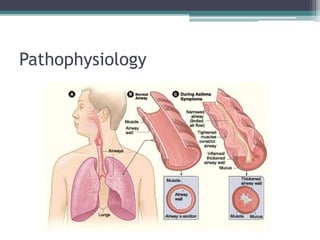
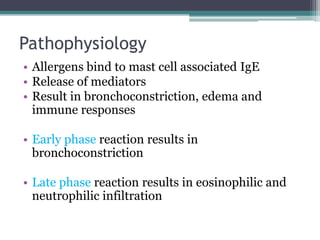
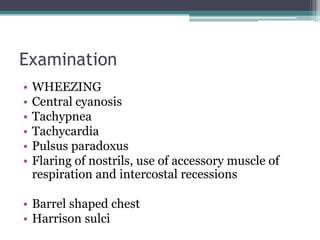
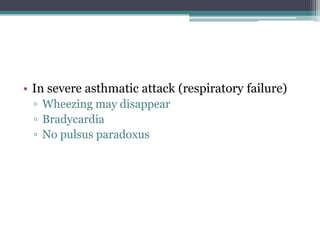
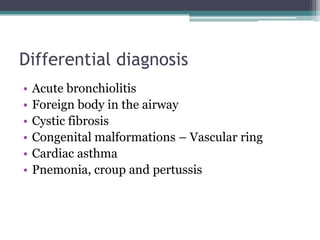
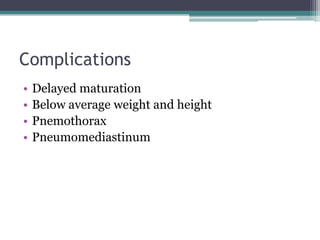
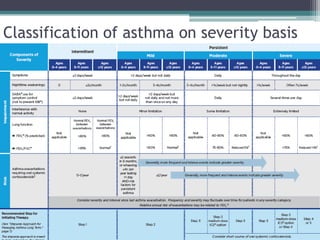
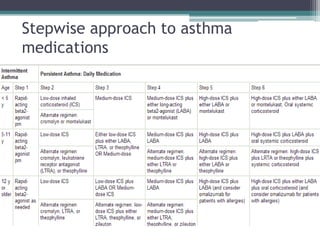
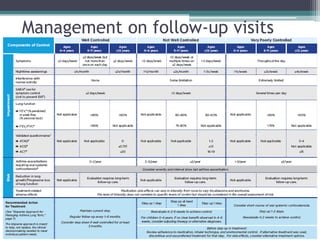
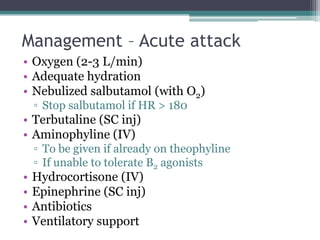
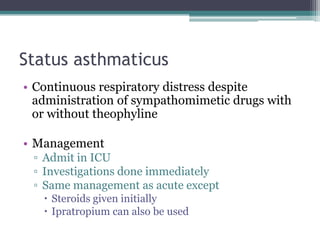
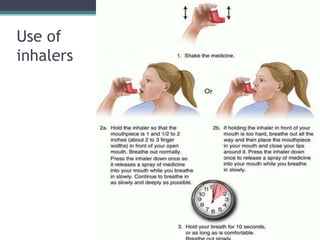
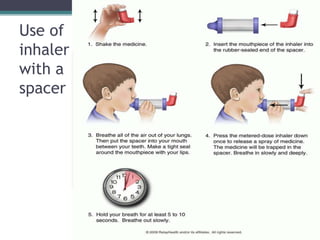
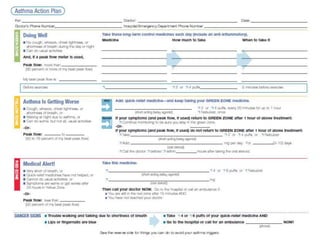
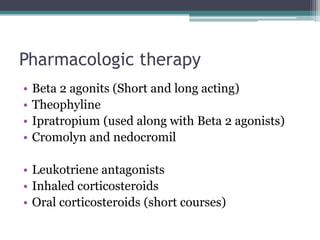
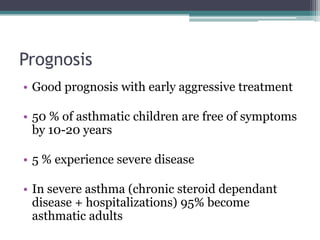
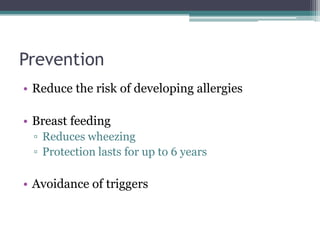
Asthma is a reversible airway obstruction often triggered by factors like infections and weather changes, more common in boys before puberty. Its pathophysiology includes inflammation and bronchospasm, with clinical manifestations such as cough, shortness of breath, and wheezing. Management involves acute treatment options like bronchodilators and steroids, and chronic care focusing on patient education, trigger avoidance, and pharmacologic therapy.