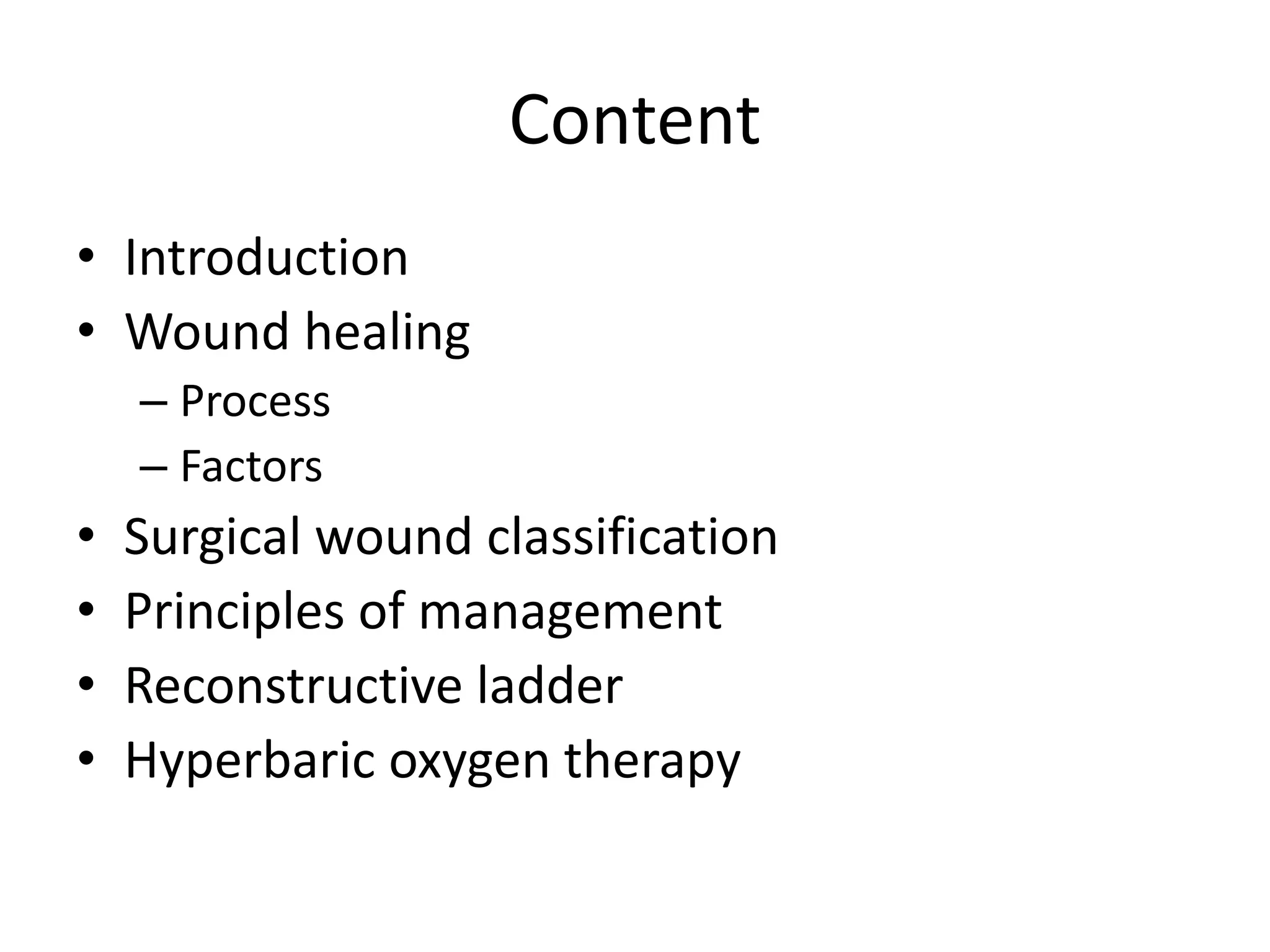
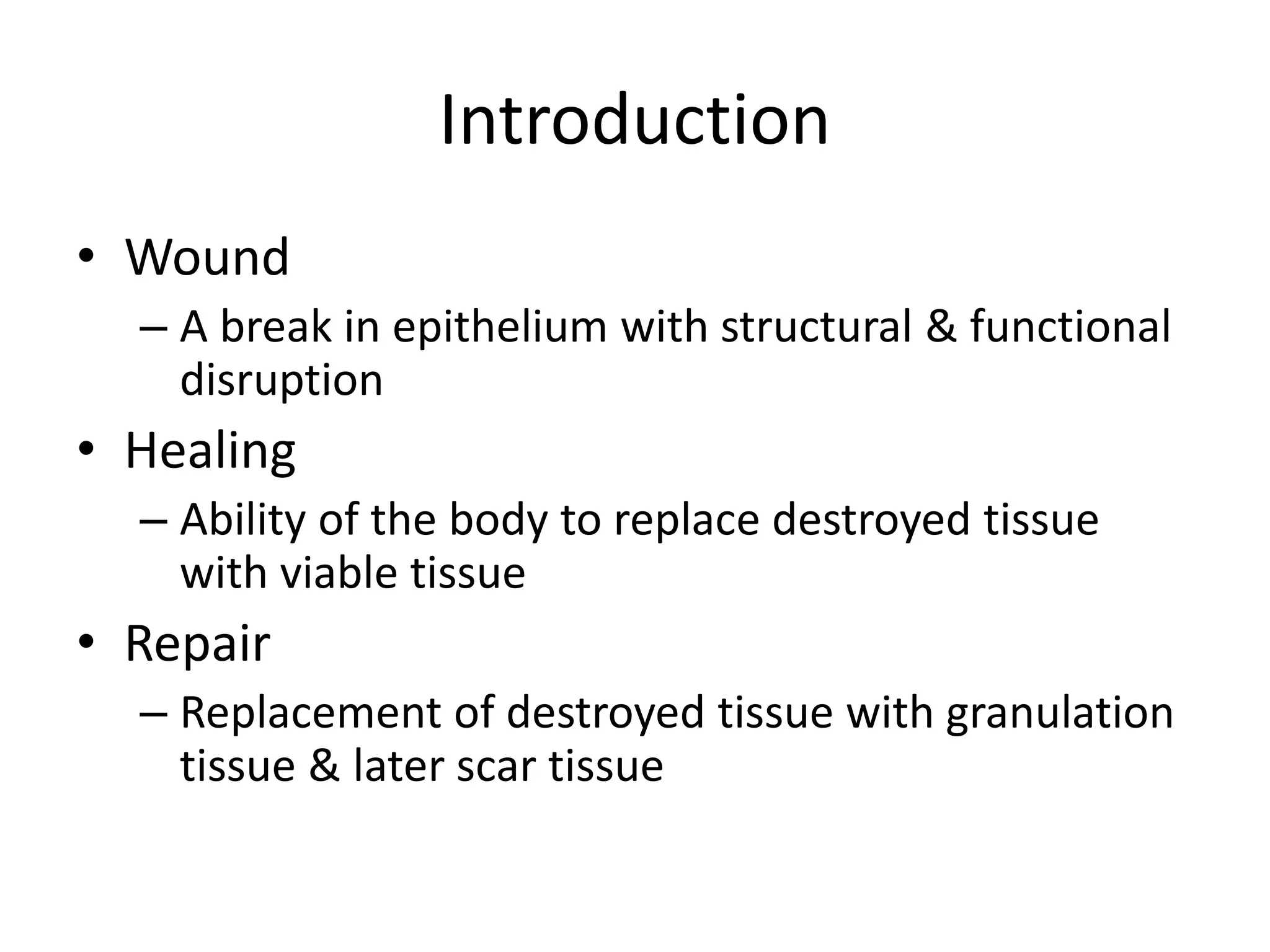
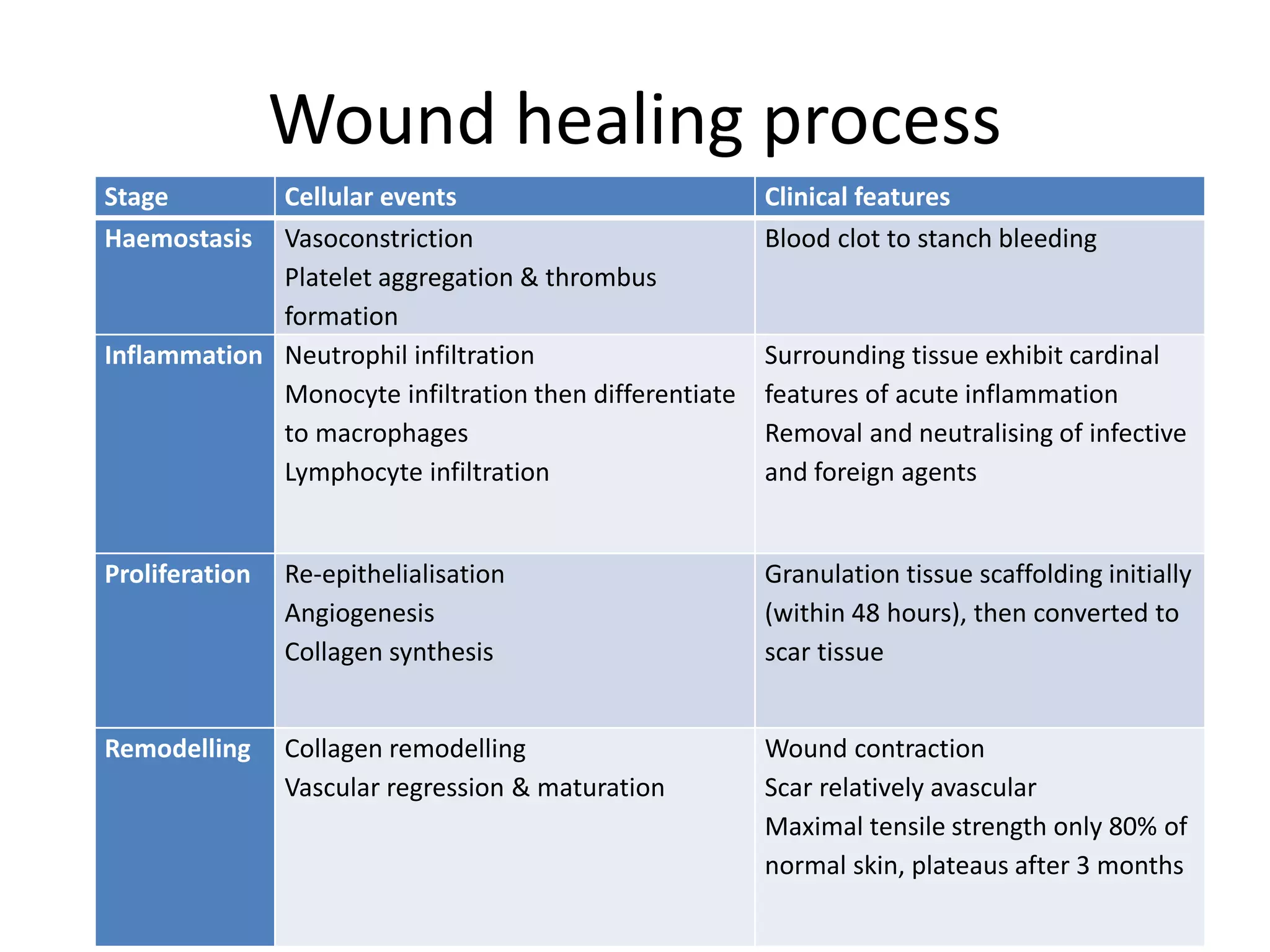
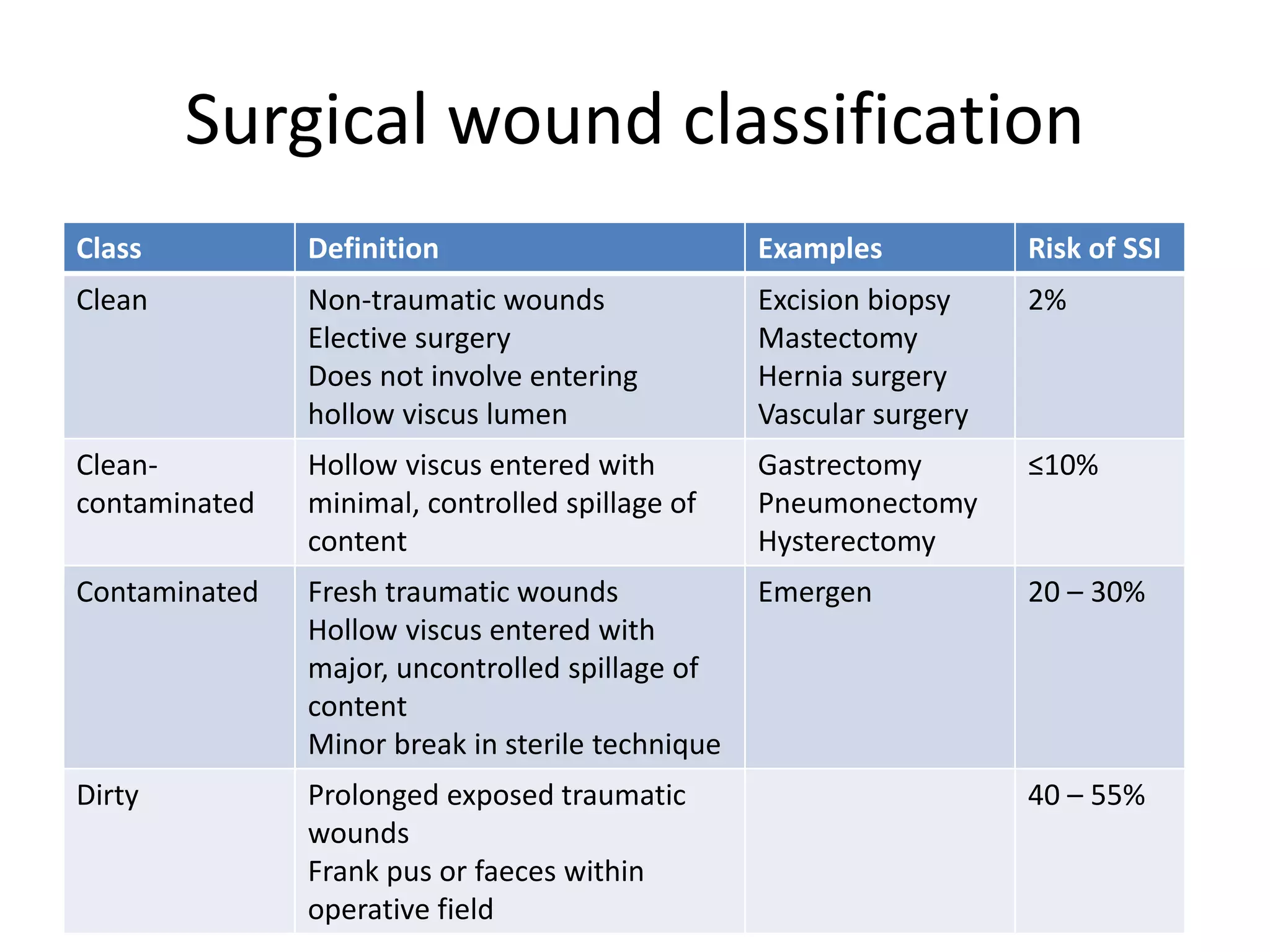
The document provides an overview of wound management, detailing the wound healing process, factors affecting healing, and surgical wound classifications. It discusses principles of management, including surgical techniques, dressings, and hyperbaric oxygen therapy as an adjunct treatment. Additionally, it introduces the reconstructive ladder, describing various methods of tissue transfer and closure options.