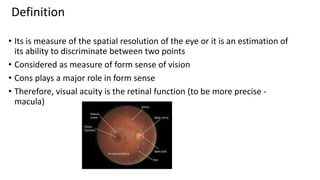
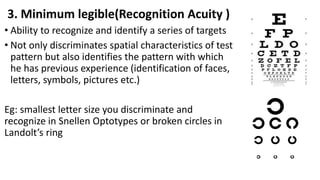
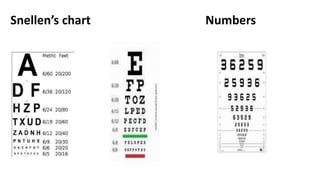
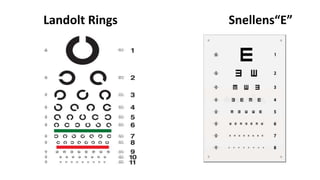
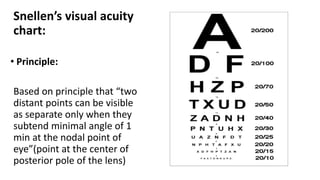
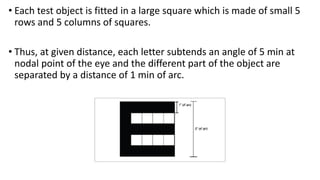
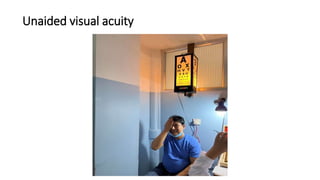
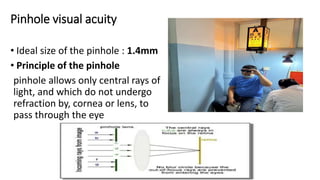
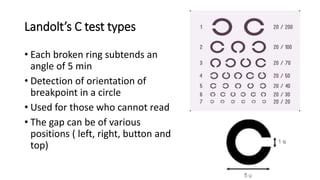
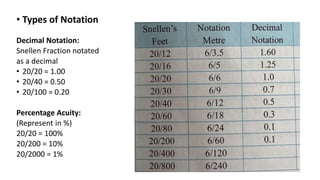
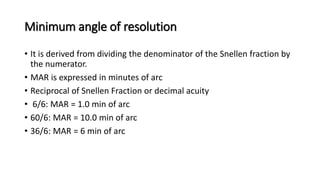
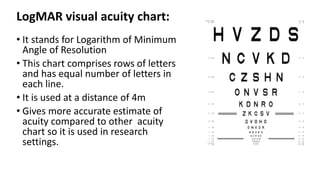
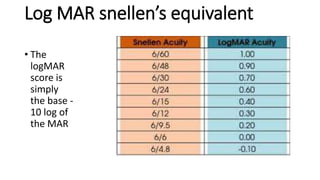
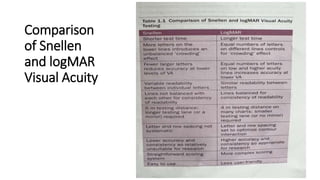
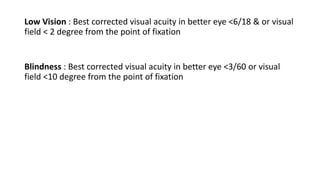
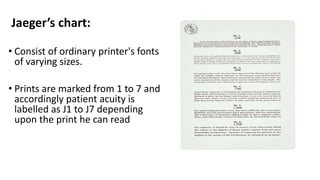
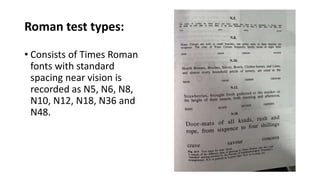
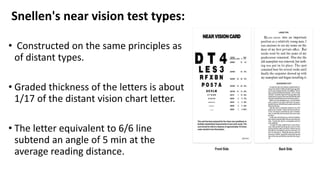
Visual acuity is a measure of the eye's ability to see fine detail and discriminate shapes and patterns. It is dependent on the retina and macula's ability to resolve fine spatial patterns. Visual acuity is measured using optotypes like letters of decreasing size or Landolt rings with gaps in different positions. Distance visual acuity is tested at 6 meters using a Snellen chart while near acuity uses Jaeger or N-charts at 40cm. Factors like stimulus size, contrast and observer related factors impact acuity. Clinical acuity measurements assess unaided, aided and pinhole vision and use notations like decimals, percentages or LogMAR scores.