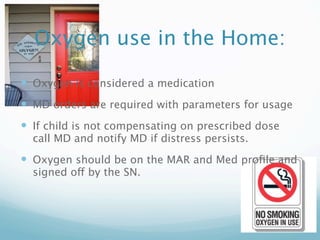
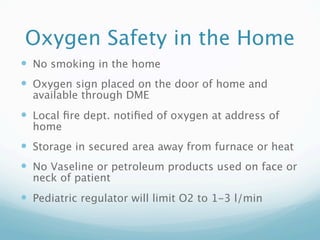
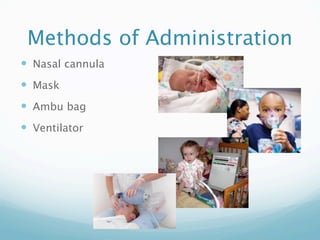
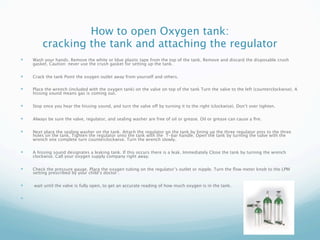
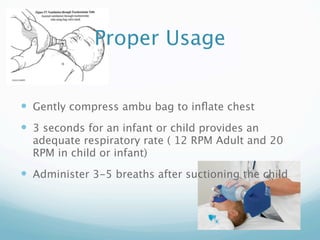
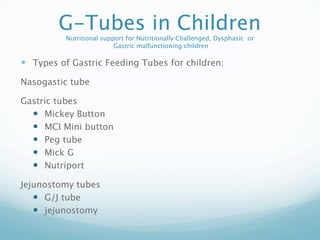
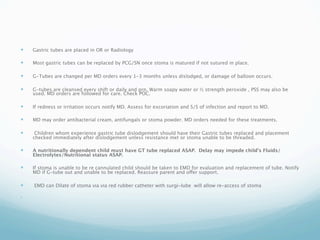
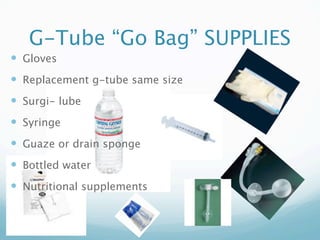
This document provides information on oxygen use and pediatric respiratory treatments in the home setting. It discusses oxygen orders and monitoring, nebulizer treatments, oxygen safety, administration methods including nasal cannula and mask, and types of humidification. It also covers opening oxygen tanks, attaching regulators, types of oxygen, using Ambu bags properly, tracheotomy care in children, and feeding tubes in children including common types like G-tubes and their replacement and care.