1. Cesarean section is a surgical procedure to deliver fetuses after 28 weeks through an incision in the abdominal and uterine walls. The rate has been steadily rising due to increased safety and availability of blood transfusions and antibiotics.
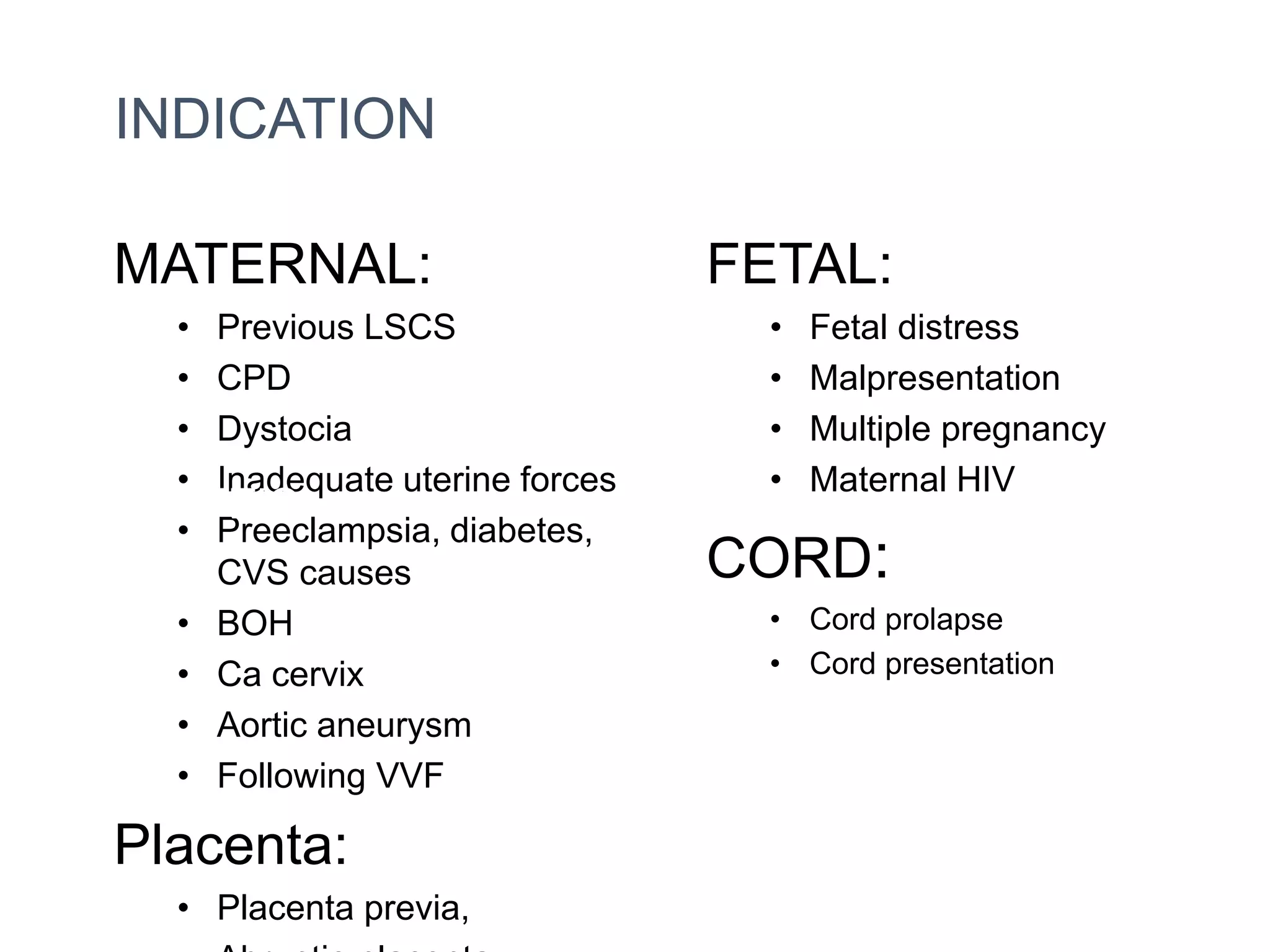
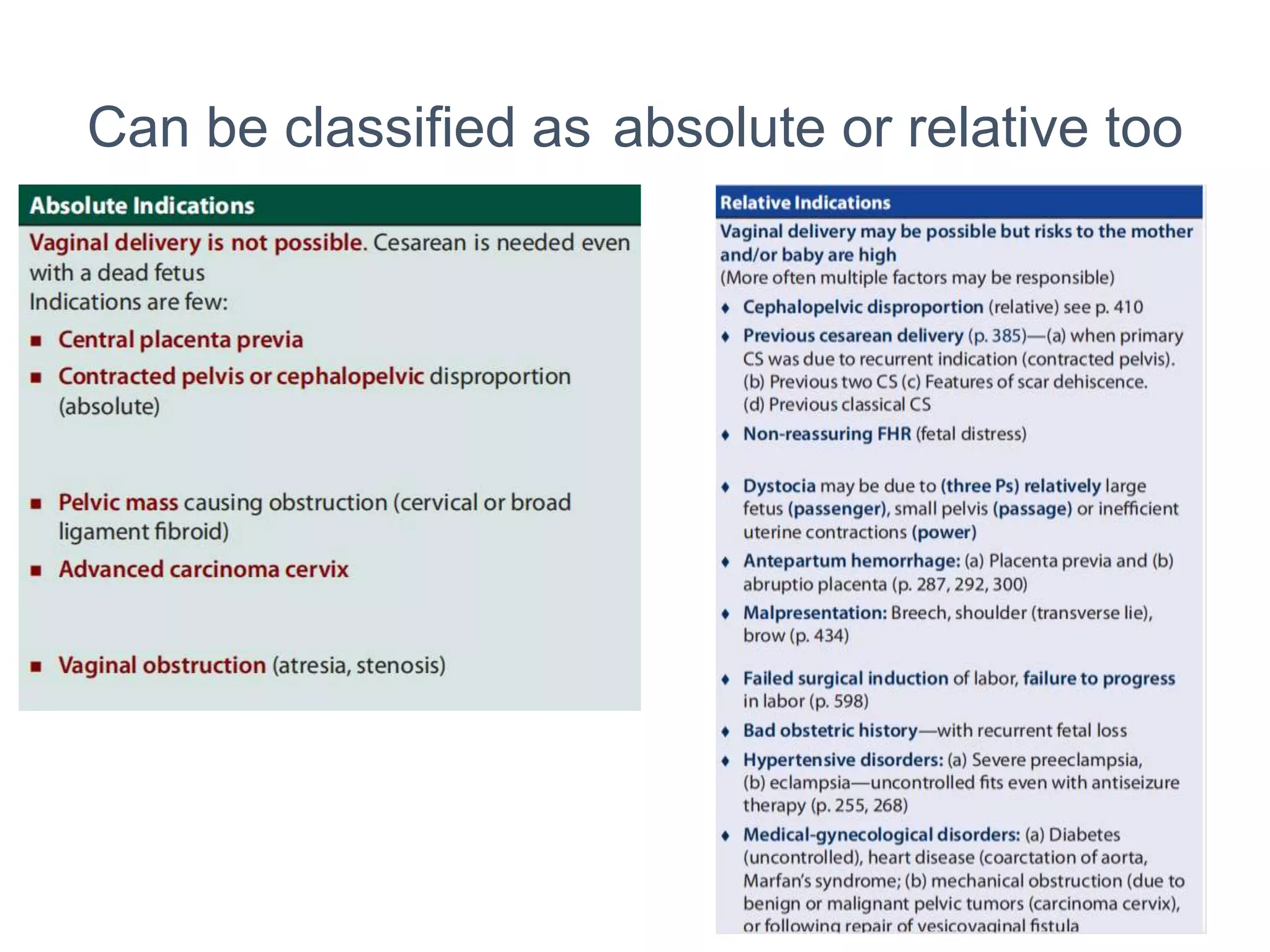
2. Indications include both maternal and fetal factors like previous cesarean, fetal distress, malpresentation, and maternal conditions like preeclampsia. Timing can be elective or emergency.
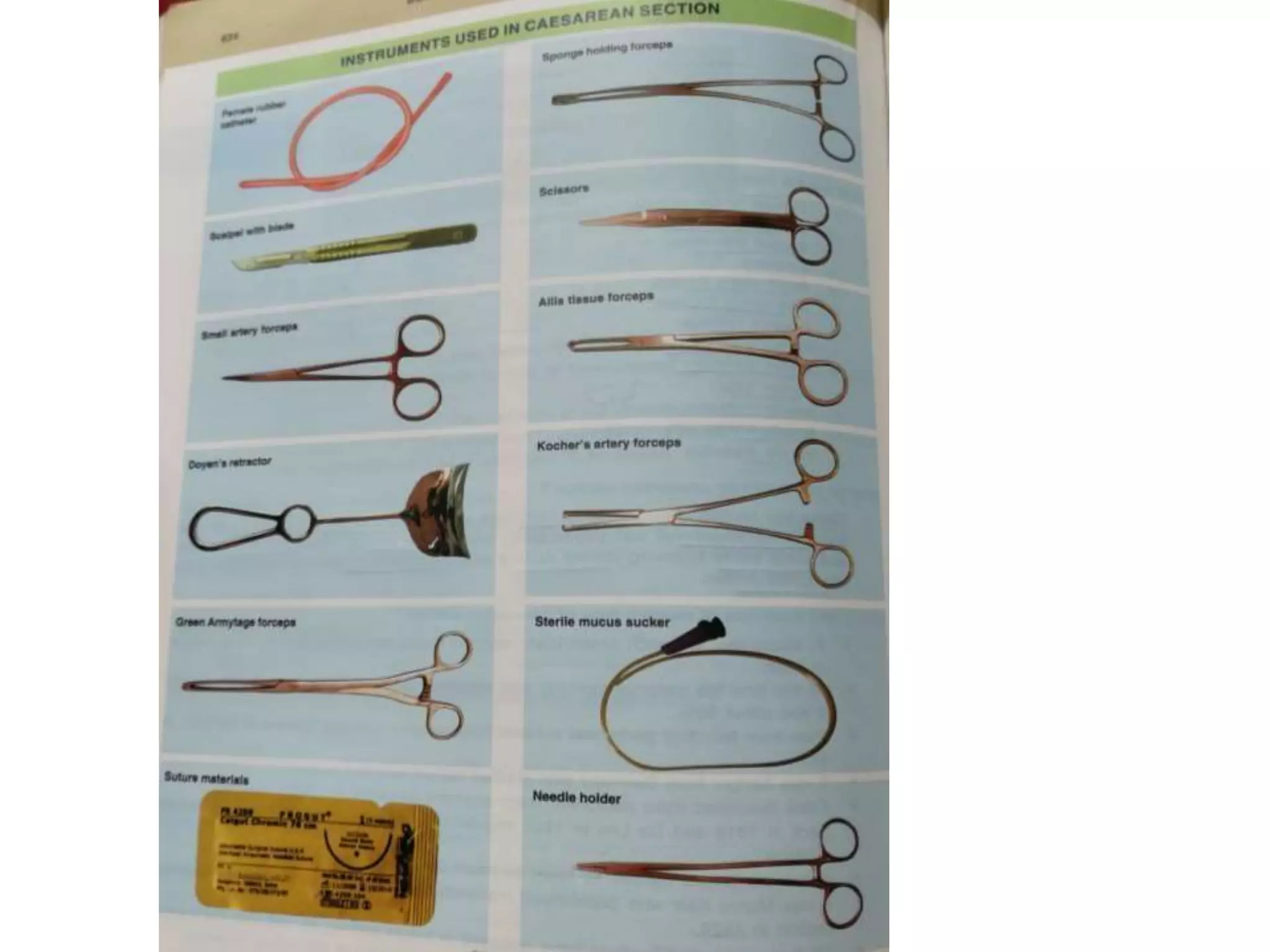
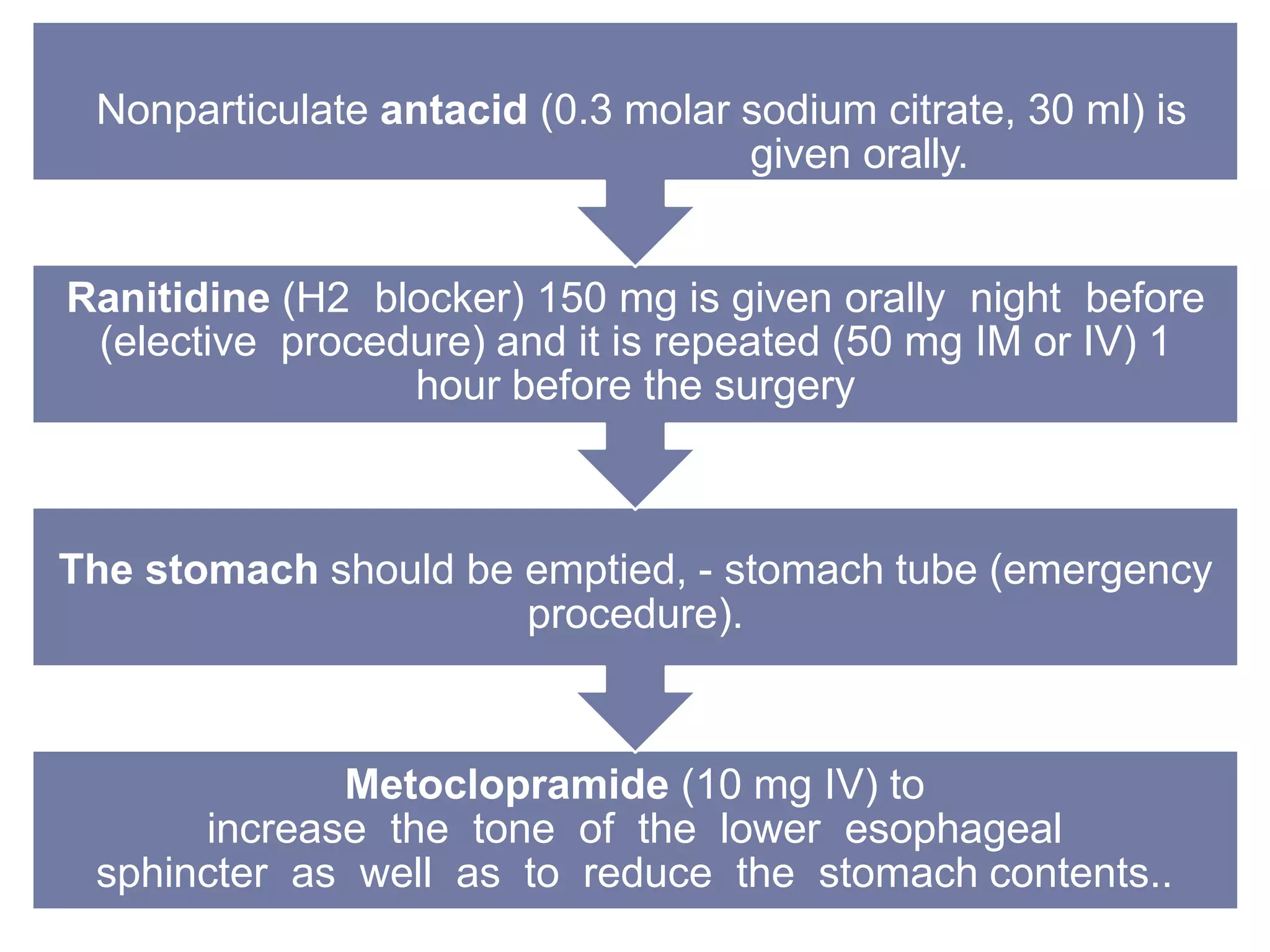
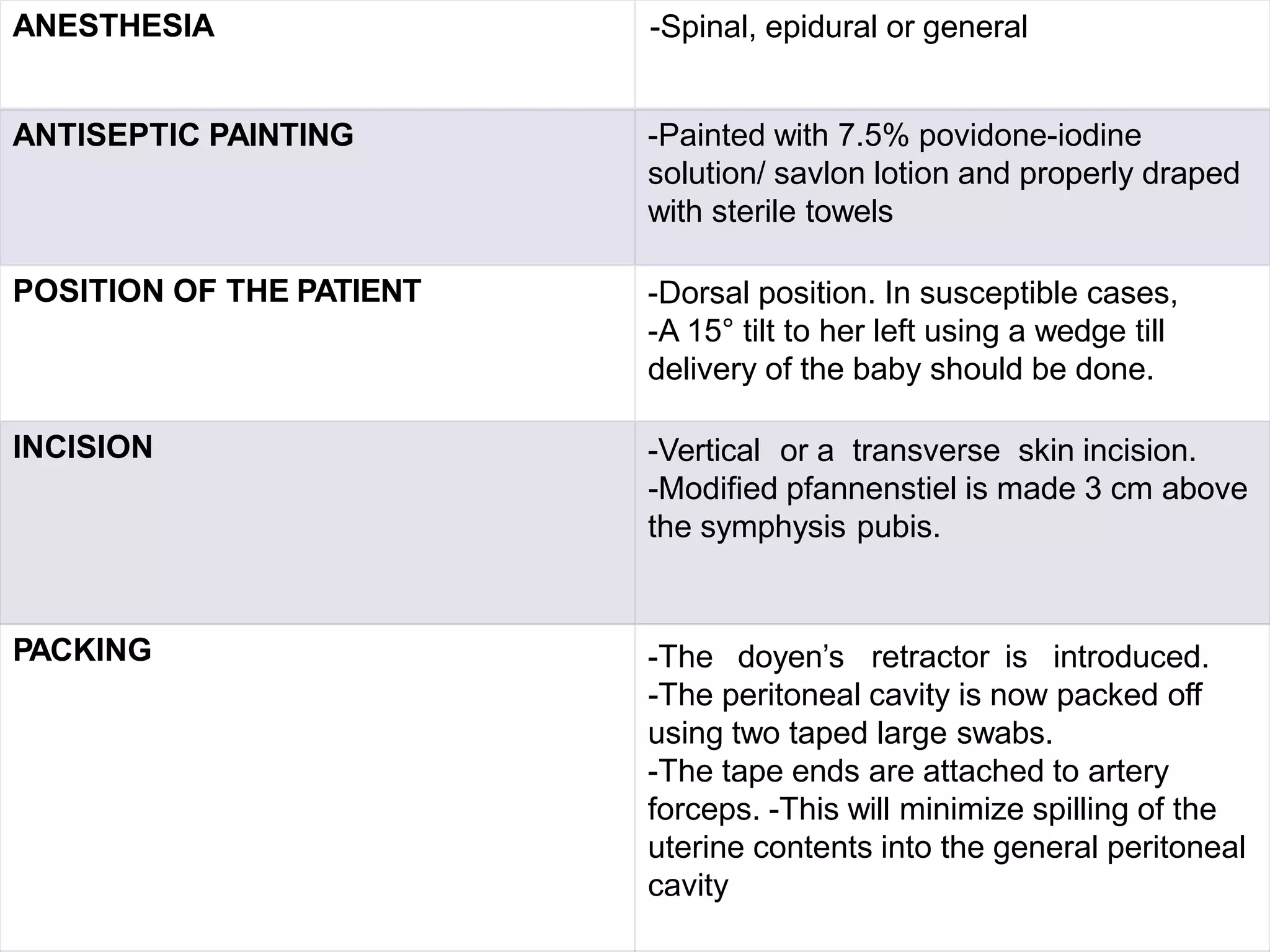
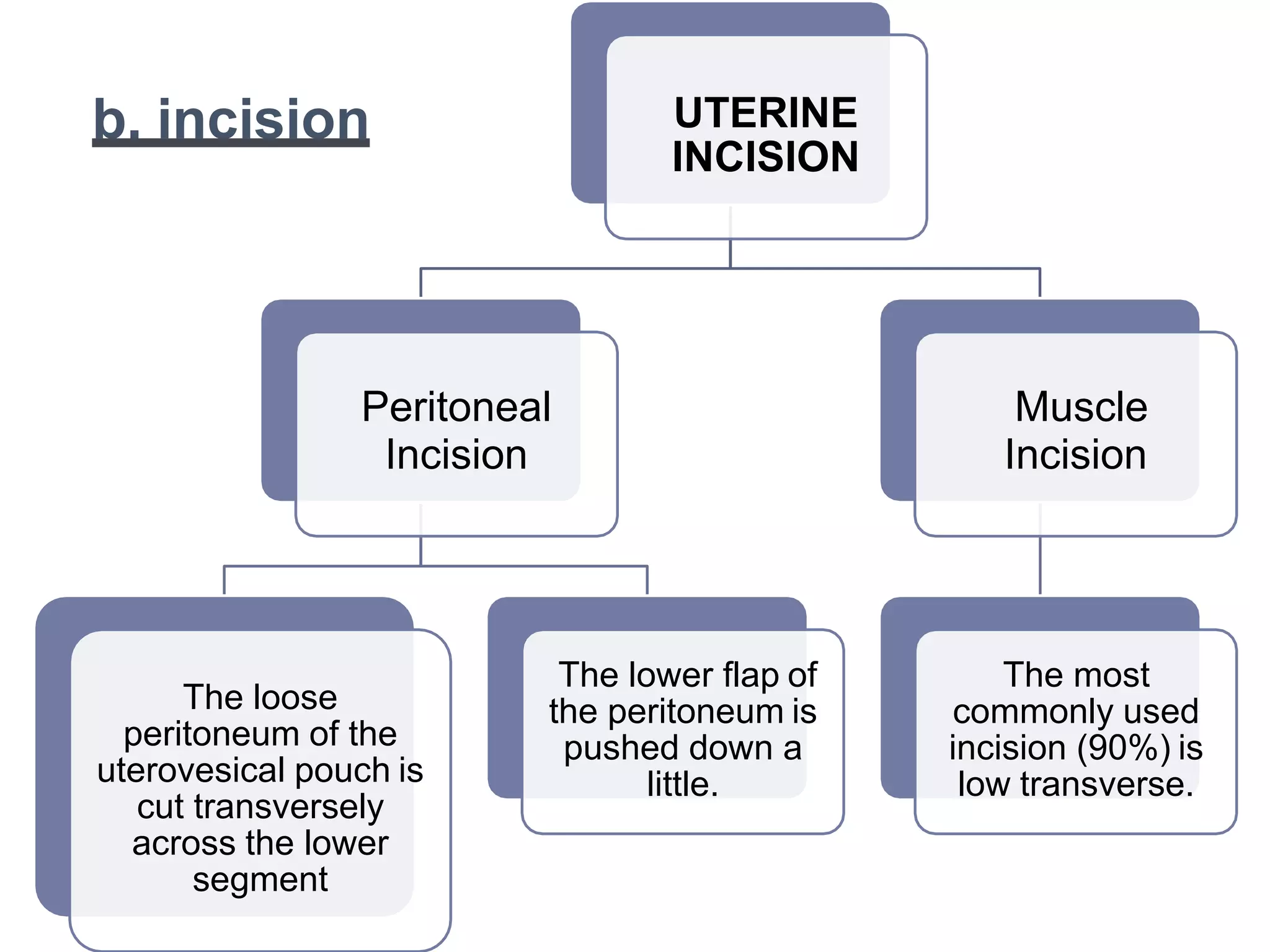
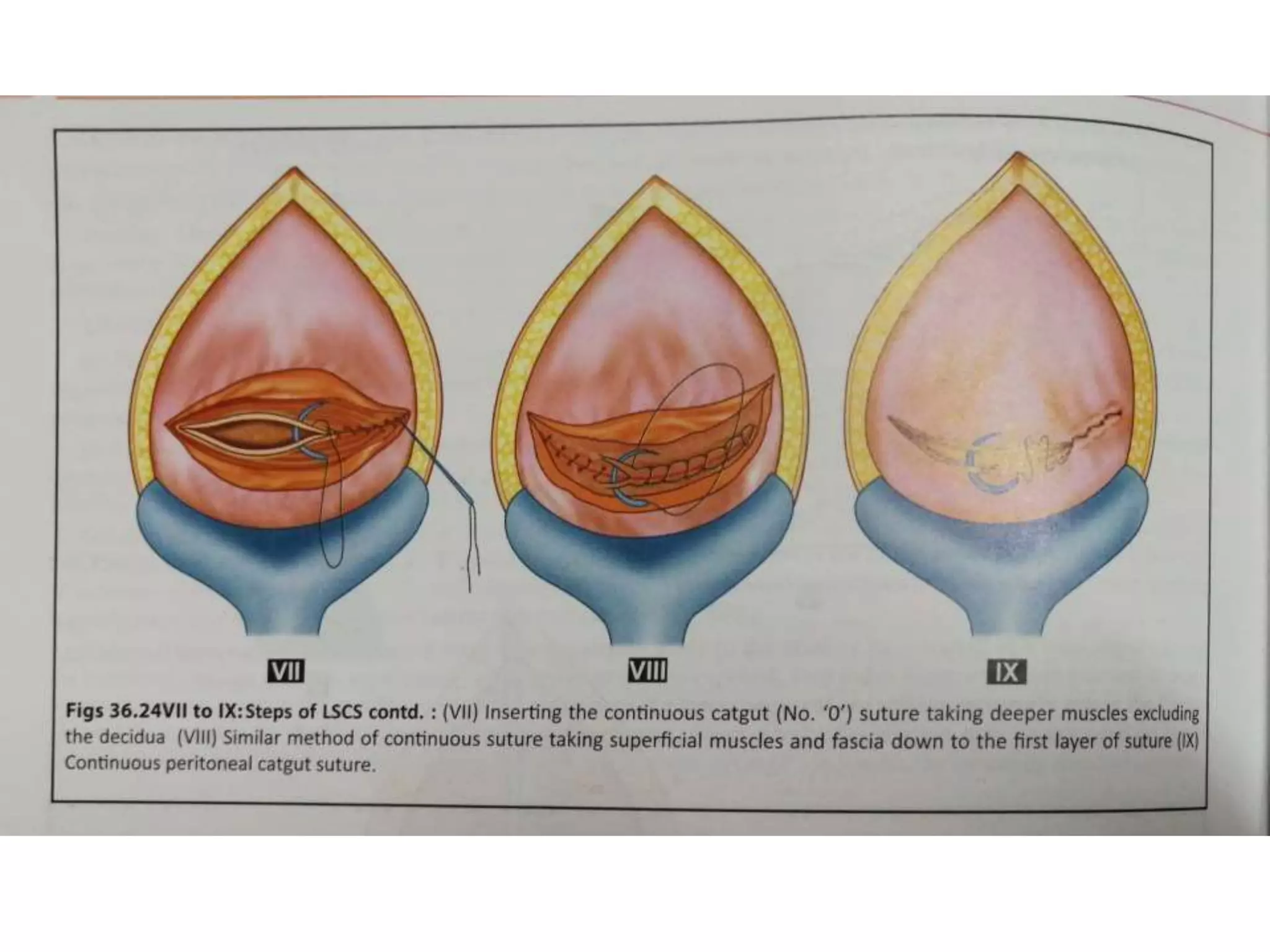
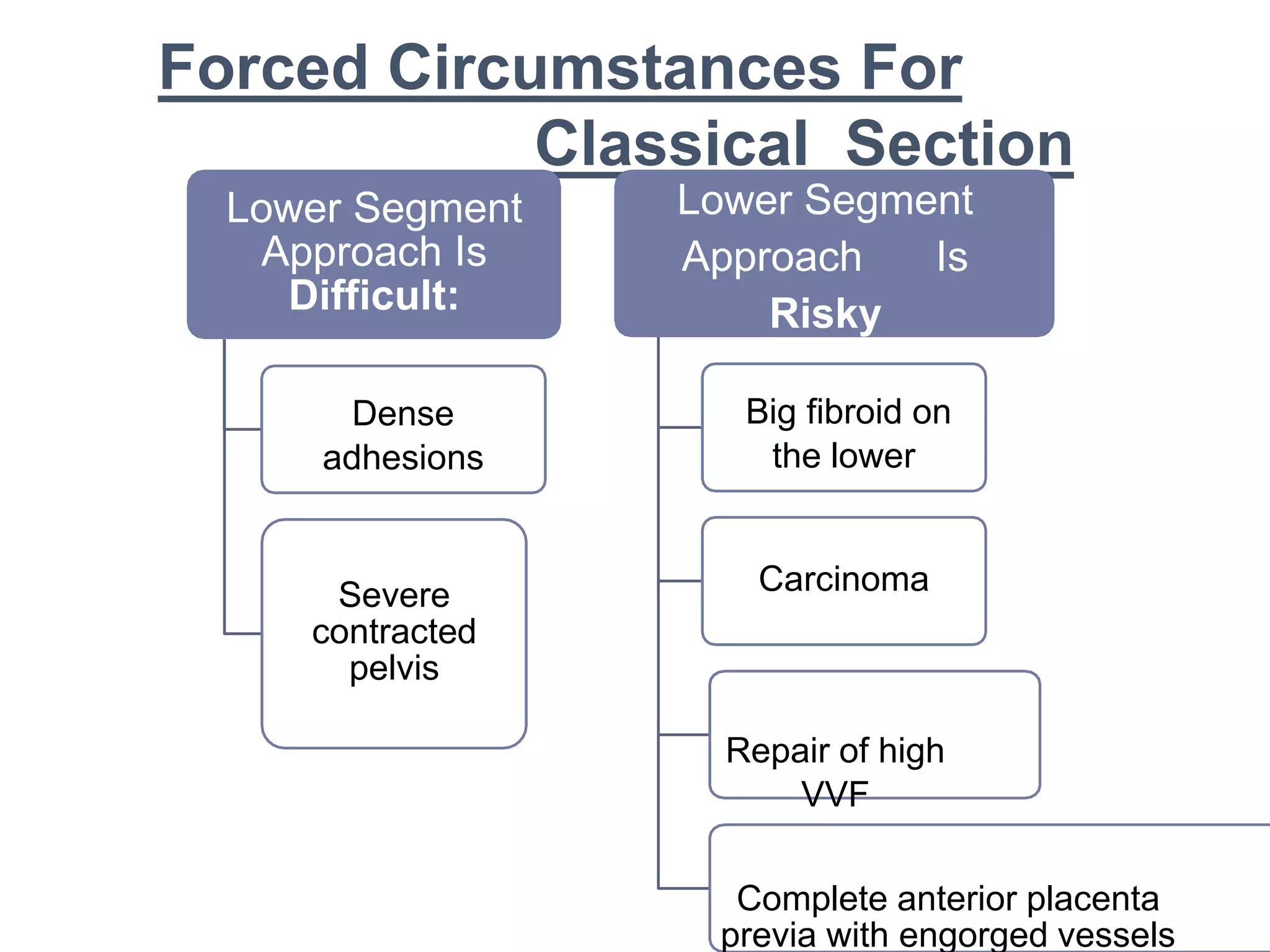
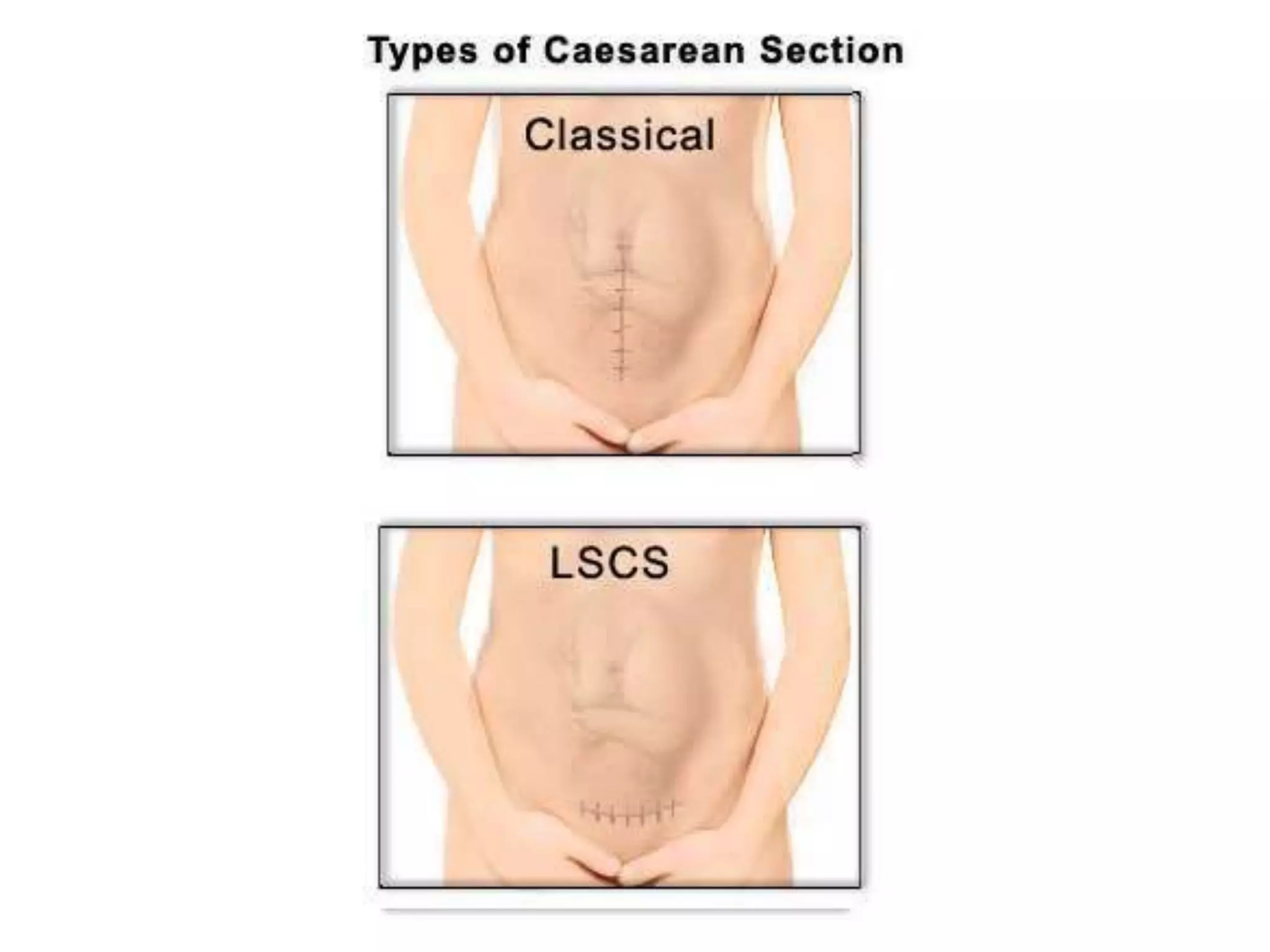
3. The standard procedure involves perioperative preparation, a low transverse incision, delivery of the head and body, removal of the placenta, suturing the incision, and postoperative care including fluids, antibiotics, and ambulation.