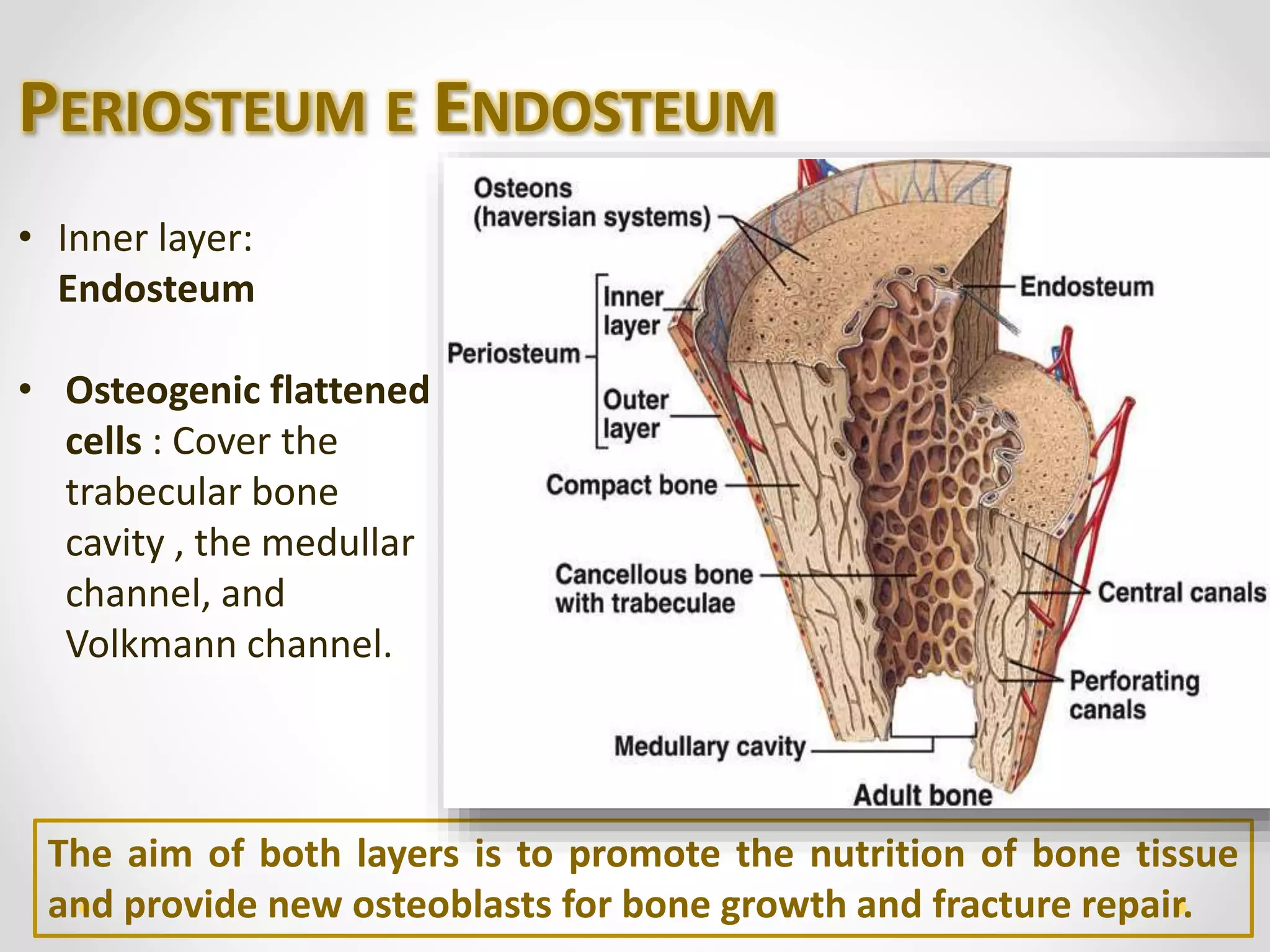
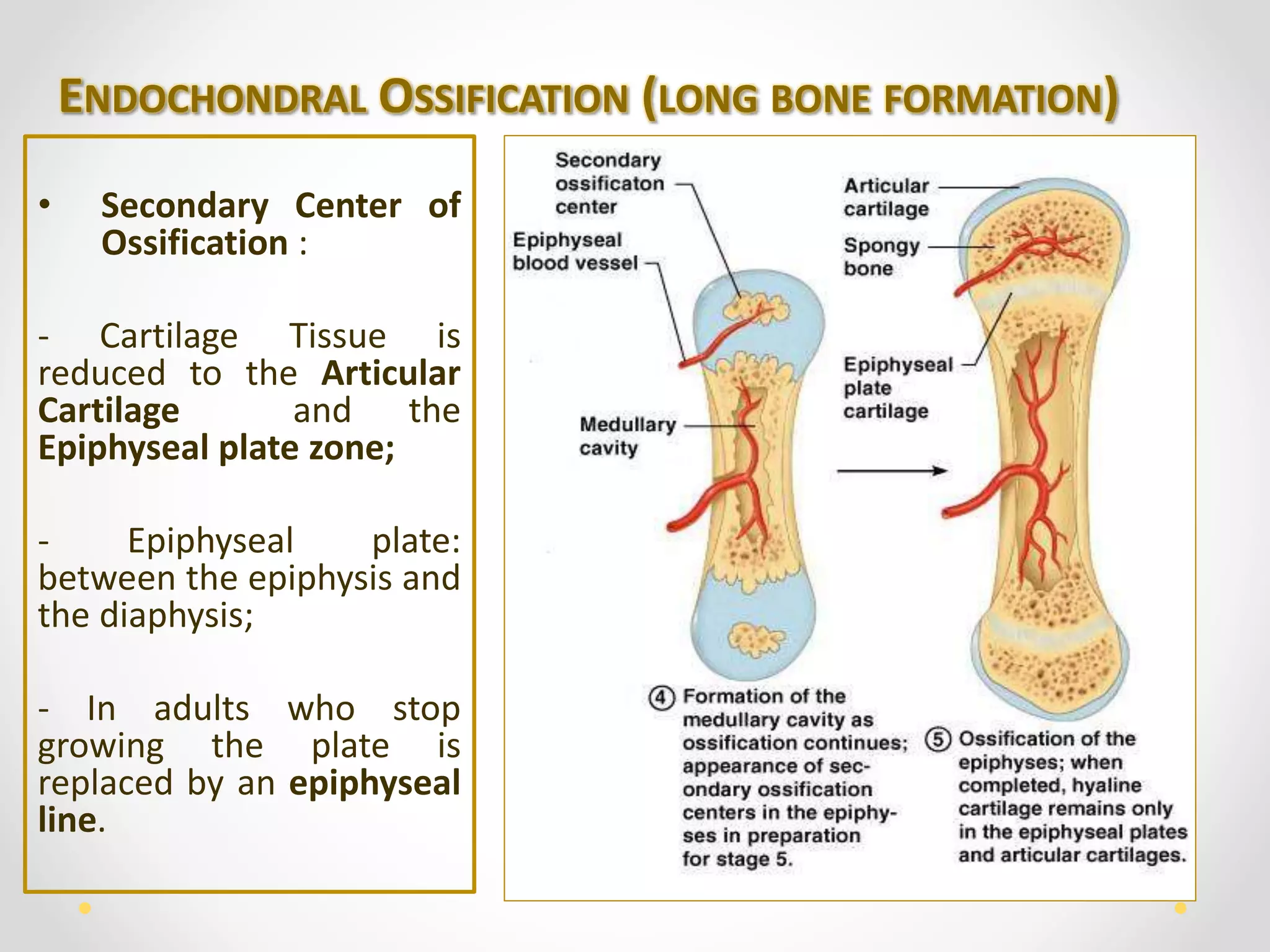
The document details the constitution and functions of human bone tissue, elaborating on the roles of bone cells (osteoblasts, osteocytes, and osteoclasts), and types of bone tissue such as compact and cancellous bone. It includes processes of osteogenesis, both intramembranous and endochondral ossification, as well as the dynamics of bone remodeling and repair. Additionally, it addresses calcium homeostasis and various bone disorders like osteoporosis and rickets.