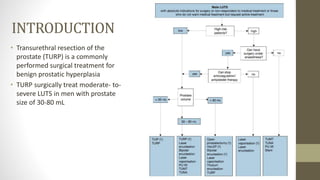
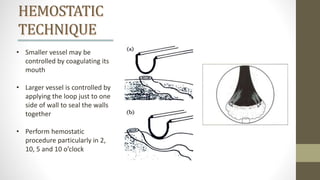
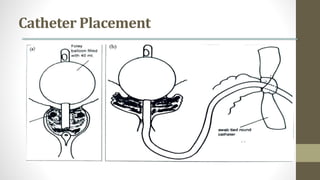
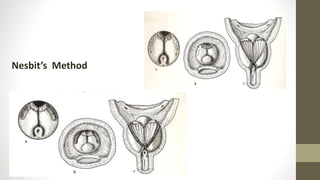
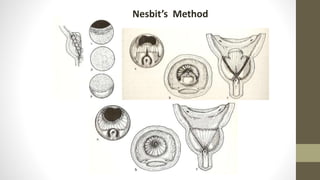
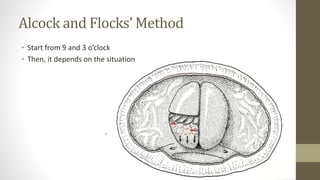
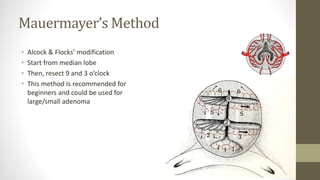
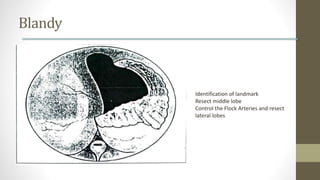
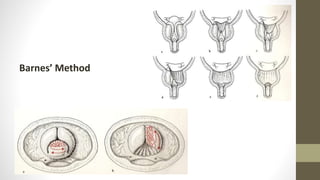
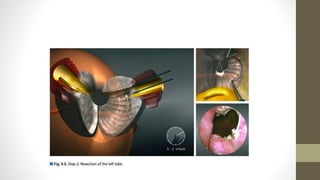
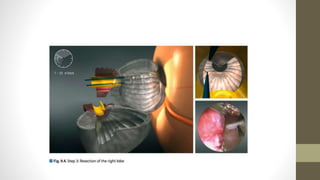
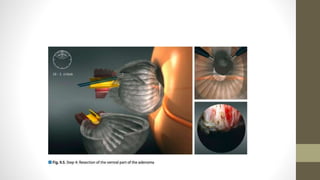
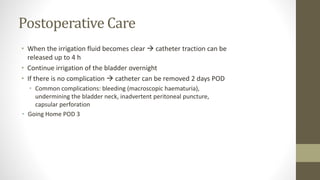
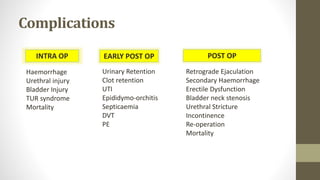
The document provides a detailed overview of the transurethral resection of the prostate (TURP) procedure, including indications, contraindications, techniques, and postoperative care. It outlines both absolute and relative indications for surgery, various surgical methods, and specific steps in the TURP technique to ensure safety and efficacy. Additionally, it addresses potential complications and postoperative management guidelines.