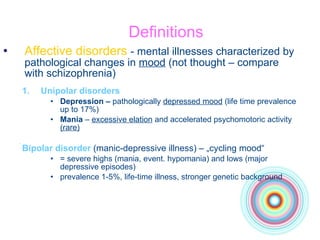
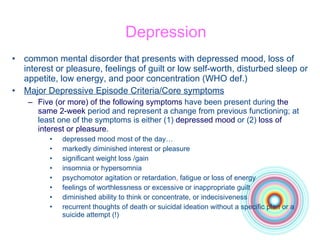
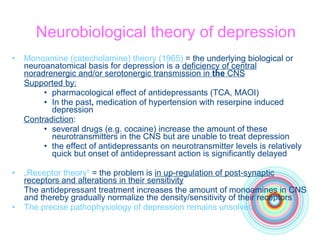
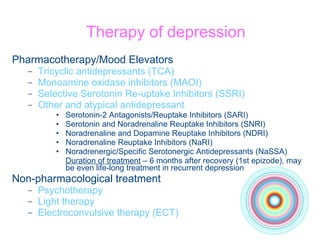
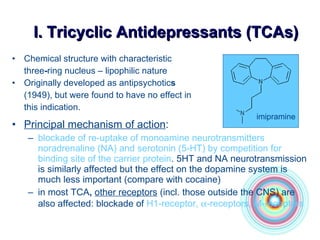
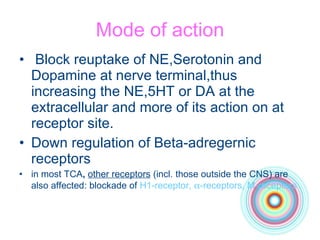
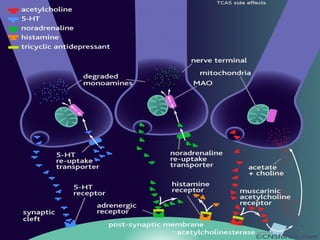
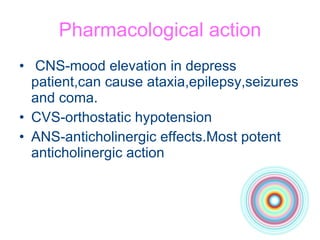
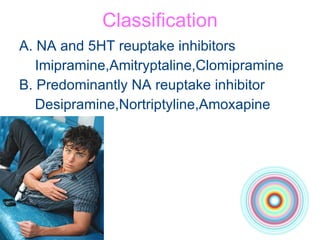
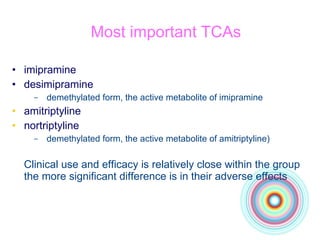
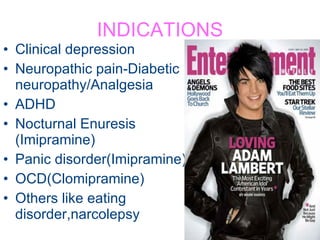
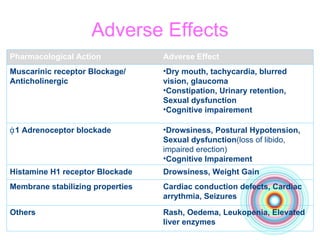
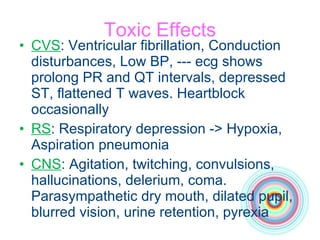
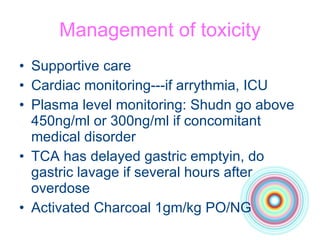
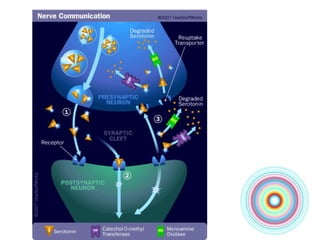
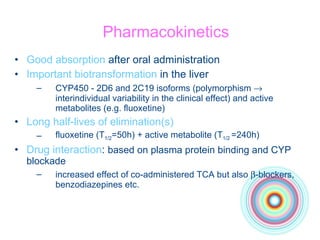
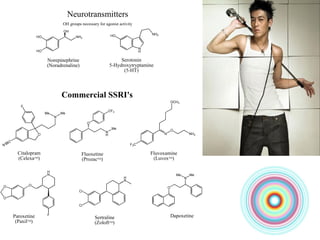
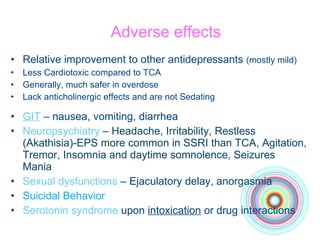
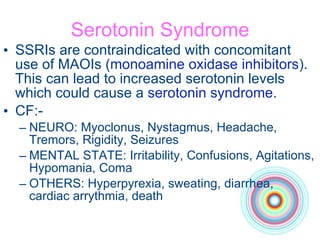
The document provides an overview of various antidepressants including tricyclic antidepressants (TCA), selective serotonin reuptake inhibitors (SSRI), and their effects, mechanisms, pharmacokinetics, and adverse effects. It discusses the classification of antidepressants, their clinical uses, particularly in treating mood disorders like depression and bipolar disorder, and the importance of proper dosage and monitoring for efficacy and side effects. Additionally, it highlights the neurobiological theories of depression, the varieties of treatment available, and warns against potential toxicity and drug interactions.