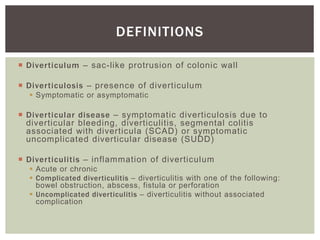
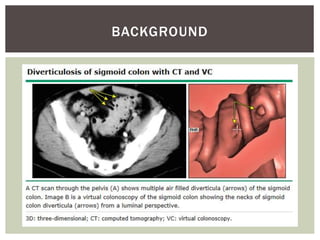
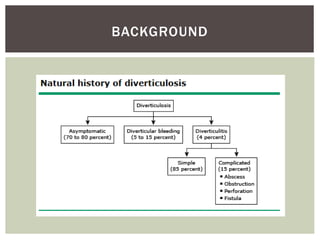
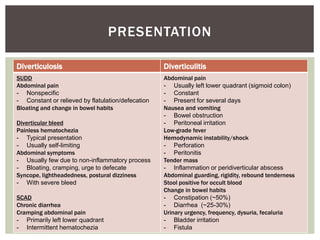
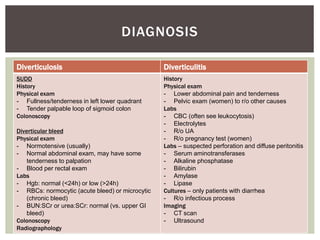
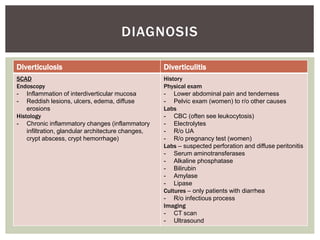
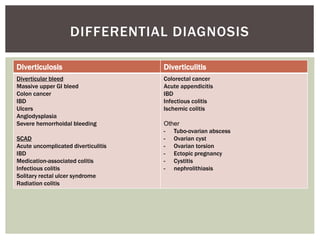
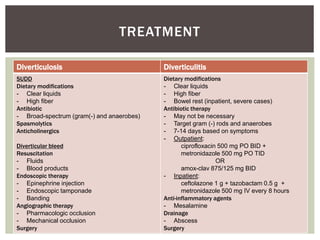
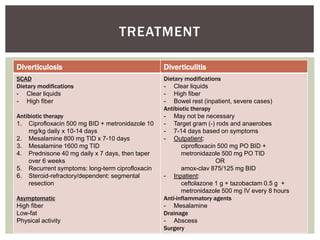
This document defines and discusses diverticulosis, diverticulitis, segmental colitis associated with diverticula (SCAD), and symptomatic uncomplicated diverticular disease (SUDD). It covers the background, definitions, presentations, diagnoses, differential diagnoses, and treatments of these conditions. Diverticulosis is the presence of diverticula (sac-like protrusions of the colonic wall), while diverticulitis is inflammation of the diverticula that can be acute or chronic. SCAD involves chronic inflammation between diverticula, and SUDD includes abdominal pain associated with diverticulosis.