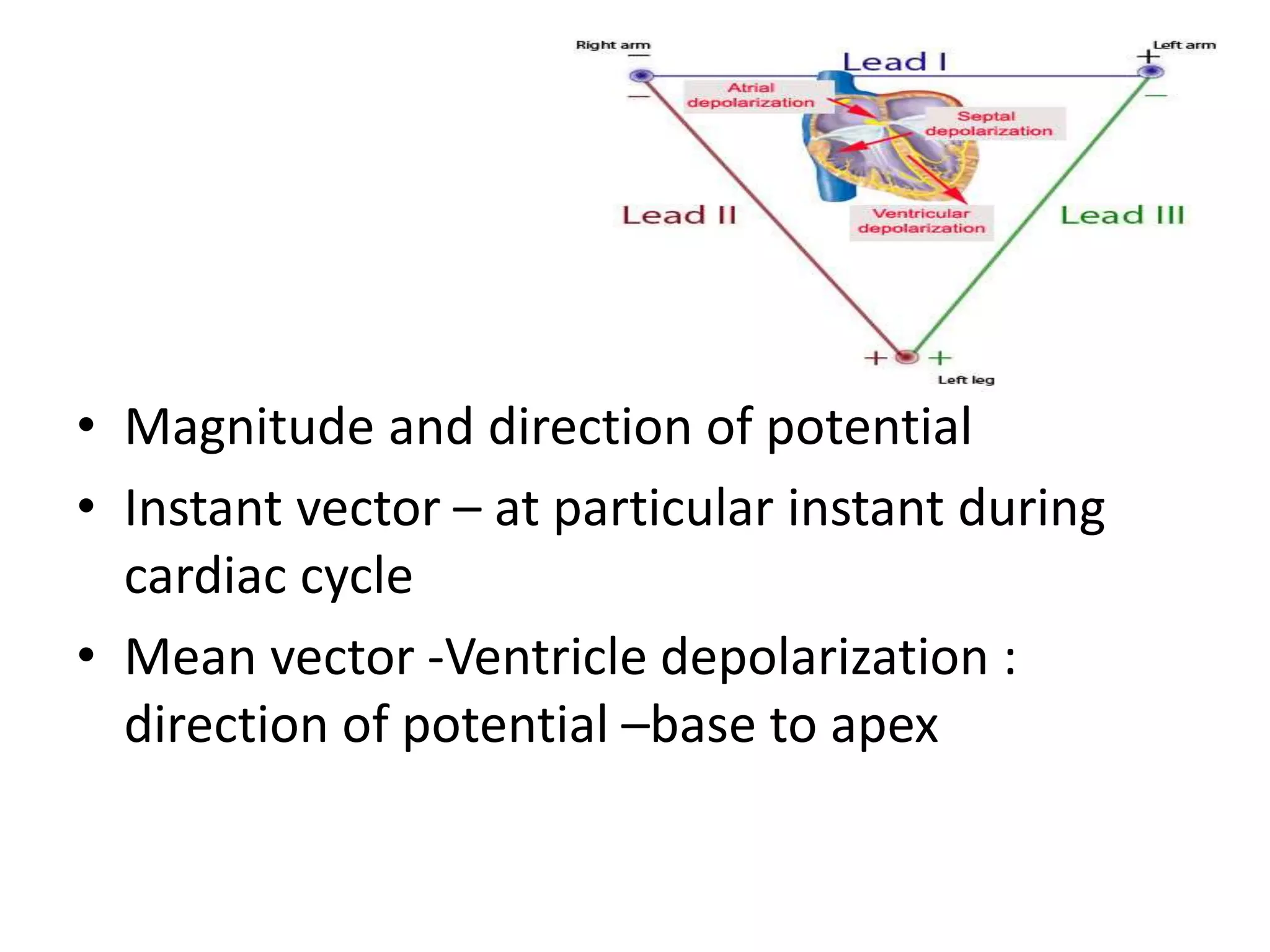
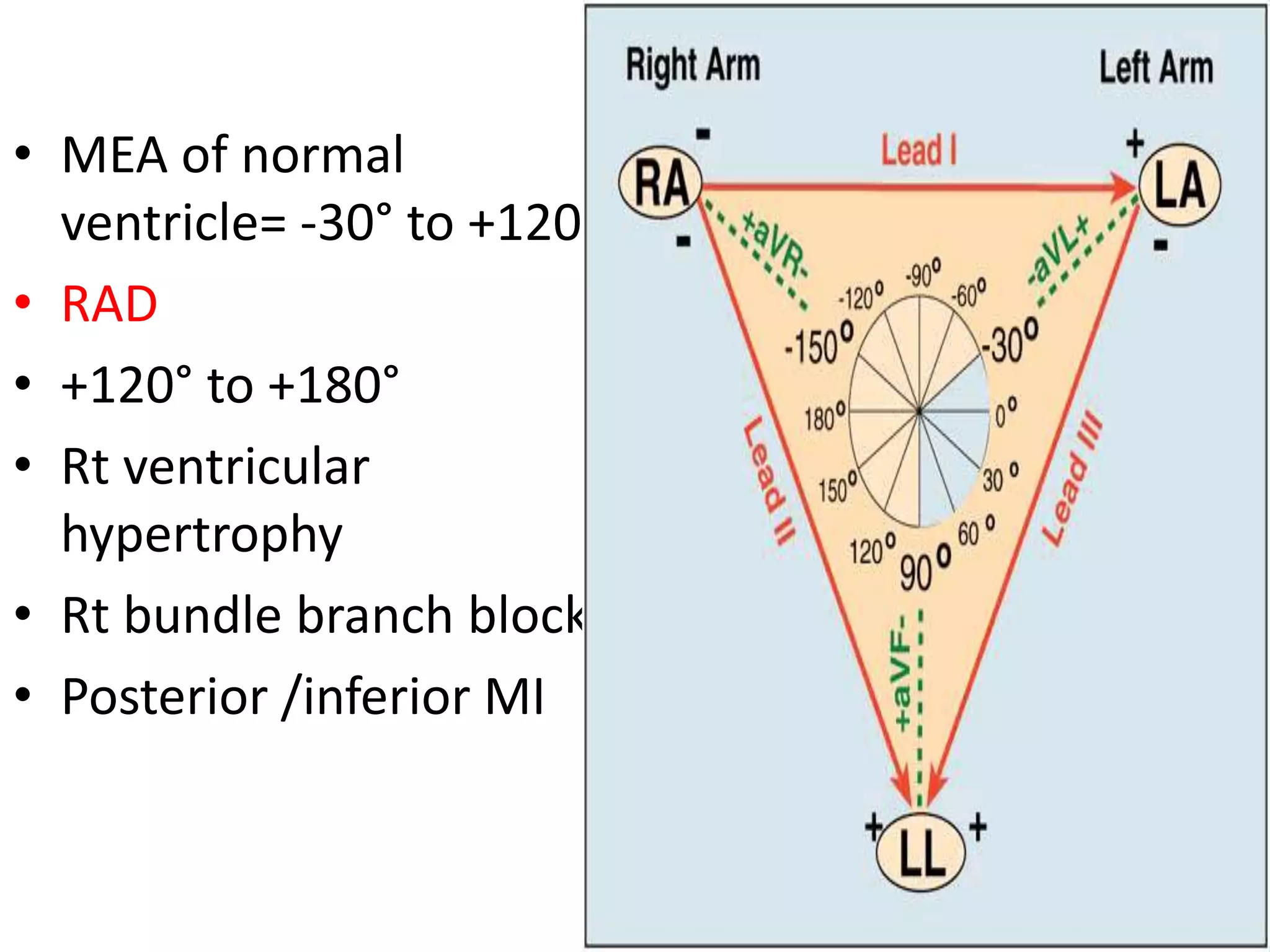
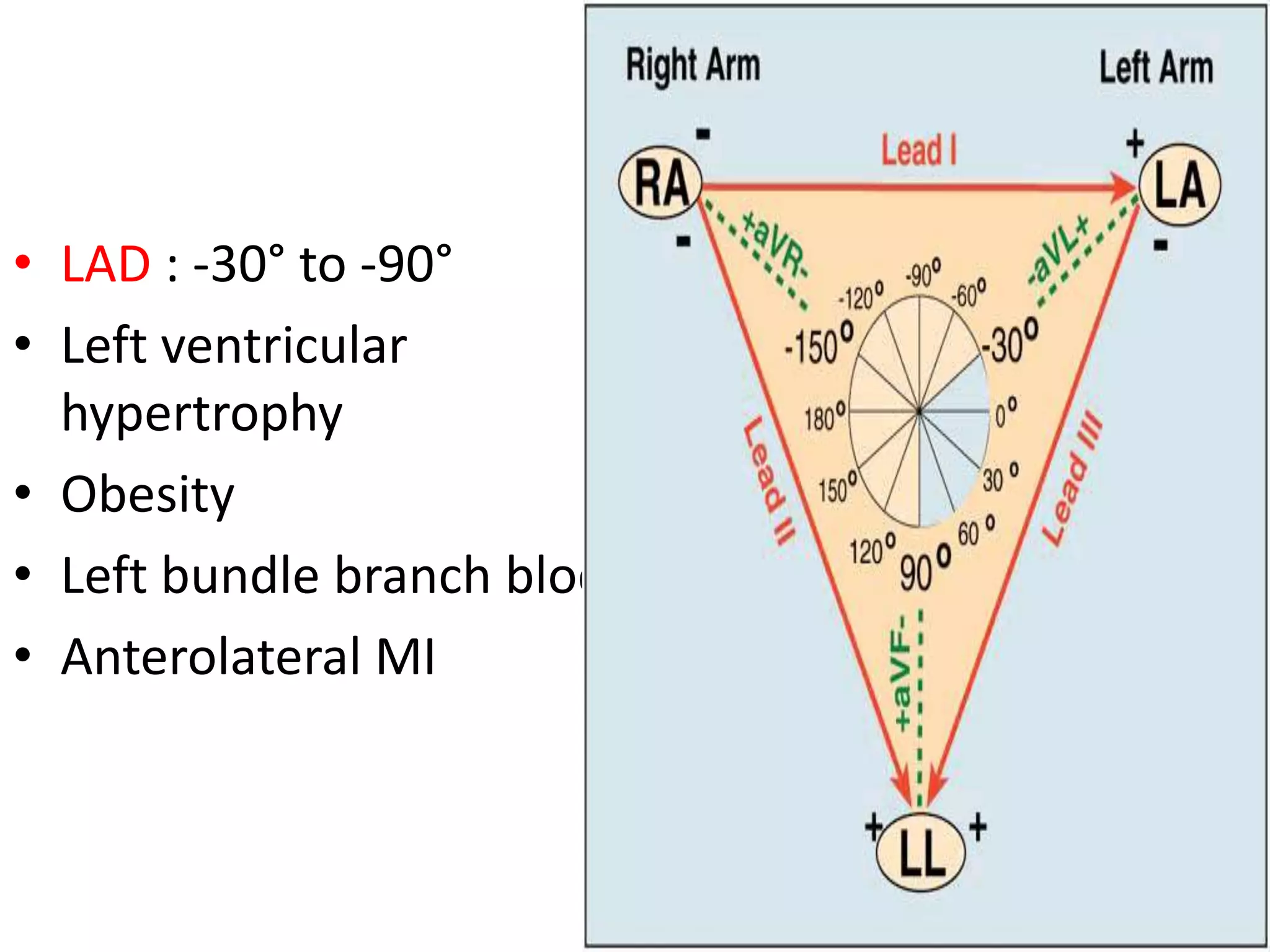
The document discusses cardiac axis and mean QRS axis, which represents the direction of electrical spread during ventricular depolarization. It is measured in the frontal plane based on the limb leads. The lead with the tallest R wave is closest to the axis. The normal range is -30 to +120 degrees with right and left axis deviations indicating abnormalities. Common causes of axis changes are also listed.