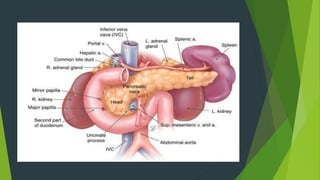
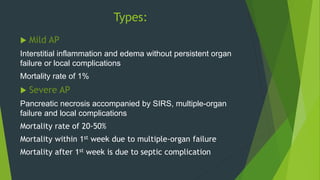
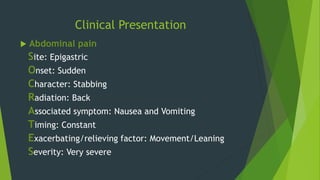
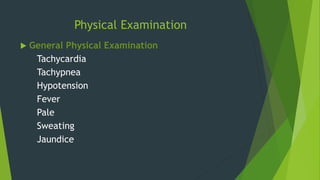
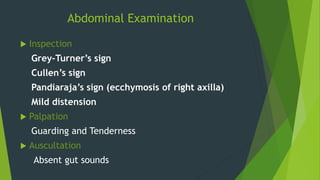
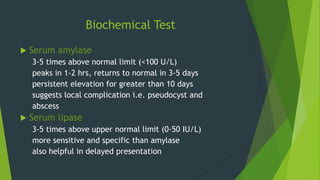
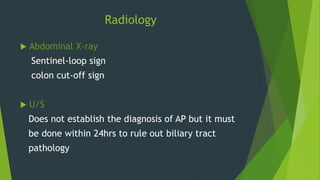
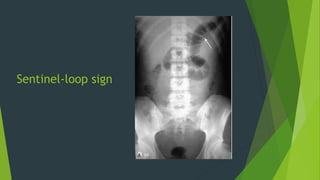
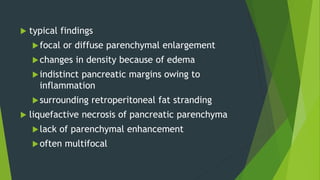
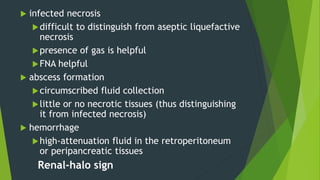
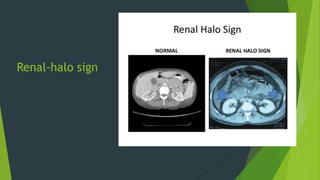
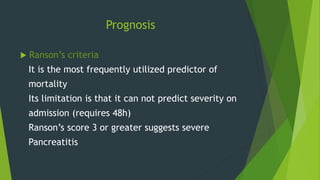
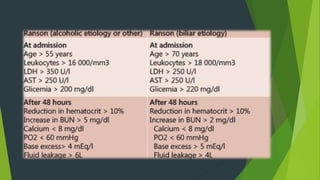
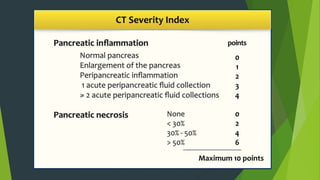
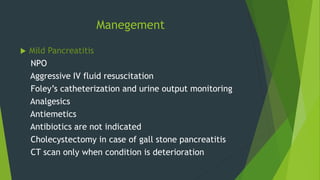
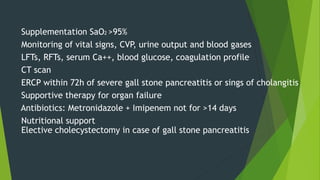
The document provides a detailed overview of acute pancreatitis, including its anatomy, causes, diagnosis, clinical presentation, and management. It categorizes the condition into mild and severe types, discussing various diagnostic tests and prognostic criteria like Ranson’s criteria and CT severity index. The management strategies vary based on severity, with guidelines for both mild and severe cases outlined, highlighting potential complications and necessary interventions.