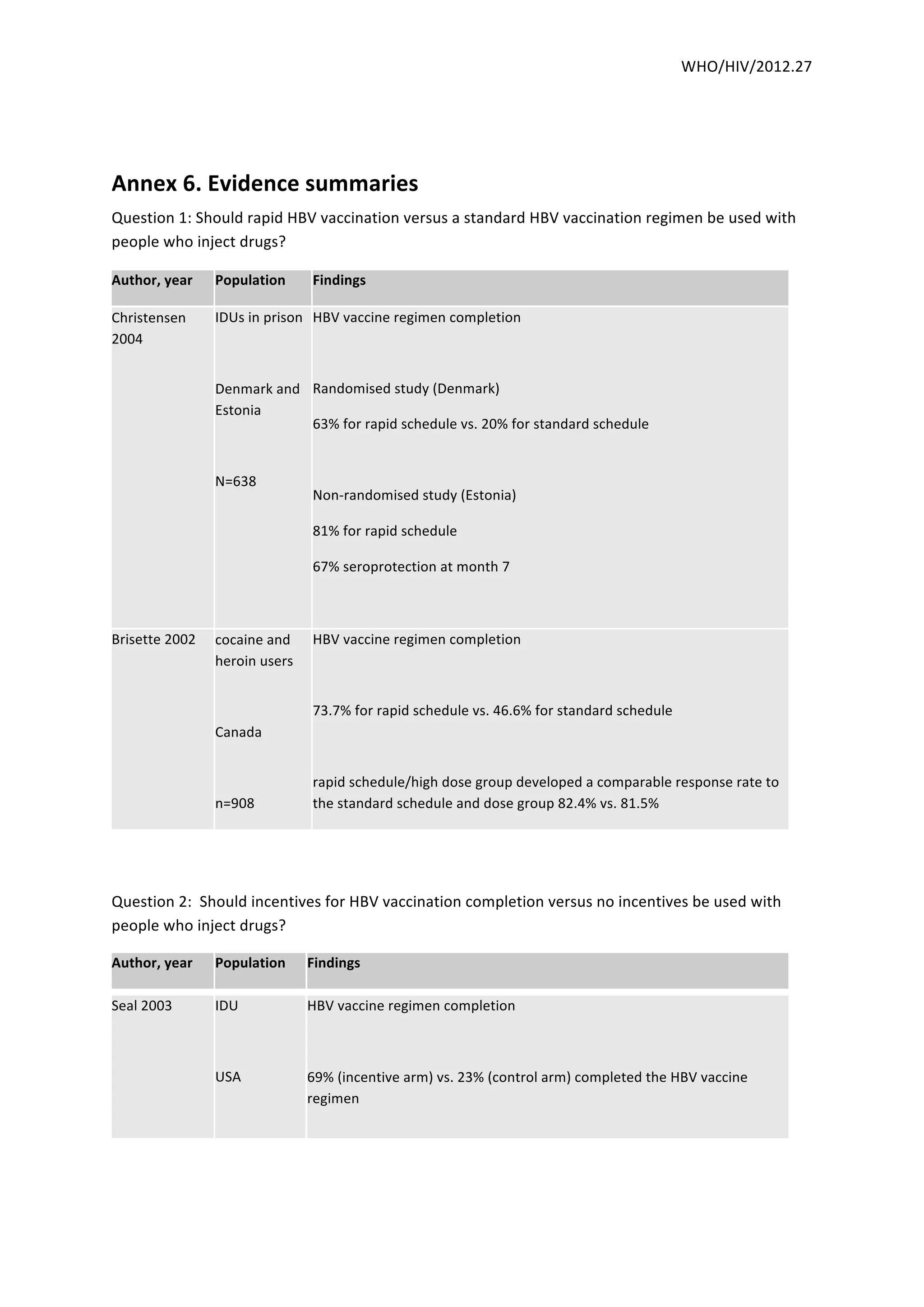
Rapid HBV vaccination schedules were more effective at completing the vaccination regimen compared to standard schedules in studies of people who inject drugs in prison in Denmark and Estonia. The use of incentives for HBV vaccination also improved completion rates compared to no incentives in US studies. Providing low dead space syringes rather than high dead space syringes was associated with lower rates of HIV and HCV in a Hungarian study, while a US study found increased risks of HIV and HCV with sharing or using high dead space syringes. Psychosocial interventions showed some benefits over no interventions, such as reduced HCV incidence and increased safer behaviors, though one US study found no difference in HCV seroconversion between a motivational intervention and assessment



![5
Question
5:
Should
peer
education
and
mentoring
versus
no
peer
education
and
mentoring
be
used
in
people
who
inject
drugs?
Author,
year
Population
Findings
Garfein
2007
IDU
USA
N=
853
29%
greater
decline
in
overall
injection
risk
among
intervention
group
6
months
post-‐intervention
relative
to
the
control
[proportional
OR
0.71;
95%
CI:
0.52,
0.97],
and
a
76%
decrease
compared
with
baseline.
Decreases
were
also
observed
for
sexual
risk
behaviors,
but
they
did
not
differ
by
trial
arm.
Overall
HCV
infection
incidence
(18.4/100
person-‐years)
did
not
differ
significantly
across
trial
arms
(RR
1.15;
95%
CL
0.72,
1.82).
No
HIV
seroconversions
were
observed.
Latka
2008
IDU
USA
N=418
Compared
with
the
control
group,
intervention-‐group
participants
were
less
likely
to
report
distributive
risk
behaviors
at
3
months
(OR=0.46;
95%
CI:
0.27,
0.79)
and
6
months
(OR=0.51;
95%
CI:0.31,
0.83),
a
26%
relative
risk
reduction,
but
were
no
more
likely
to
cite
their
HCV-‐positive
status
as
a
reason
for
refraining
from
syringe
lending.
Effects
were
strongest
among
intervention-‐group
participants
who
had
known
their
HCVpositive
status
for
at
least
6
months.
Peer
mentoring
and
self-‐efficacy
were
significantly
increased
among
intervention-‐group
participants,
and
intervention
effects
were
mediated
through
improved
self-‐efficacy.](https://image.slidesharecdn.com/whohiv2012-140612104825-phpapp01/85/Who-hiv-2012-27_eng-5-320.jpg)
