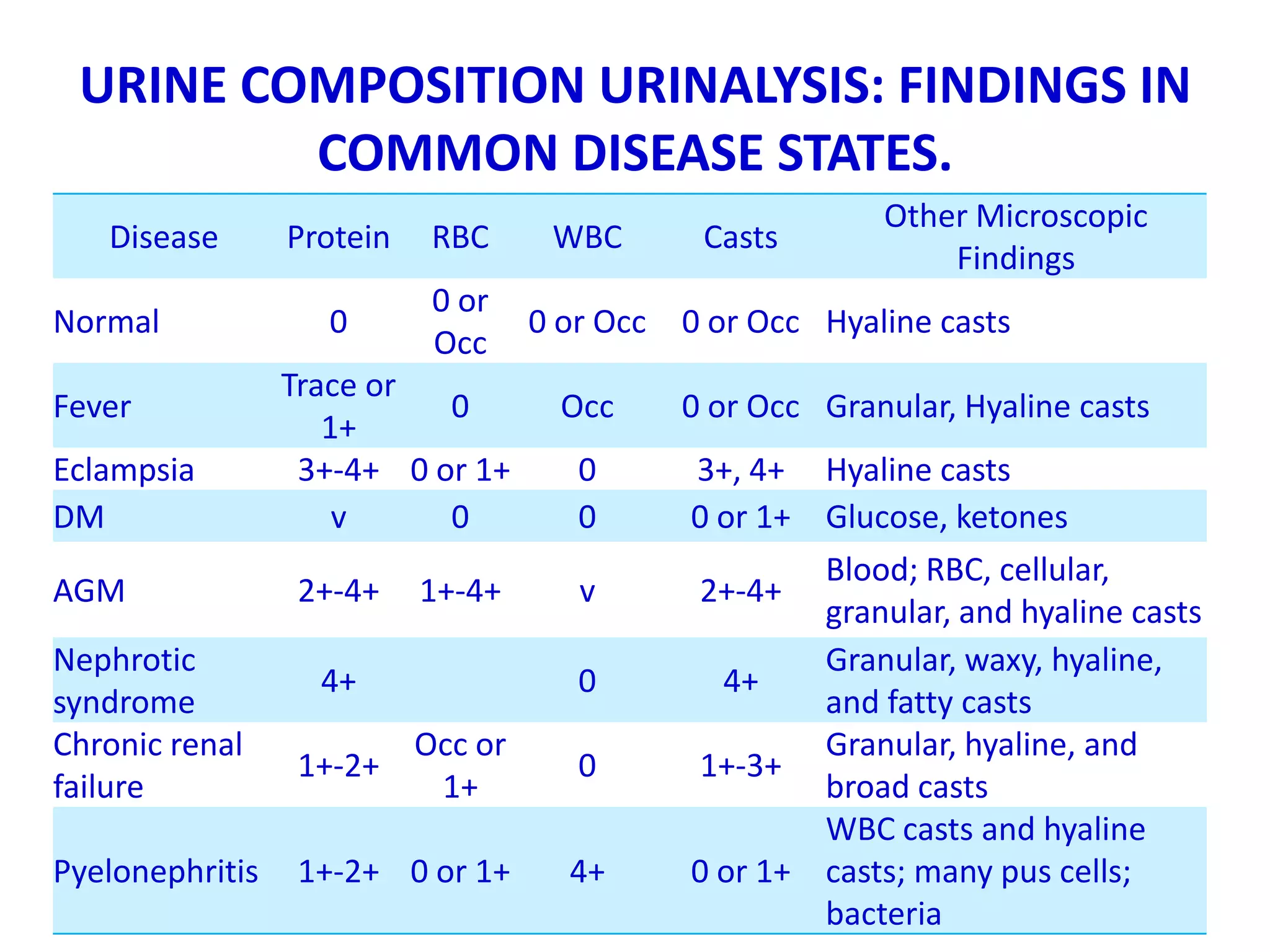
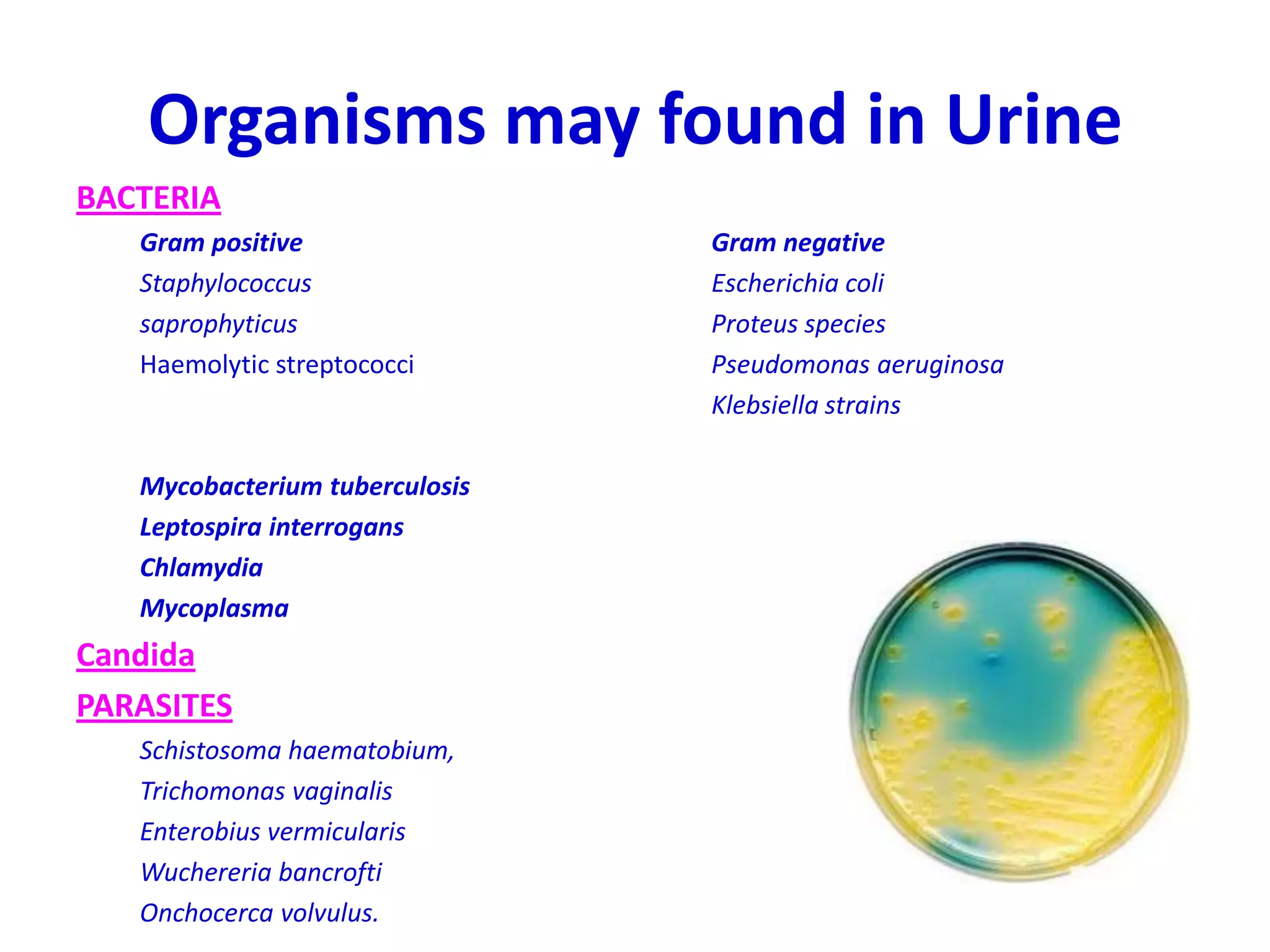
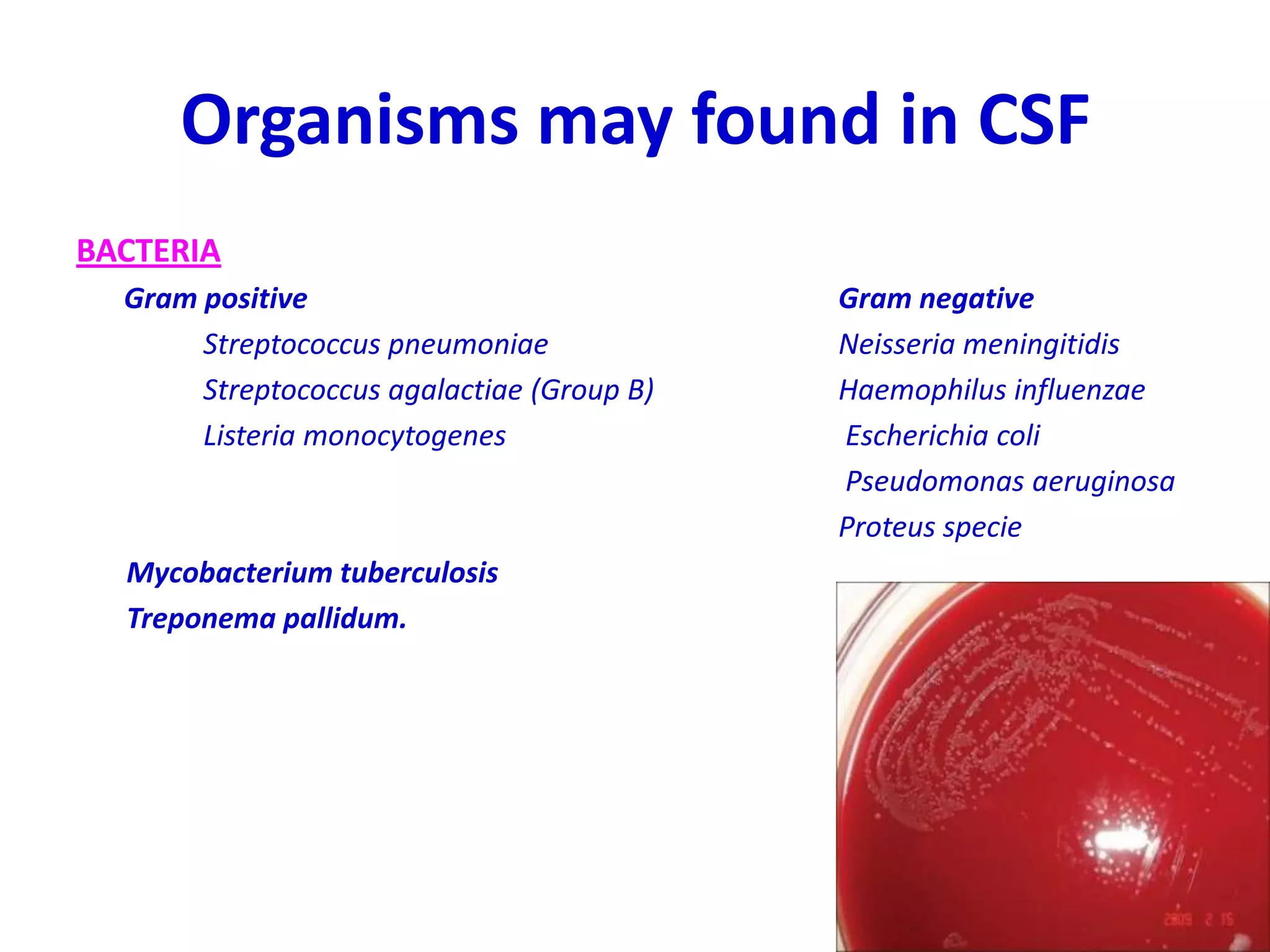
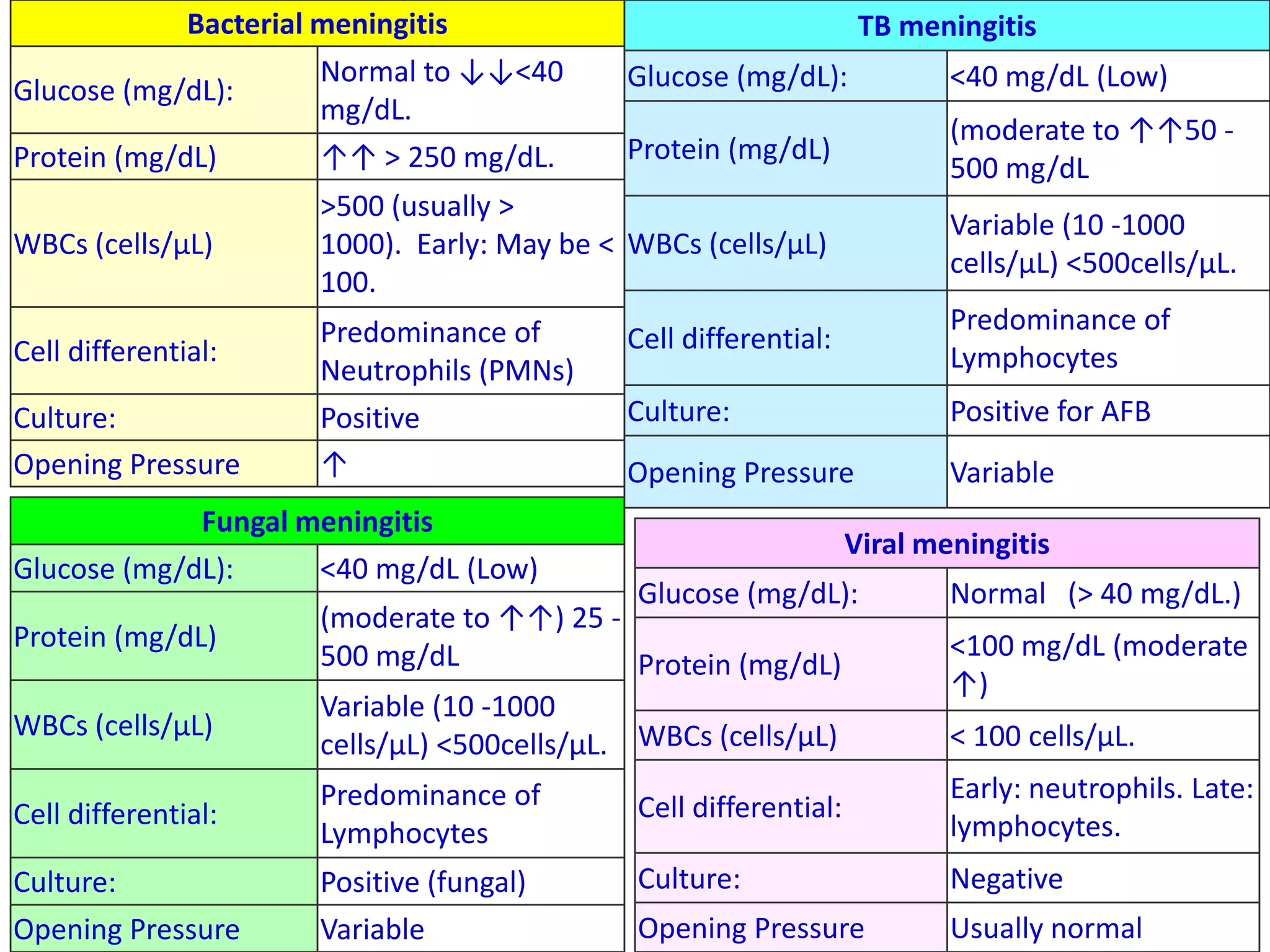
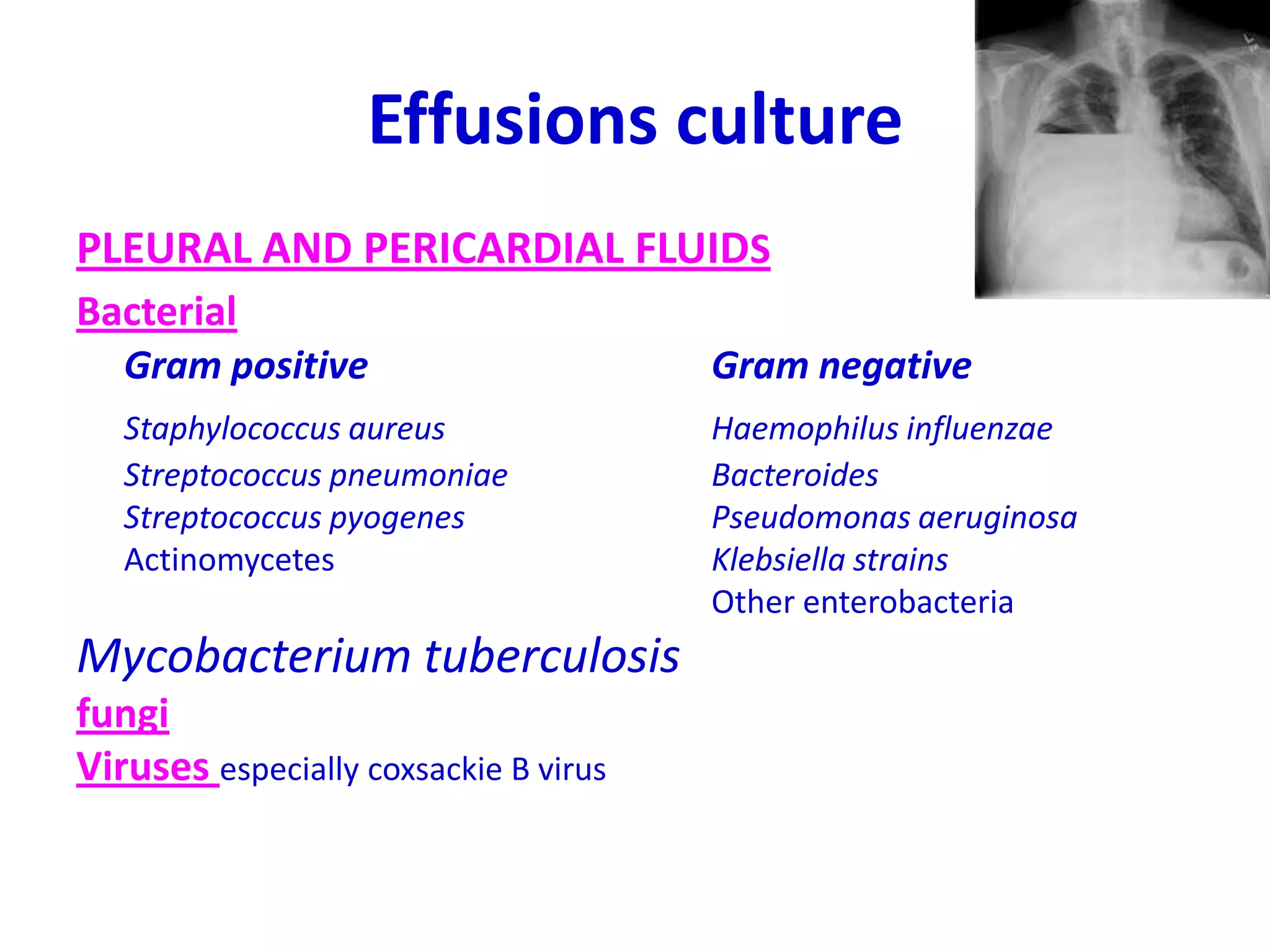
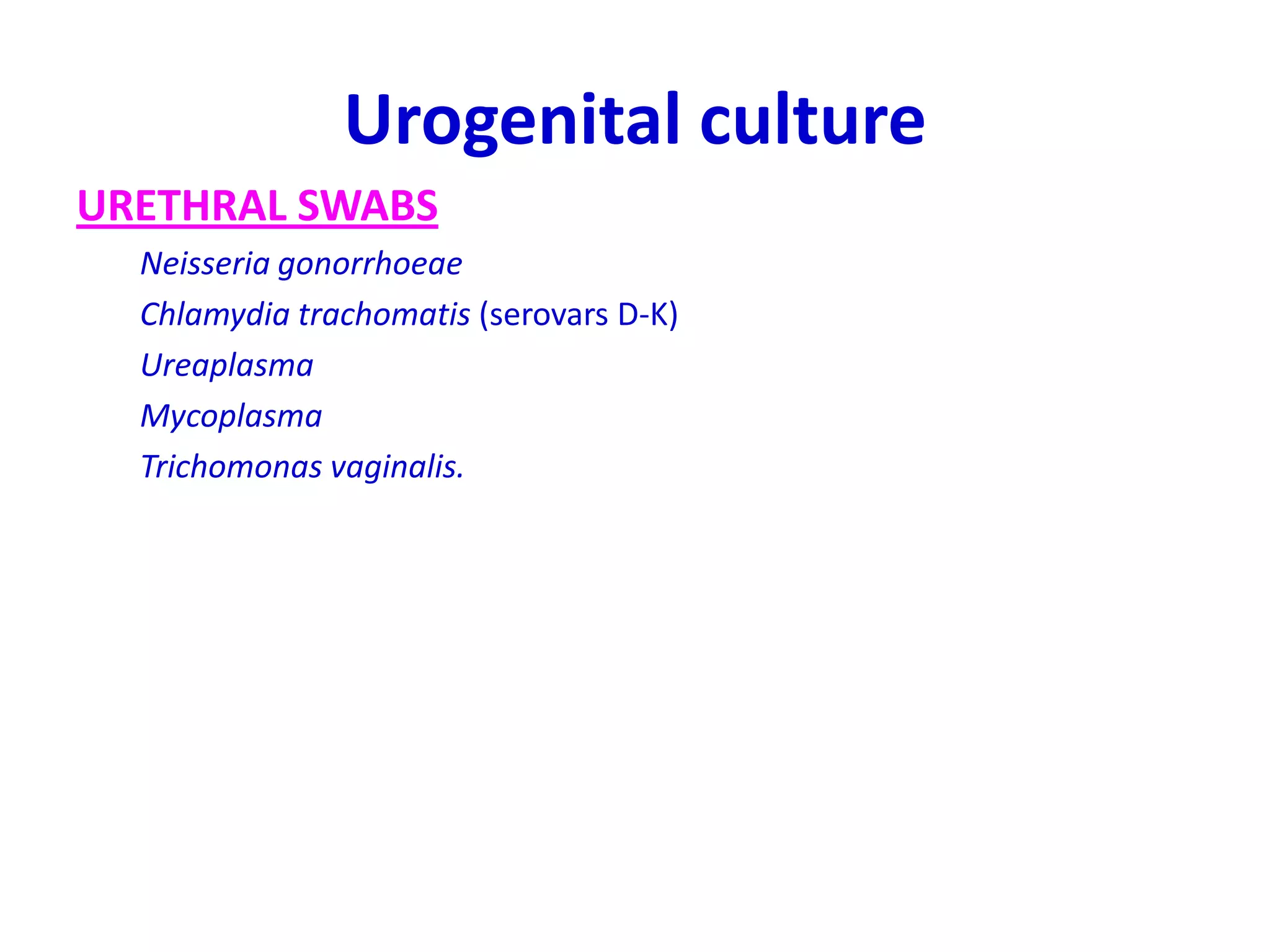
This document provides information about various components that may be analyzed in urinalysis, urine sediment, and other body fluids and samples. It discusses normal ranges and clinical significance of findings for numerous tests, including urinalysis dipstick components, microscopic examination of urine sediment, cerebrospinal fluid analysis, culture of various clinical samples, and numerous serological tests. The document is intended as a reference for clinicians on interpreting results from these diagnostic tests.














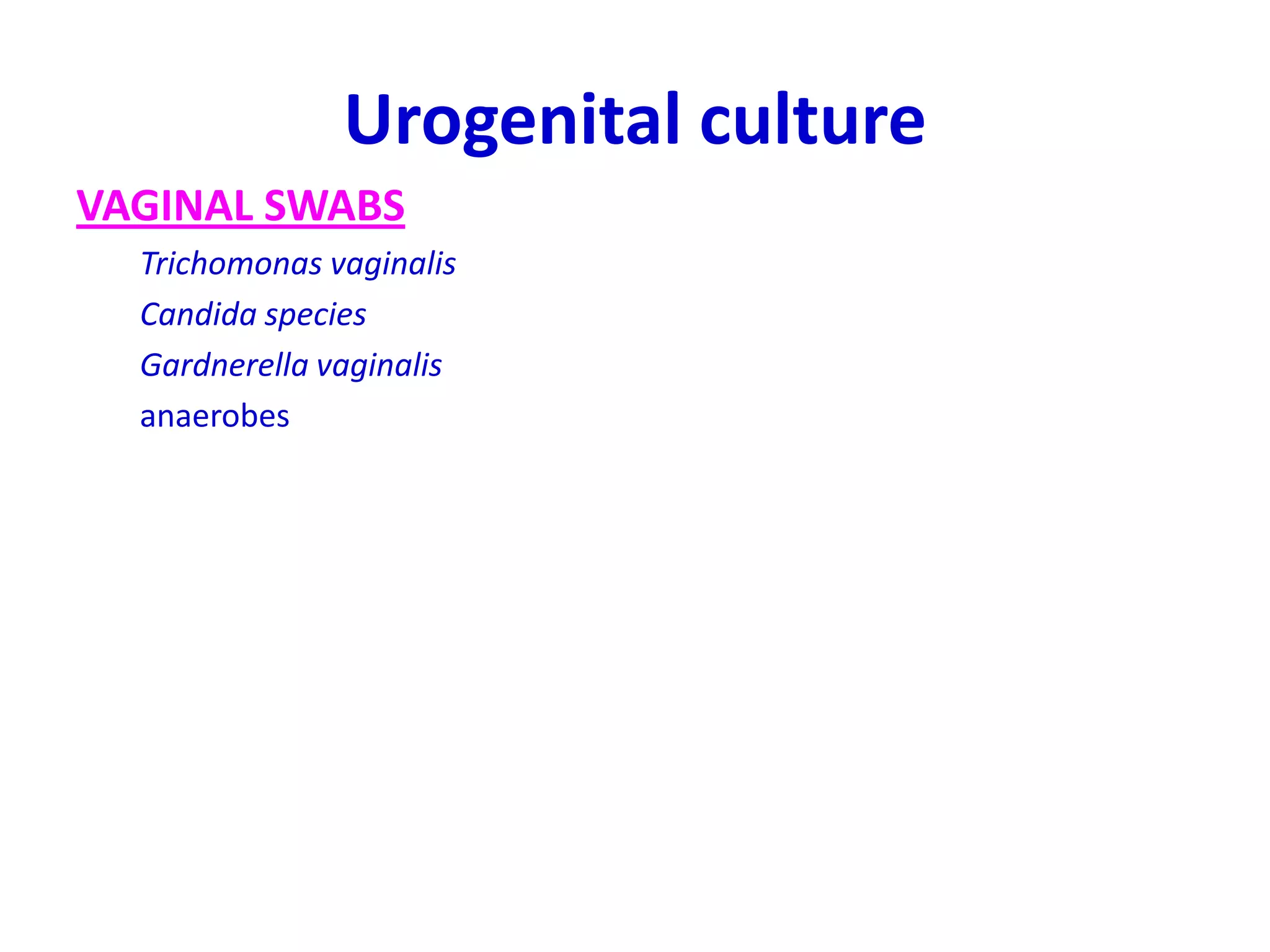





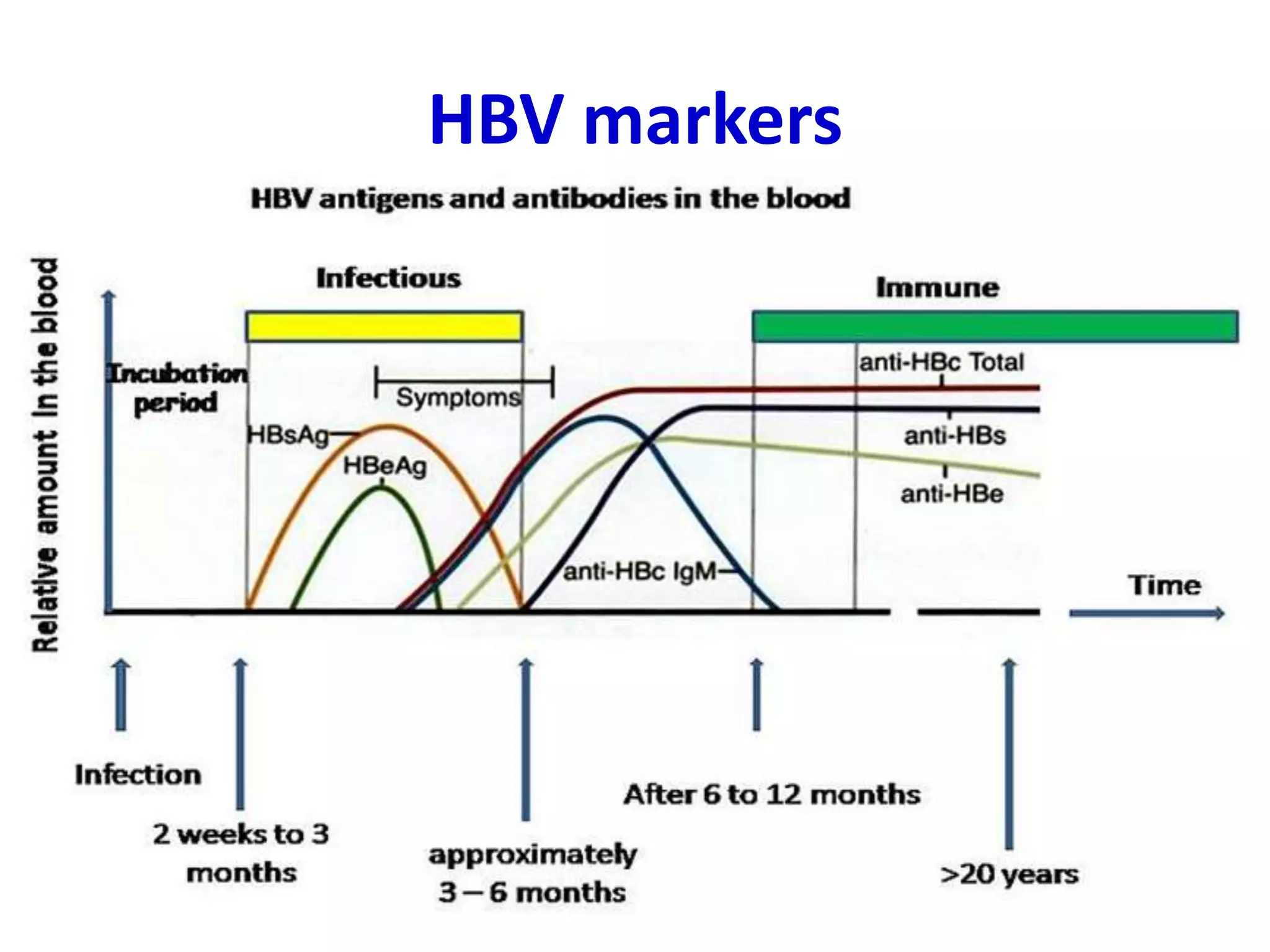
![Hepatitis B surface antigen (HBsAg)
In hepatitis B virus infection
HBsAg is
• detectable 2-5 weeks before
onset of symptoms
• peaks at the time of onset of
clinical illness.
• persists for 1-5 months
• Declining with resolution of
clinical symptoms.
Positive in:
• Acute hepatitis B
• chronic hepatitis B (persistence
of HBsAg for >6 months, positive
HBcAb [total])
• HBsAg positive carriers.
.](https://image.slidesharecdn.com/labinvestig-140520081936-phpapp01/75/Lab-investig-33-2048.jpg)