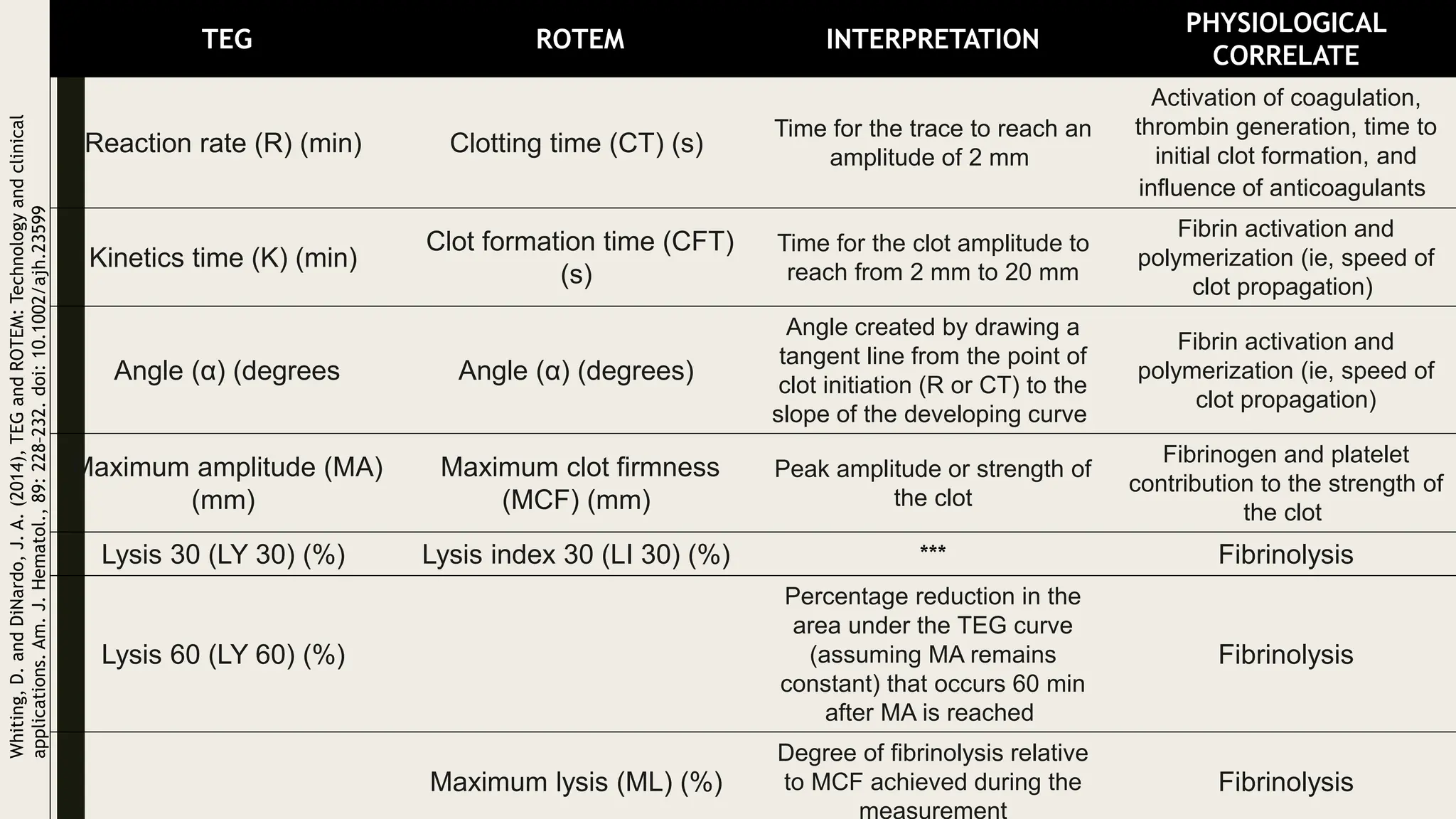
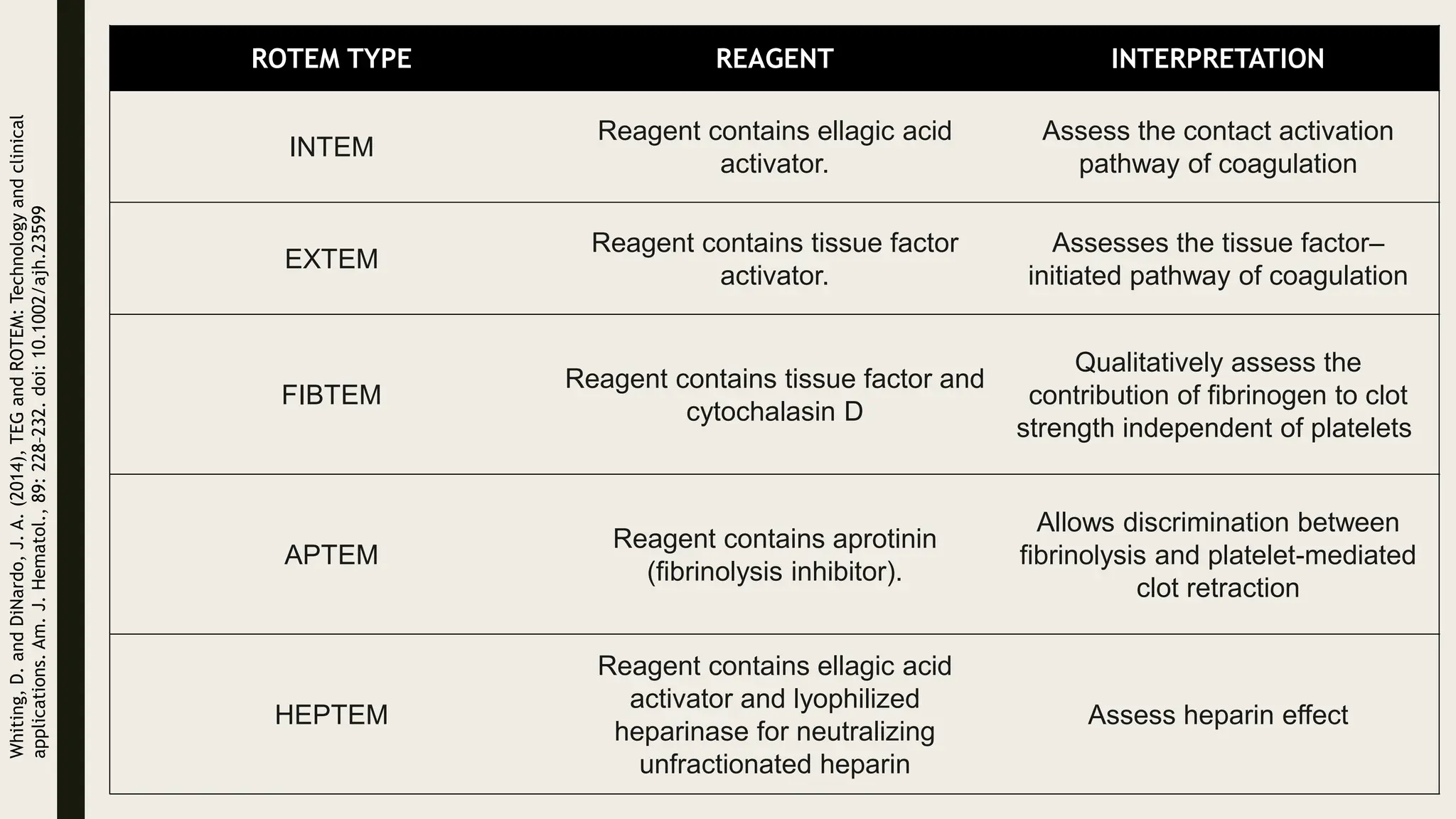
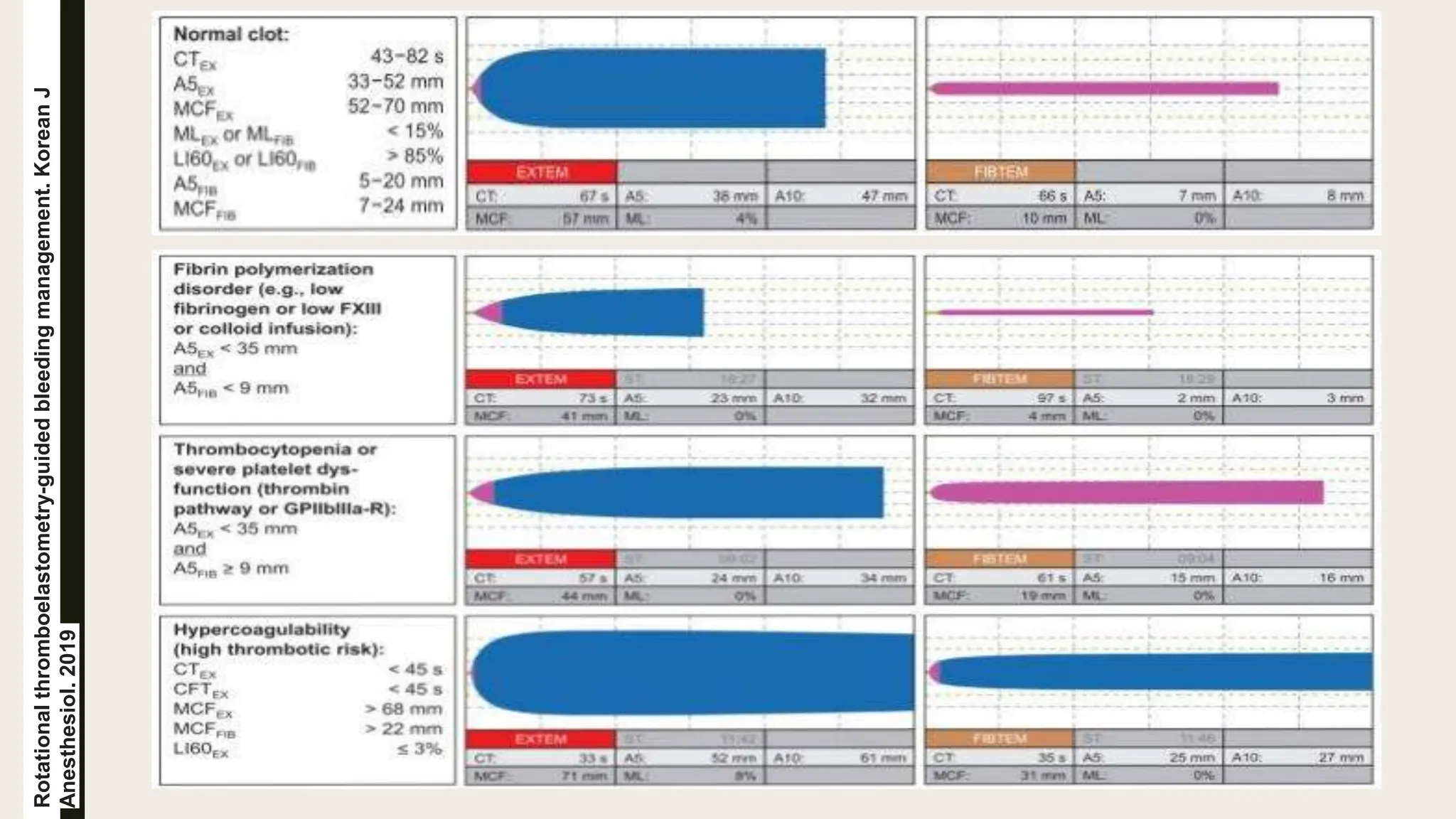
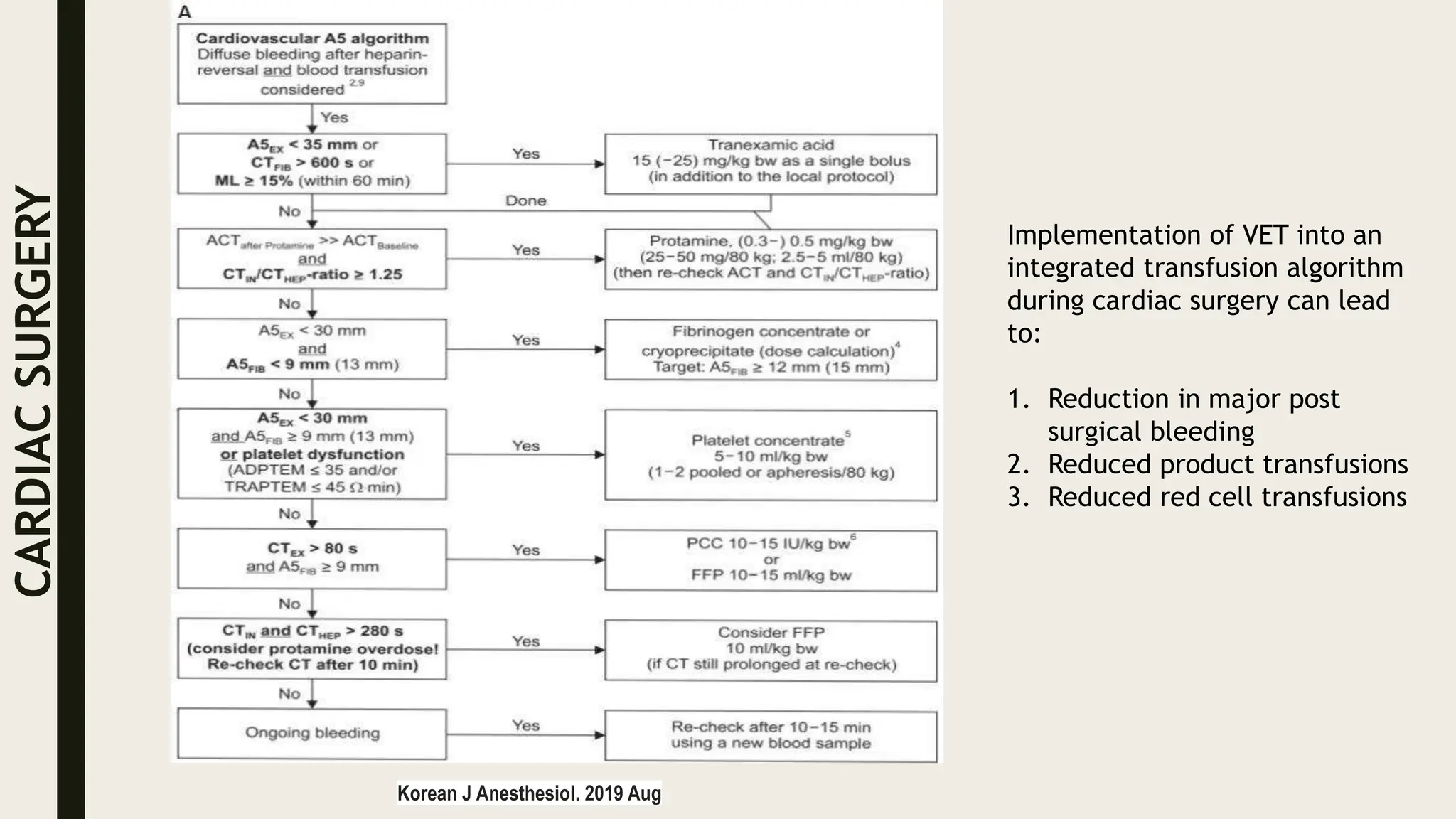
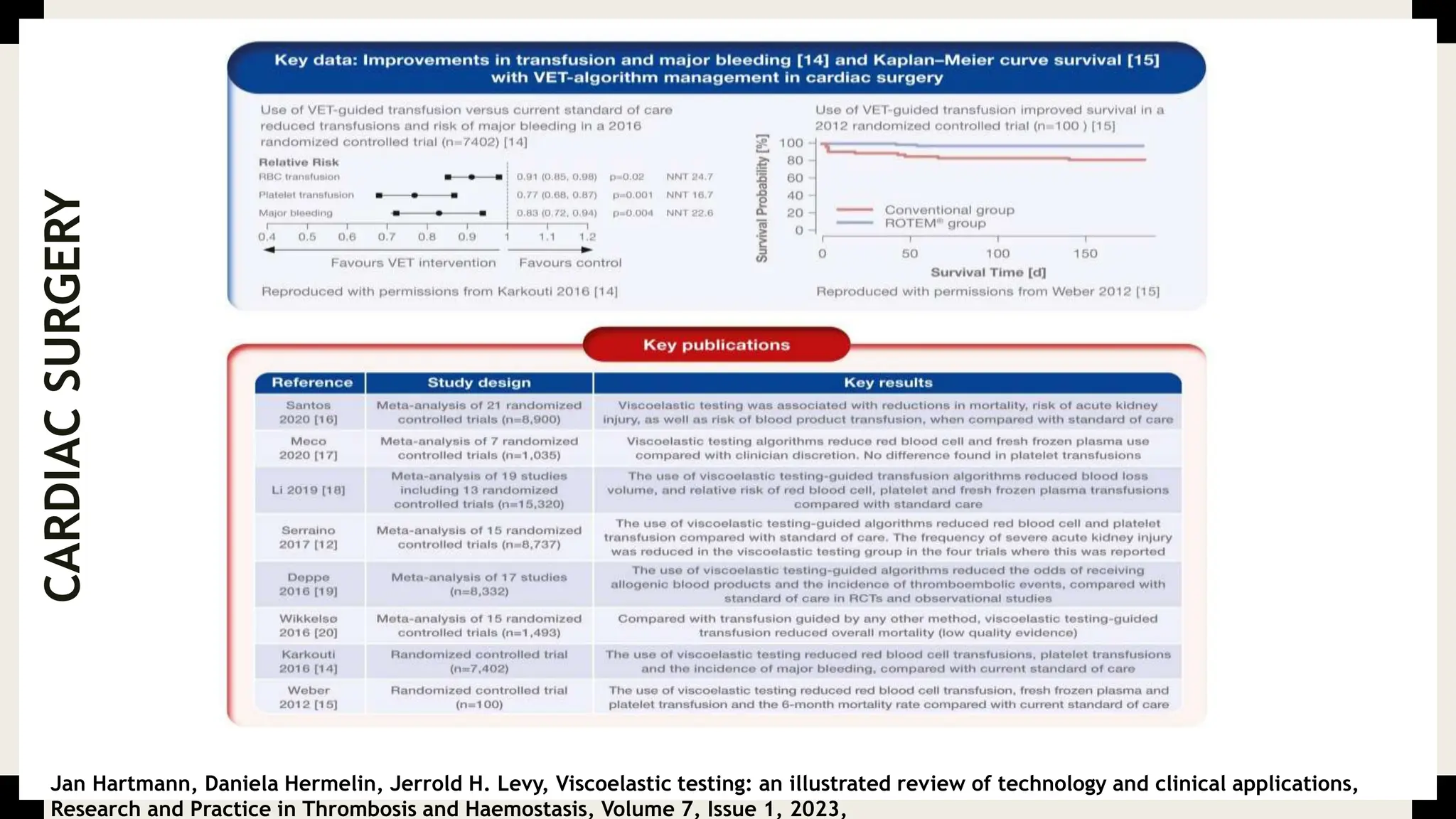
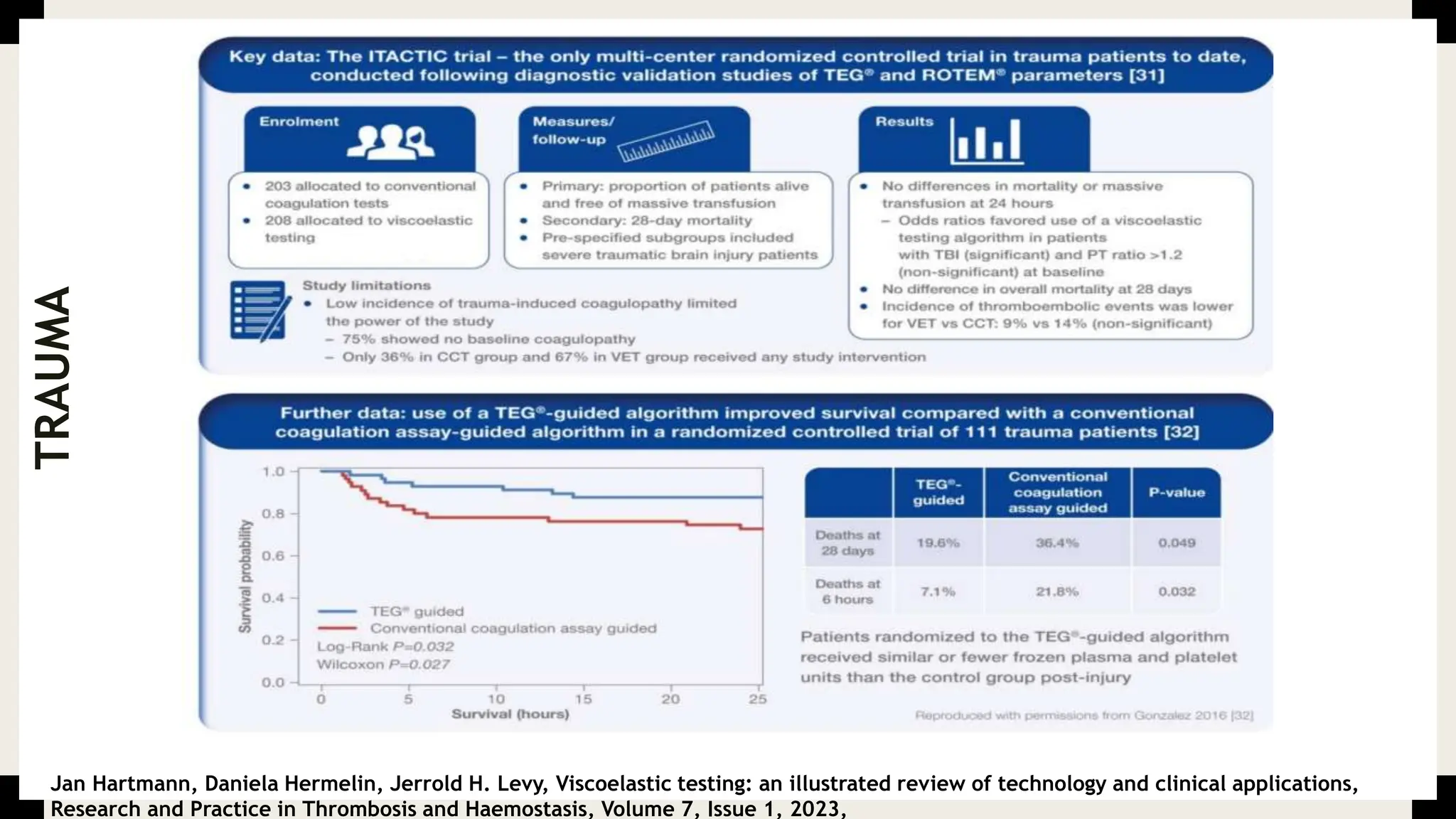
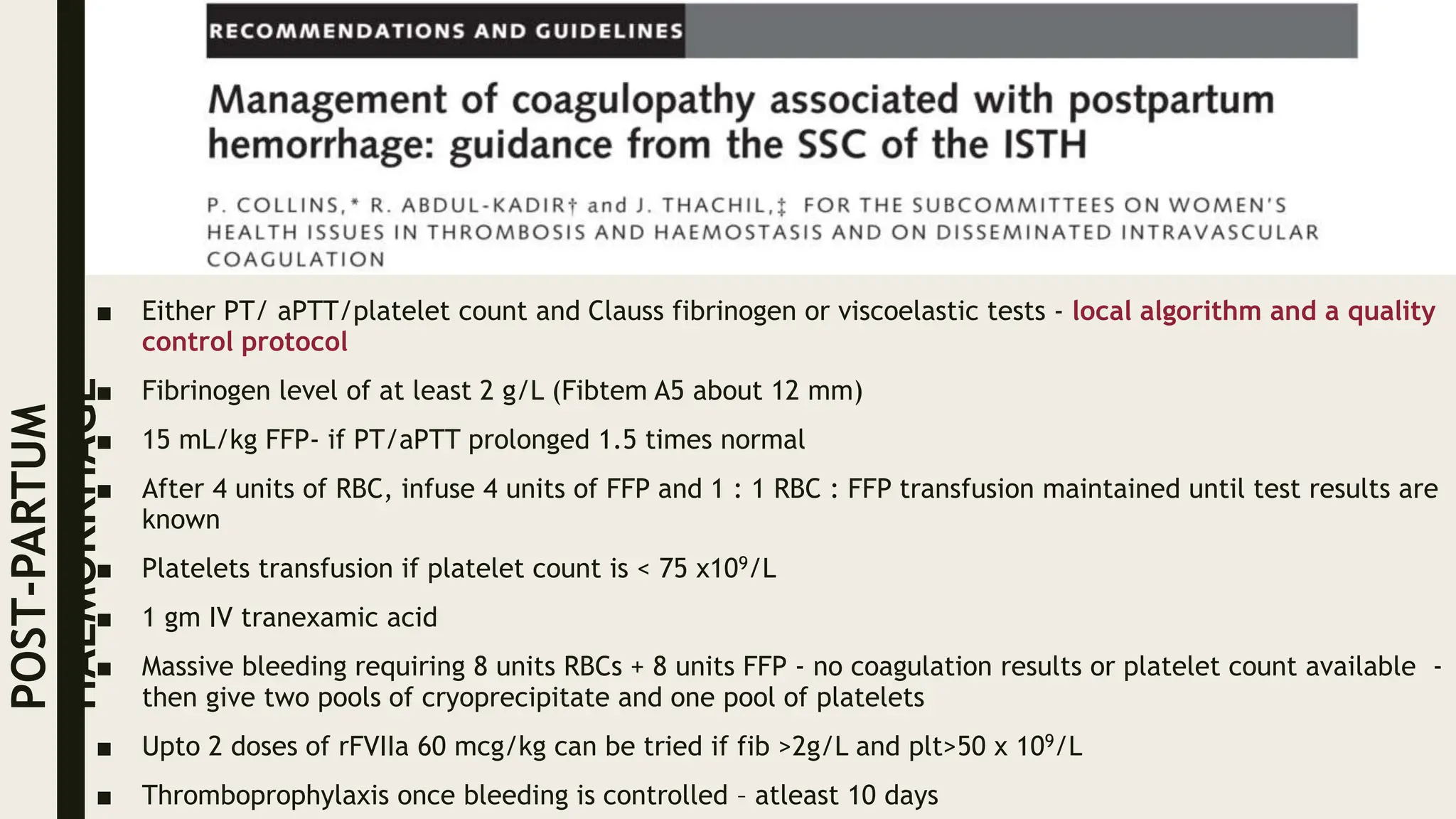
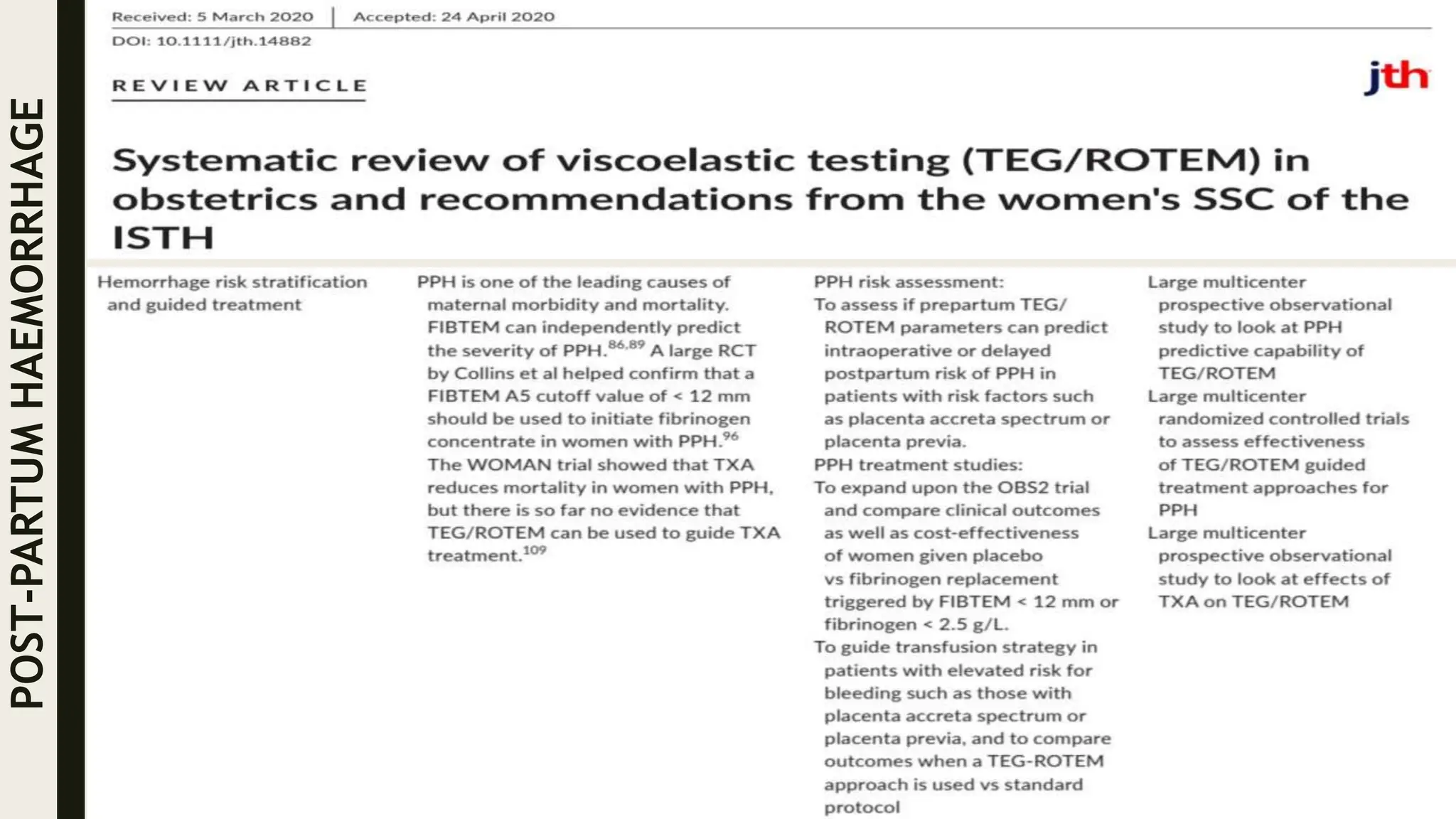
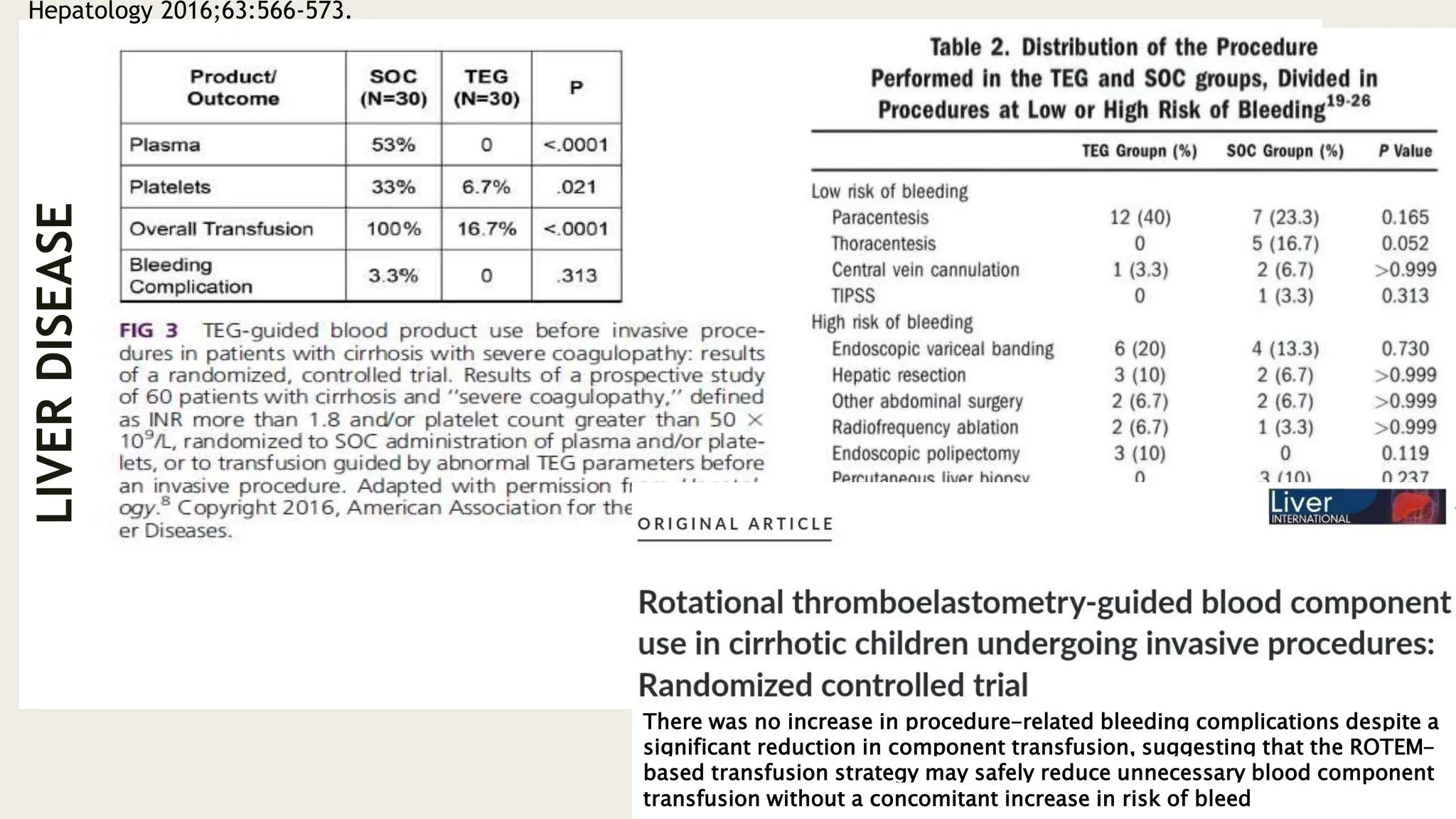
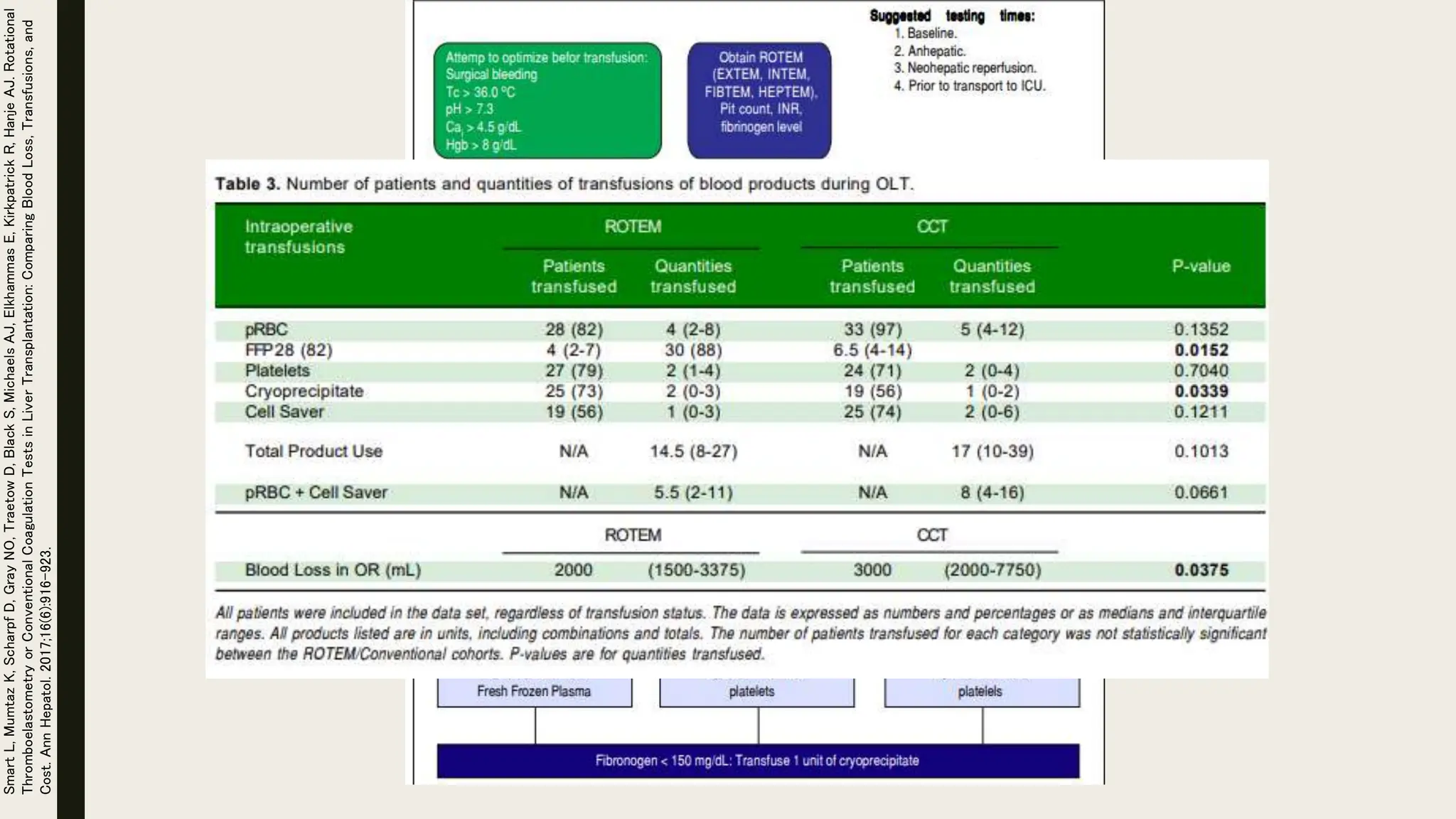
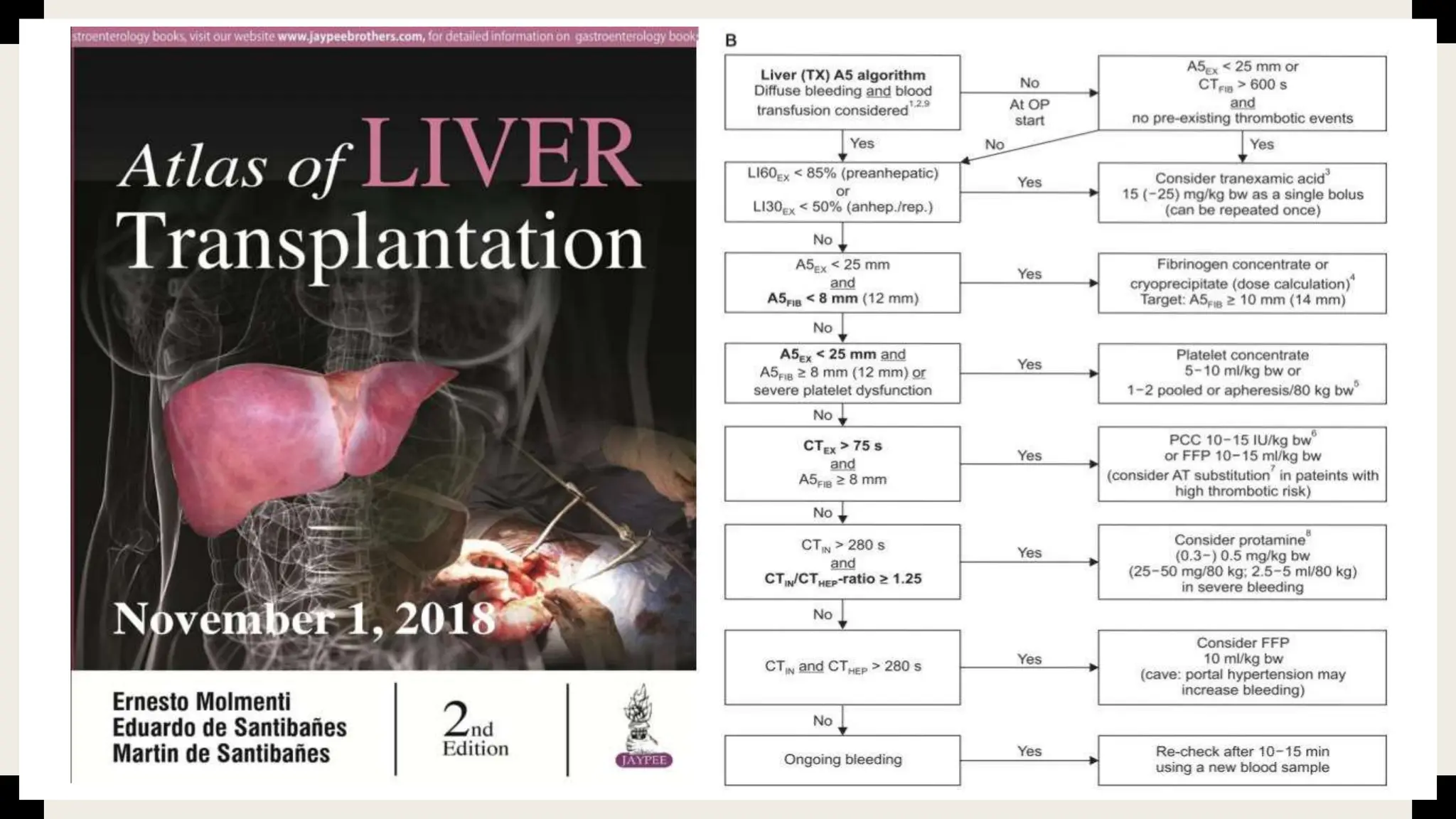
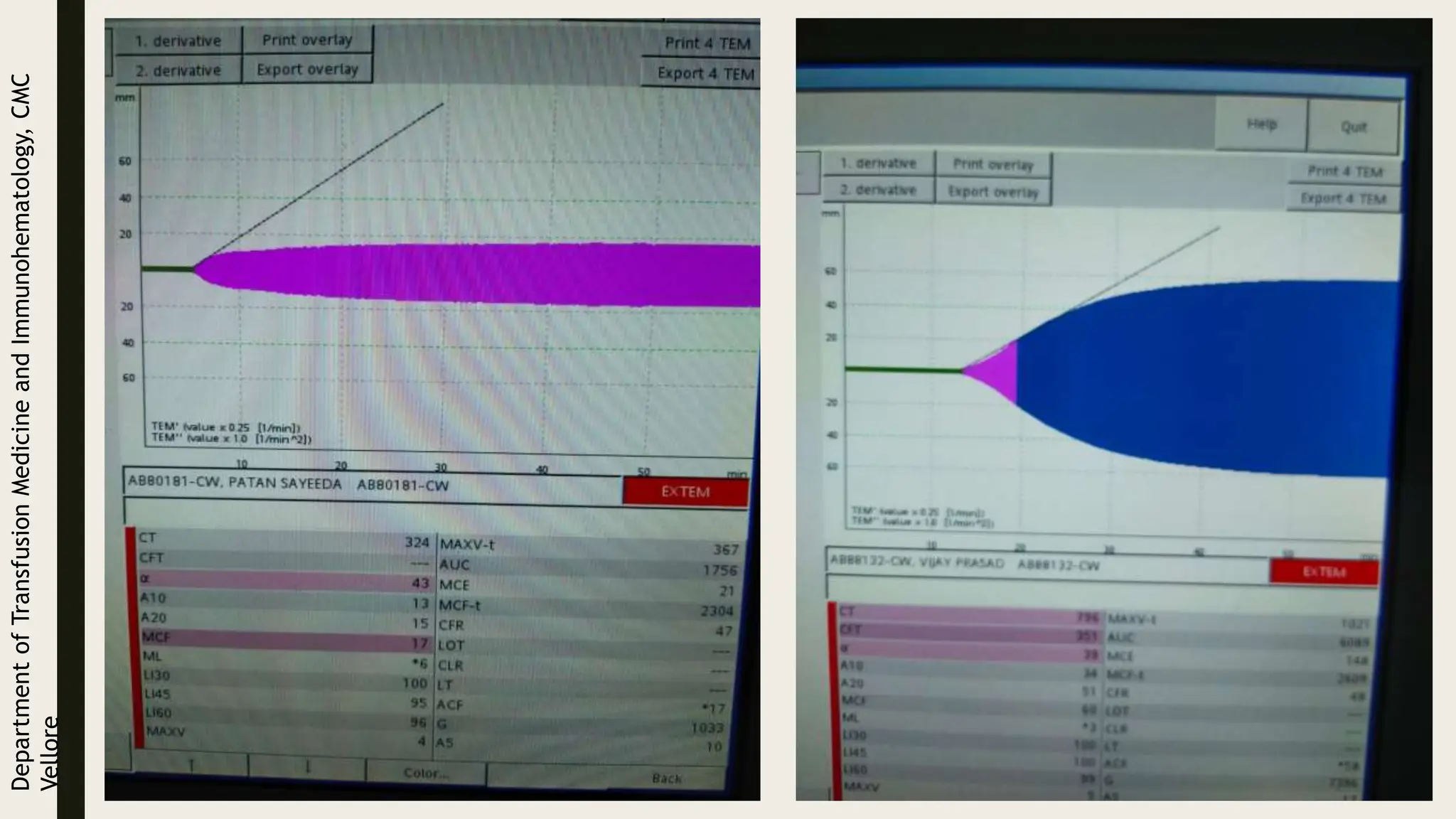
The document discusses various assays and models used to evaluate global hemostasis and coagulation, emphasizing the importance of thrombin and clot waveform analysis in diagnosing bleeding disorders and predicting thrombotic risks. It elaborates on the advancements in thrombin generation assays and viscoelastic testing techniques like TEG and ROTEM for clinical applications, particularly in trauma and surgical settings. Recommendations for testing protocols and interpretations are provided to enhance the management of coagulation-related issues.