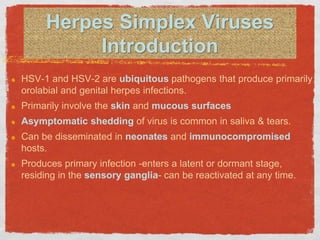
HSV-1 and HSV-2 are ubiquitous viruses that cause infections through direct contact with infected secretions. They establish latency in sensory ganglia after primary infection and can reactivate, causing lesions. Clinical presentations depend on the virus type and location of infection. Common manifestations include orolabial lesions from HSV-1 and genital lesions from HSV-2, as well as infections at other sites in immunosuppressed individuals or through direct contact during activities like wrestling.