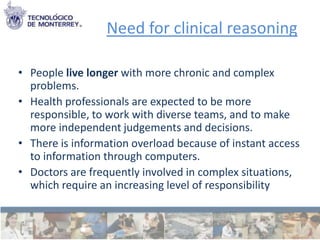
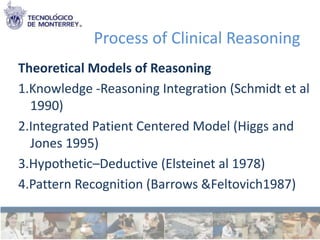
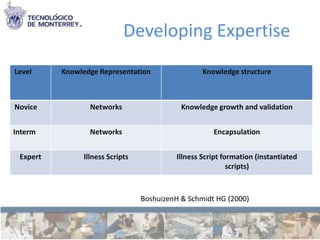
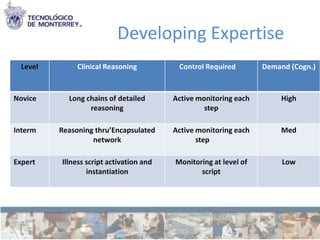
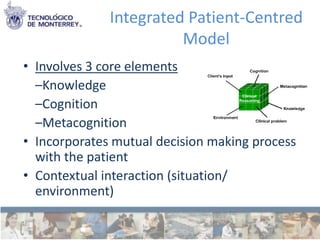
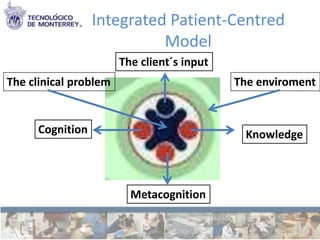
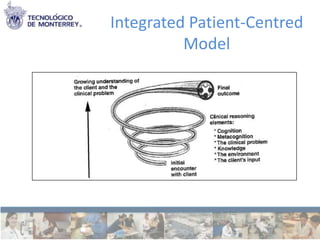
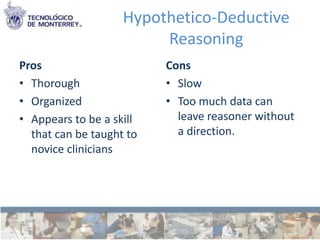
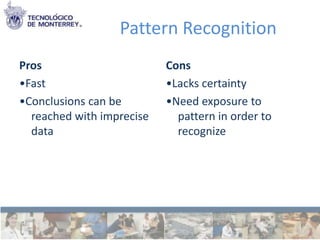
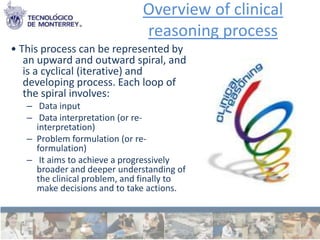
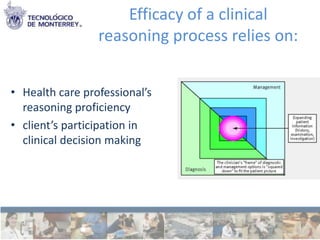
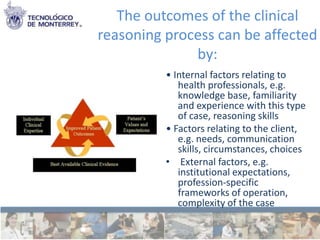
This document discusses clinical reasoning, which refers to the thinking and decision-making processes used in clinical practice. It defines clinical reasoning as a process where clinicians structure meaning, goals, and health strategies based on clinical data, patient choices, professional judgment, and knowledge. The document then outlines several models of clinical reasoning, including knowledge-reasoning integration, integrated patient-centered reasoning, hypothetico-deductive reasoning, and pattern recognition. It also discusses how clinical reasoning skills develop from novice to expert and the importance of knowledge, cognition, metacognition, narrative reasoning, and collaboration in clinical decision making.