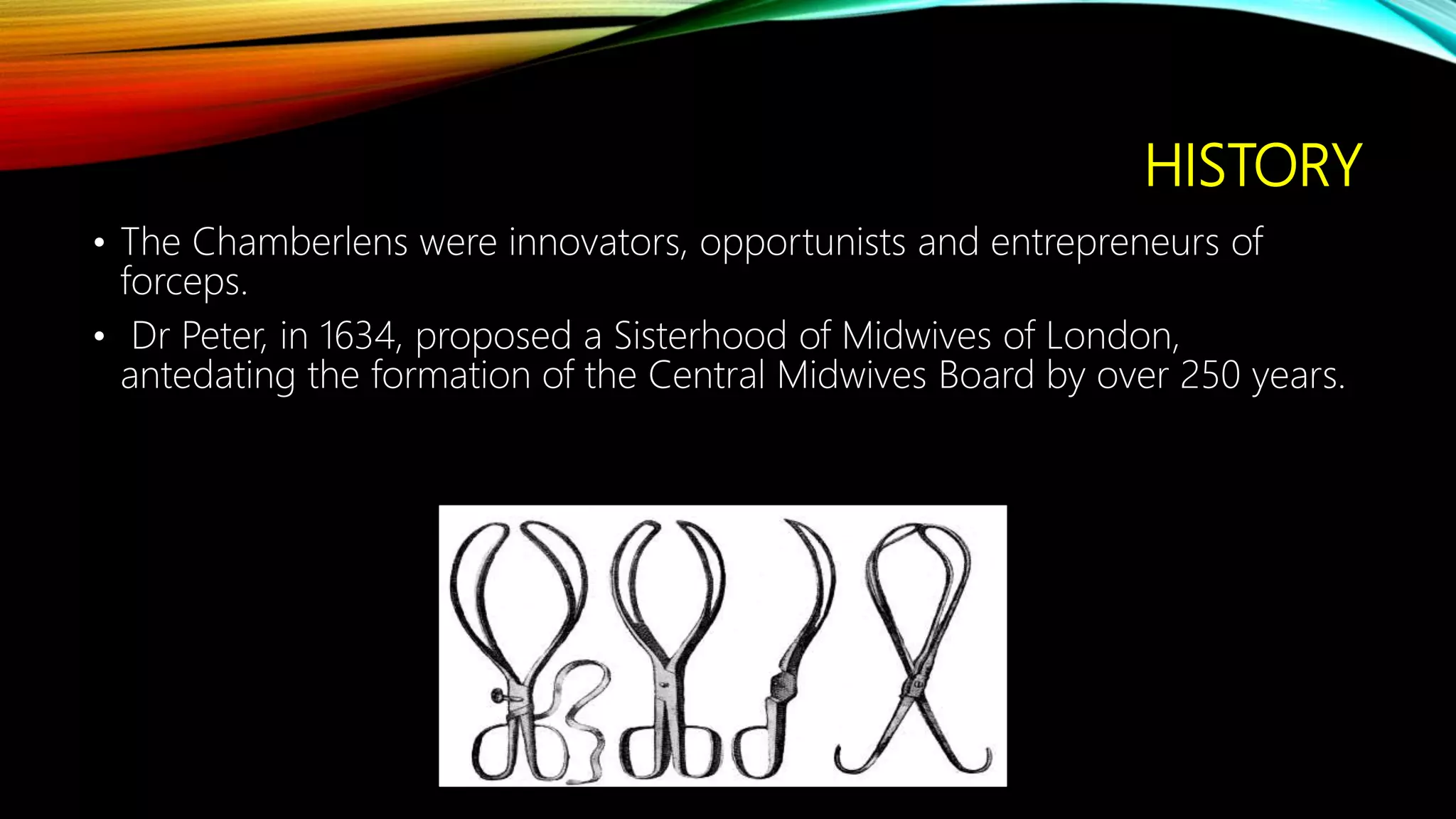
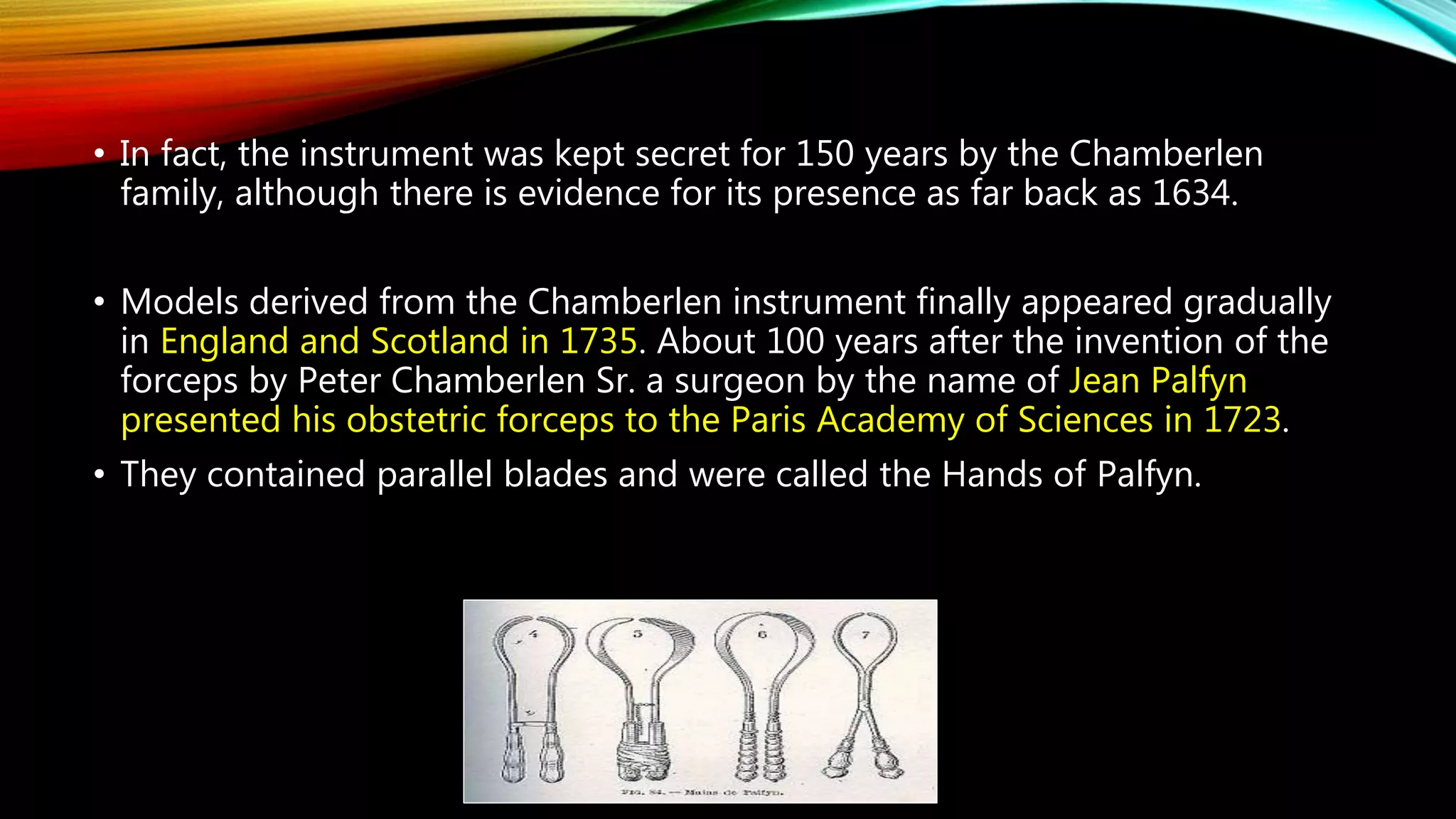
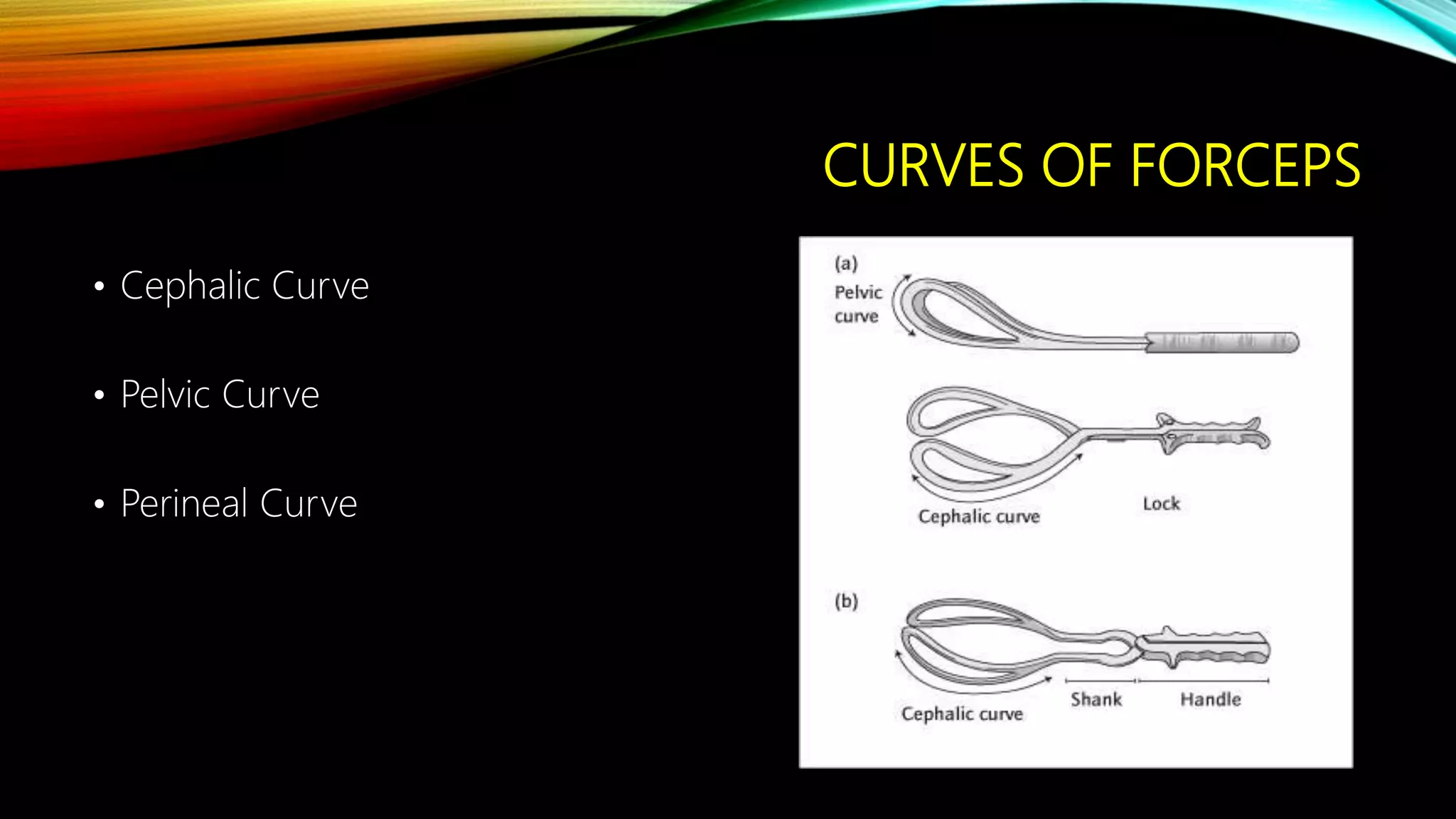
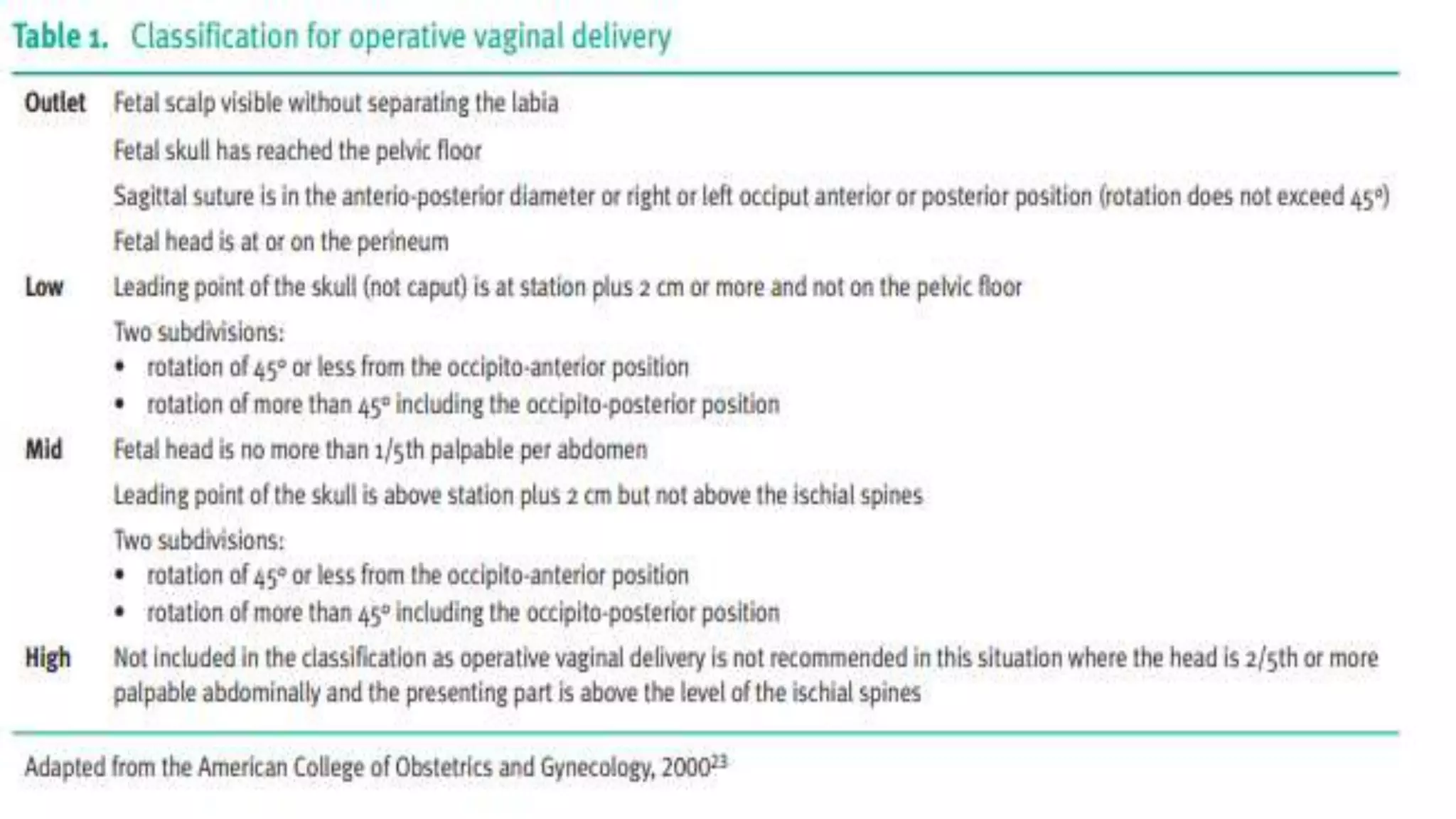
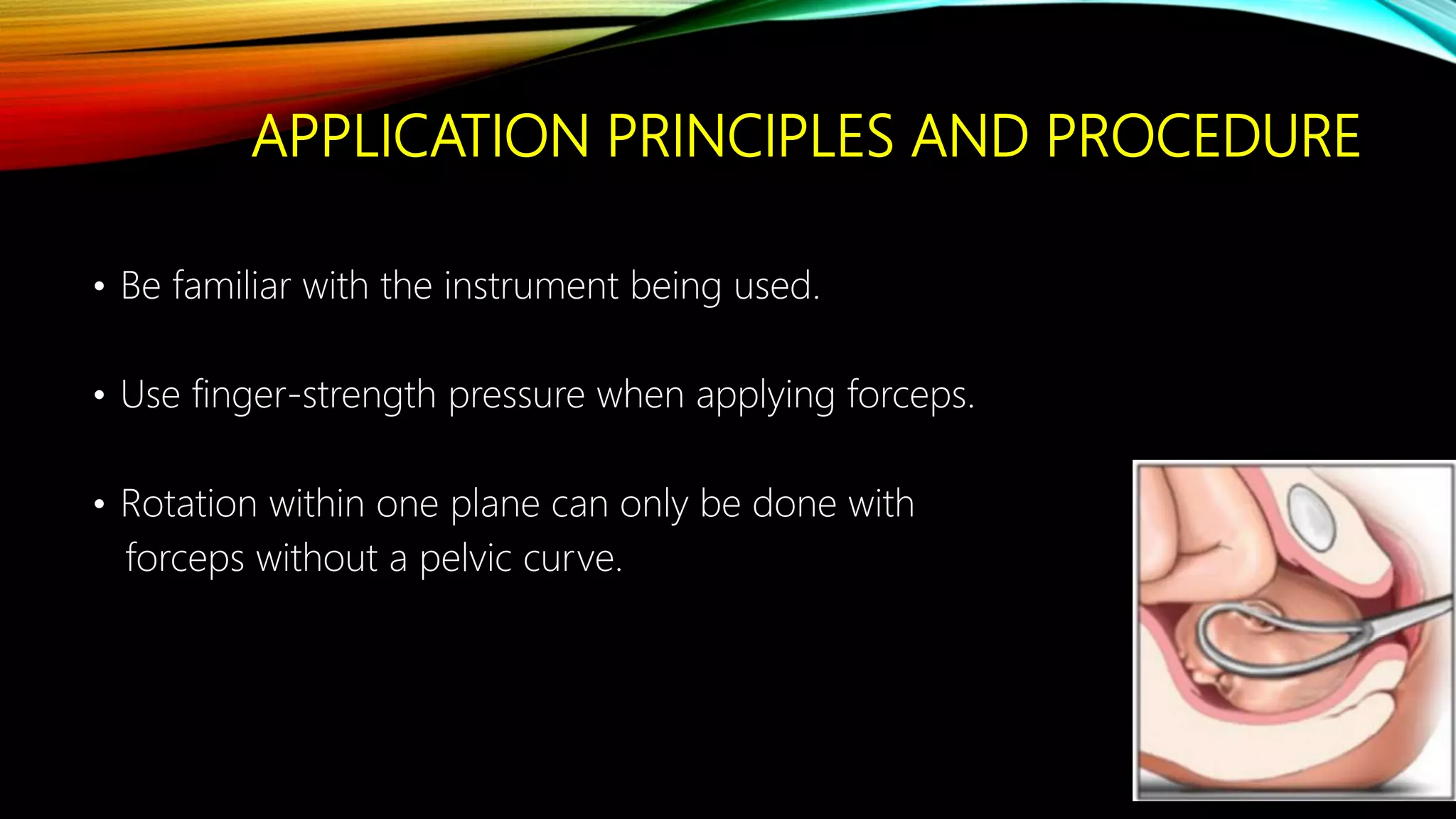
The document provides a detailed history and overview of forcep delivery, tracing its origins from the Chamberlen family and the development of various forceps types and techniques. It outlines prerequisites, contraindications, application principles, and potential complications for both mothers and infants during forceps-assisted deliveries. The document emphasizes the importance of proper technique and patient selection to minimize the risk of failed operative deliveries and associated complications.