This document provides tips and instructions for using a PowerPoint presentation on wound healing. It discusses:
- Freely editing, modifying, and using the slides.
- Many slides are blank except for the title to facilitate active learning sessions where students provide information before each slide is shown.
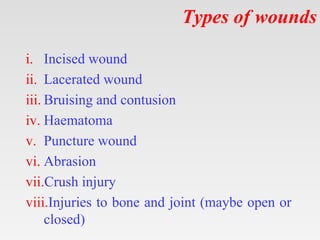
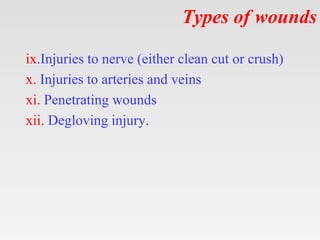
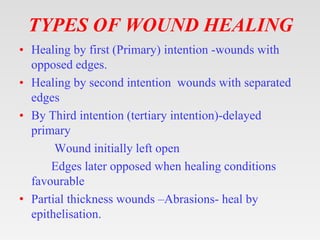
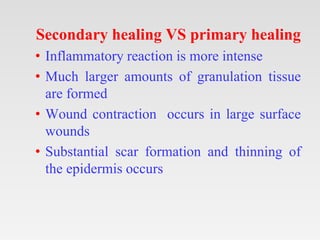
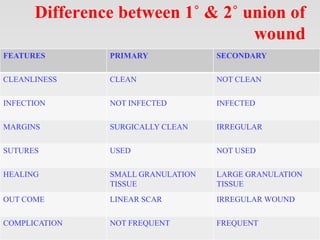
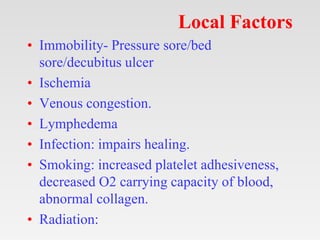
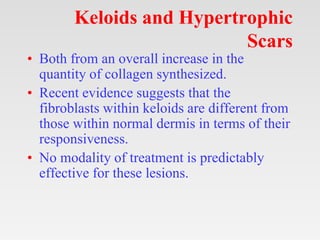
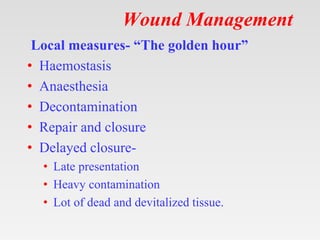
- The presentation covers definitions of wounds, classifications of wounds and surgical wounds, phases of healing, factors affecting healing, and wound management.
- It encourages interactive learning by showing blank slides first to elicit student responses before presenting each topic. This is recommended for both individual study and classroom learning.