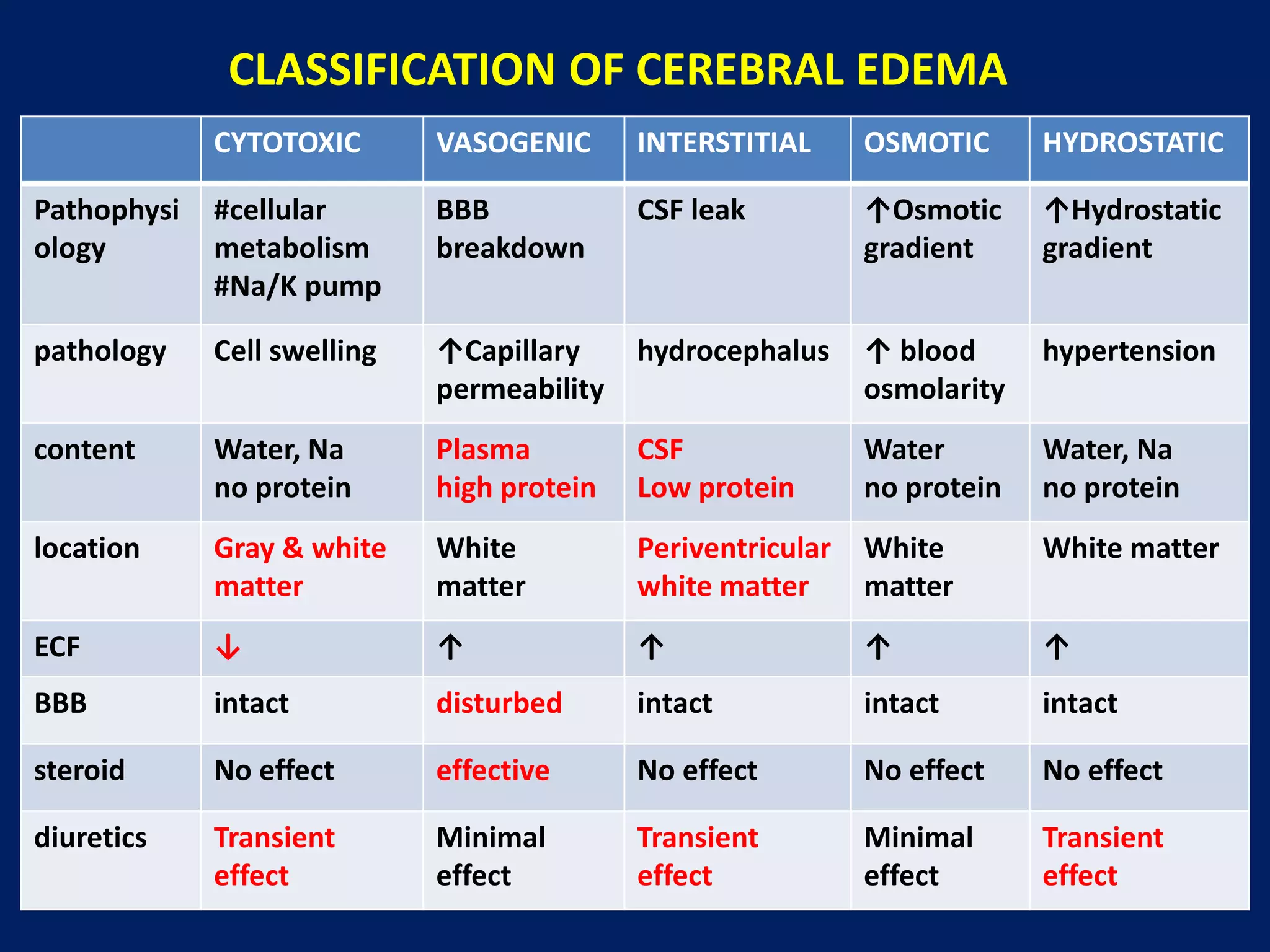
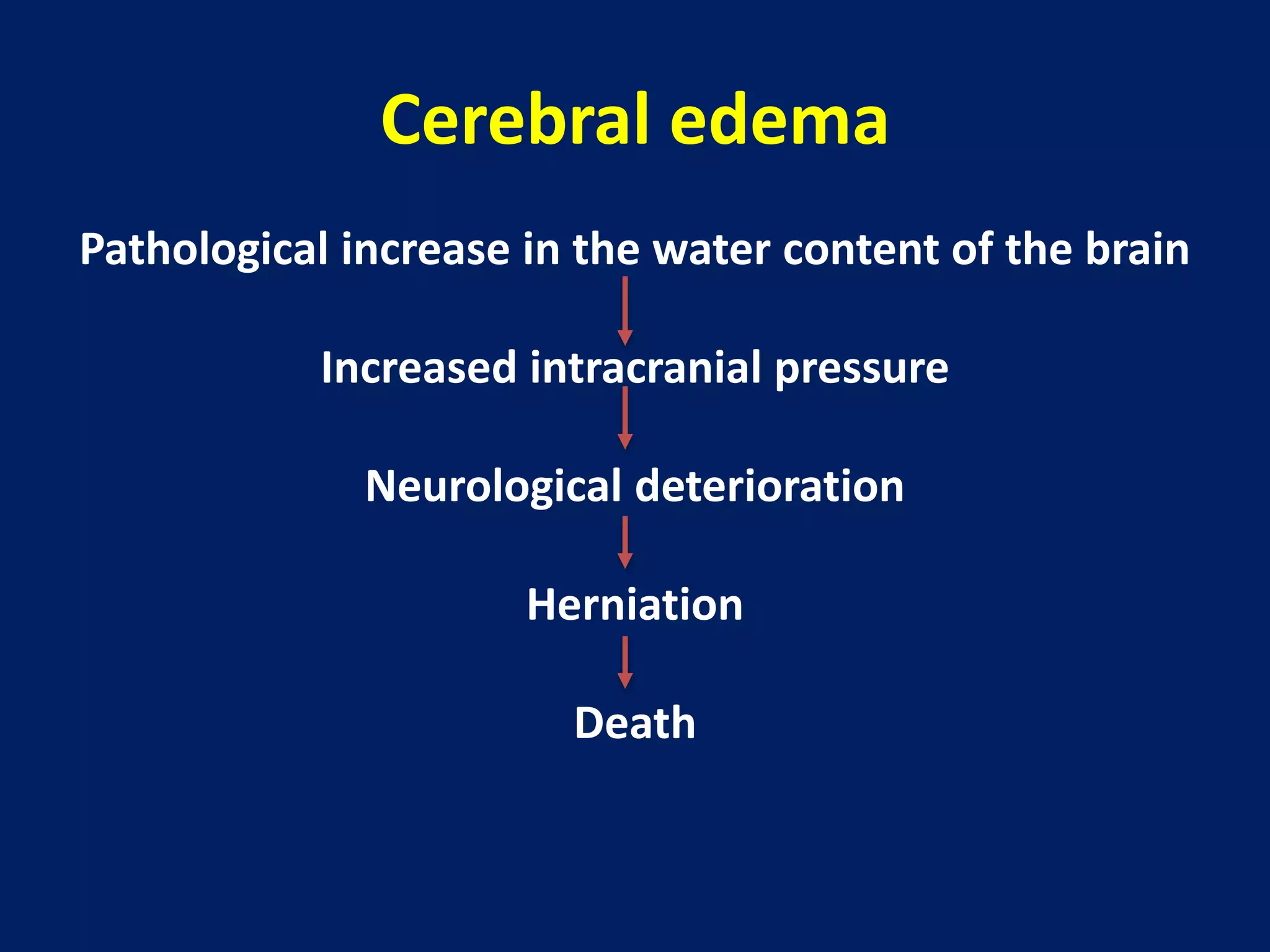
1. Cerebral edema occurs when there is abnormal accumulation of fluid in the brain parenchyma, increasing brain volume and intracranial pressure.
2. It can be caused by traumatic brain injury, stroke, tumors, or other conditions that disrupt the blood-brain barrier.
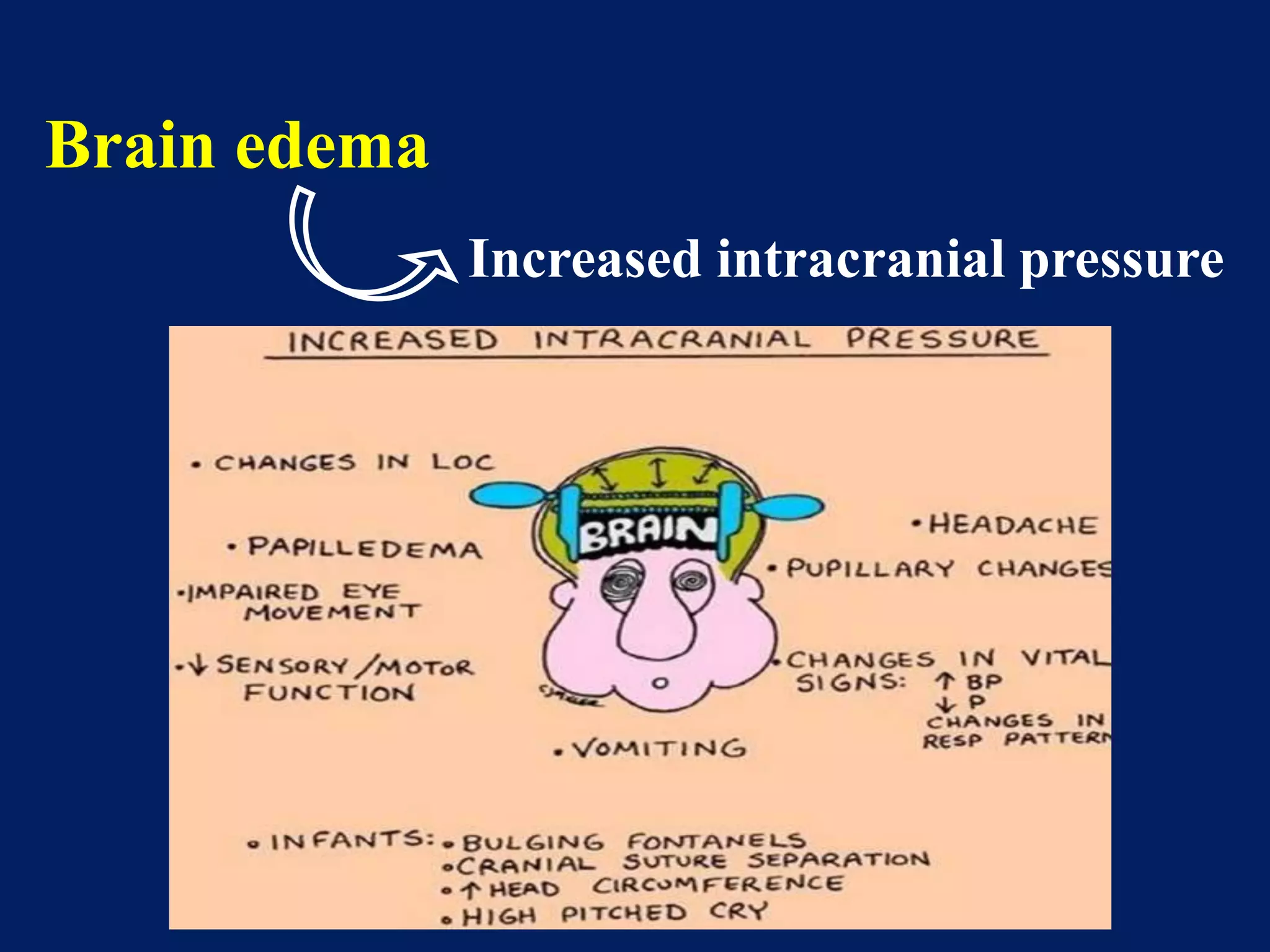
3. Increased intracranial pressure from cerebral edema can cause neurological deterioration and herniation if not treated.
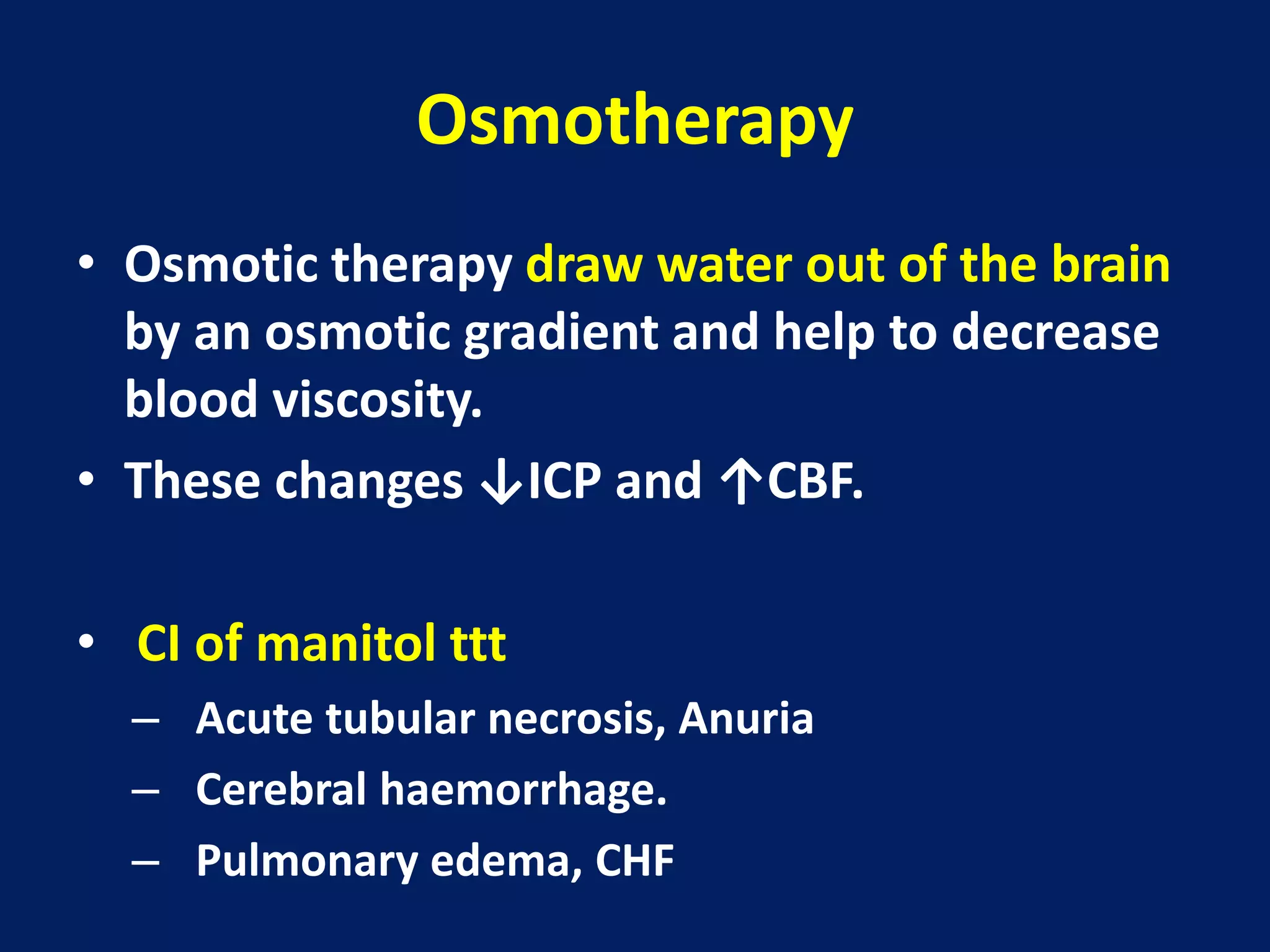
4. Management involves controlling intracranial pressure, optimizing ventilation and oxygenation, administering osmotherapy agents like mannitol to draw water out of the brain, and in severe cases surgery may be needed.