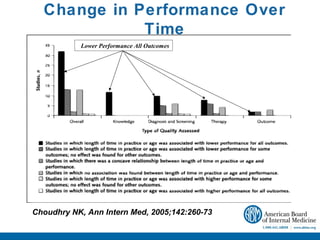
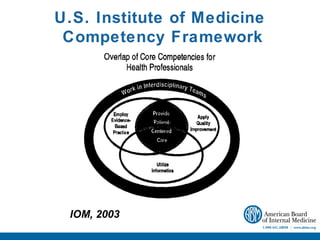
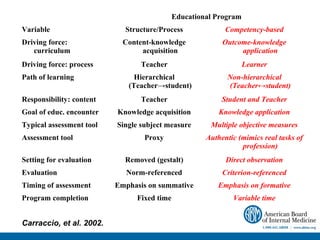
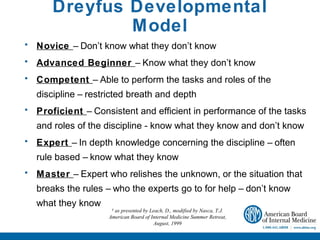
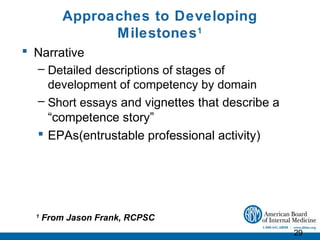
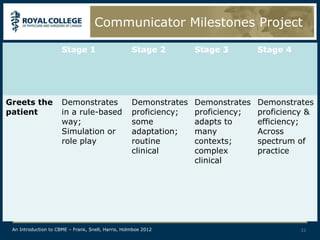
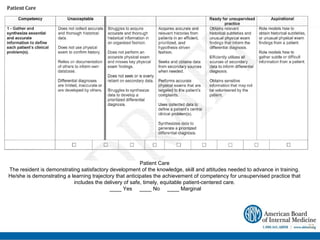
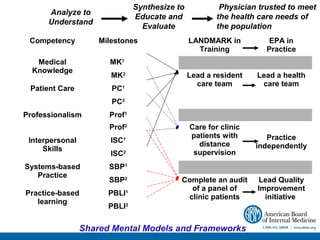
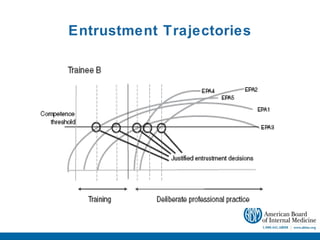
The document discusses competency-based medical education across the continuum of training. It begins by outlining the speaker's conflicts of interest in assessment-related organizations. The objectives are then stated as discussing the roles of assessment in a competency-based program, developing approaches to effective assessment, and integrating assessment into Memorial University's education system. Milestones and entrustable professional activities are presented as frameworks to assess competency development longitudinally. Challenges of assessment across training levels and principles of competency-based assessment are also addressed.